Abstract
The purpose of this study was to examine how aging and sex impacted scores on the Eating Assessment Tool-10 in a large sample of healthy, non-dysphagic adults. Differences in Eating Assessment Tool-10 total normal (< 3) and abnormal (≥ 3) scores were examined across four age categories (21–39 years, 40–59 years, 60–79 years, 80 years and older) and between sexes. The mean (± SD) Eating Assessment Tool-10 total score for this healthy cohort of 167 individuals was 0.6 (± 1.6), with the majority of participants (75%) earning a score of zero. No significant differences were found in Eating Assessment Tool-10 total scores across age categories (p = .53) or between sexes (p = .79). Post-hoc analyses further explored relationships between Eating Assessment Tool-10 total scores and swallow performance measures as observed during videofluoroscopy. All participants (n = 15) scoring 3 and greater on the Eating Assessment Tool-10 passed an aspiration screen (i.e., 3-ounce water swallow challenge). Nine participants scoring less than 3 and failing the aspiration screen were not observed to have airway invasion as measured by the Penetration-Aspiration Scale during videofluoroscopy. A significant relationship was not observed between Eating Assessment Tool-10 total scores and highest Penetration-Aspiration Scale score. Eating Assessment Tool-10 total scores reported in the current study for patients with gastroesophageal reflux disease were significantly lower (p < .001) than total scores reported in the Eating Assessment Tool-10 validation study by Belafsky et al. (2008). In summary, aging or sex effects did not appear to impact self-report of dysphagia-related symptoms as measured by the Eating Assessment Tool-10. The Eating Assessment Tool-10, therefore, may not demonstrate the sensitivity needed to capture sub-clinical changes of the aging swallowing mechanism.
Keywords: EATING ASSESSMENT TOOL-10, DYSPHAGIA, SWALLOWING, HEALTHY, ADULTS
Abstract
L’objectif de cette étude était d’examiner l’impact du vieillissement et du sexe sur les scores du Eating Assessment Tool-10, et ce, auprès d’un grand échantillon d’adultes en santé qui n’ont pas de dysphagie. Les scores totaux normaux (< 3) et anormaux (≥ 3) obtenus à l’Eating Assessment Tool-10 ont été examinés au sein de quatre catégories d’âge (21–39 ans, 40–59 ans, 60–79 ans, 80 ans et plus), ainsi qu’en fonction du sexe. La moyenne (± ÉT) des scores totaux était de 0,6 (± 1,6) pour cette cohorte de 167 individus en santé et une majorité d’entre eux (75%) ont obtenu un score de zéro. Aucune différence significative n’a été trouvée entre les catégories d’âge (p = 0,53) ou en fonction du sexe (p = 0,79). Des analyses post-hoc ont exploré plus en détail la relation entre les scores totaux du Eating Assessment Tool-10 et des mesures de performance de la déglutition recueillies lors d’une vidéofluoroscopie. Aucune aspiration n’a été dépistée (à l’aide d’une épreuve demandant d’avaler 3 onces d’eau) chez les 15 participants ayant obtenu un score égal ou plus grand que 3 à l’Eating Assessment Tool-10. Des aspirations ont été dépistées (à l’aide d’une épreuve demandant d’avaler 3 onces d’eau) chez neuf des participants ayant obtenu un score inférieur à 3 à l’Eating Assessment Tool-10. Néanmoins, aucun matériel n’est entré dans leurs voies respiratoires, si l’on se fie aux résultats obtenus avec la Penetration-Aspiration Scale lors de la vidéofluoroscopie. Aucune relation significative n’a été observée entre les scores totaux obtenus à l’Eating Assessment Tool-10 et les scores plus élevés obtenus à la Penetration-Aspiration Scale. Les scores totaux obtenus à l’Eating Assessment Tool-10 par les patients de la présente étude ayant du reflux gastro-oesophagien étaient significativement inférieurs (p < 0,001) à ceux obtenus dans l’étude de validation de Belafsky et al. (2008). En résumé, l’âge et le sexe ne semblent pas influencer les symptômes de dysphagie rapportés par les patients et mesurés par l’Eating Assessment Tool-10. Par conséquent, l’Eating Assessment Tool-10 ne semble pas avoir la sensibilité nécessaire pour identifier les changements subcliniques se produisant en cours de vieillissement au niveau du mécanisme de la déglutition.
The Eating Assessment Tool (EAT-10) was motivated by a need for a clinically practical dysphagia assessment of dysphagia symptom severity, quality of life, and treatment efficacy that can be rapidly administered and easily scored in a clinical setting (Belafsky et al., 2008). Items include symptom-related information such as unintentional weight loss, effort or pain during swallowing, and coughing during eating. Each item on the 10-item instrument is arranged in a 5-point Likert scale (0 = No problem, 4 = Severe problem).
During the validation study by Belafsky et al. in 2008, the EAT-10 was administered to 235 individuals (patient cohort) with known voice and swallowing disorders and 100 healthy, non-dysphagic individuals (normal cohort). Male participants comprised 53% of the normal cohort, and the mean (± SD) age was 48 ± 16 years. The normal cohort included persons without history of voice, swallowing, reflux, or other medical disorders known to influence swallowing function (Belafsky et al., 2008). The mean EAT-10 score for the normal cohort was 0.40 ± 1.01, which produced the upper normal limit score of 2.41 (mean + 2 SD). These normative data suggest that an EAT-10 score of ≥ 3 is abnormal. The EAT-10 scores of patients across a variety of medical diagnostic categories (e.g., head and neck cancer, reflux disease) had significantly higher EAT-10 scores compared with the healthy group (p < .001). The validation study, however, did not explore if aging affects EAT-10 total scores in healthy, community-dwelling adults.
Previous evidence estimates the prevalence of dysphagia in older, community-dwelling individuals at a rate of 11% (Holland et al., 2011). Increasing rates of swallowing impairments are expected as the aging population in the United States rapidly grows. Physiologic changes to the swallowing mechanism resulting from natural aging have been well documented, including loss of dentition, altered salivary flow, muscular atrophy and infiltration of fatty tissue, and reduced mobility and strength of upper aerodigestive tract structures relevant to swallowing (Baum & Bodner, 1983; Ekberg & Feinberg, 1991; Mulheren et al., 2018; Robbins, Hamilton, Lof, & Kempster, 1992; Yoshikawa et al., 2005). These age-related changes in swallowing function known as presbyphagia may impact health status and quality of life as an individual continues to age. Although the EAT-10 was validated using a healthy cohort, potential aging effects on total scores were not considered. Understanding how aging can impact swallowing function can help differentiate typical from atypical changes.
The primary purpose of this study was to describe performance on the EAT-10 in a large sample of healthy, non-dysphagic and non-reflux community-dwelling adults. To achieve this aim, we explored differences in EAT-10 total scores across four age categories (21–39 years, 40–59 years, 60–79 years, and 80 years and older) and between sexes. We then compared our healthy cohort results to findings reported in the original validation study by Belafsky et al. (2008). We did not anticipate any sex differences but expected higher EAT-10 total scores in older adults relative to their younger counterparts, although anticipated the average EAT-10 total score would be consistent with the previous report by Belafsky et al. During post-hoc analysis, we further explored associations between EAT-10 total scores and additional swallowing measures, including pass/fail outcomes on an aspiration screening measure and observation of bolus airway invasion during videofluoroscopy. We hypothesized that higher EAT-10 scores (3 and greater) would have higher rates of fails and occurrences of bolus airway invasion.
Method
Participants
Participants for the current study were derived from a normative database consisting of 195 healthy participants. All participants were required to provide informed consent prior to participation in study procedures. This study received approval by the Institutional Review Board affiliated with the university (Pro00011566).
Our current sample included community-dwelling adult volunteers without a current or previous diagnosis of dysphagia, gastroesophageal reflux disease, neurological insult/disease (e.g., stroke, Parkinson’s disease), pulmonary disease (e.g., chronic obstructive pulmonary disease), head and neck cancer, anterior neck surgery (e.g., thyroid surgery, anterior spinal surgery), or other medical conditions known to influence swallowing function per self-report during completion of a demographic and clinical questionnaire as part of determining study eligibility. All study participants reported eating a full regular diet with all liquids without restrictions (Functional Oral Intake Scale Level 7; Crary, Carnaby Mann, & Groher, 2005). Further, participants were judged by study personnel to have adequate cognition to participate in study procedures and/or pass a cognitive screen (Montreal Cognitive Assessment; Nasreddine et al., 2005). Participants were recruited using study flyers, word-of-mouth, and community outreach opportunities (e.g., booth at local event).
Procedures
Participants completed the EAT-10 as part of a study protocol investigating the effects of typical aging on oropharyngeal swallowing function. Study procedures in addition to completion of the EAT-10 included completion of a 3-ounce water swallowing challenge (DePippo, Holas, & Reding, 1992; Suiter & Leder, 2008) and videofluoroscopic examination in accordance to the Modified Barium Swallow Impairment Profile protocol (Martin-Harris et al., 2008). Modified Barium Swallow Impairment Profile scores and Penetration-Aspiration Scale (PAS) scores were collected from videofluoroscopic studies obtained under continuous fluoroscopy and recorded at 30 frames per second. All study procedures were completed in an adult radiology suite during a one-time study visit. Participants were compensated for time and travel.
Analysis
EAT-10 scores were tabulated by sex and age category. In addition, scores were categorized in a binary manner as normal (0–2) or abnormal (≥ 3). Fisher’s exact test was used to test for associations between the binary score and sex and age categories. Logistic regression was used to test for interaction effects between age and sex using the binary score as the outcome variable. Due to the small sample size for the 80+ year age category, it was combined with the 60–79 age category in the logistic regression model. An alpha level of .05 was used for this analysis to evaluate the significance for all comparisons.
Results
A total of 167 (93 women) participants were included in the analysis from the normative database. Mean age (± SD) in the current participant sample was 46 (± 17) years. Further demographic information is provided in Table 1. The mean (± SD) EAT-10 total score was 0.6 ± 1.6, with a range from 0 to 11. The majority of participants in the current study scored a 0 on the EAT-10 (n = 126, 75.4%; Table 2). Fifteen participants (9.0%) earned an w score (i.e., EAT-10 total score of 3 or more). The rate of abnormal scores (≥ 3) was 2% higher in women vs. men (90% vs. 92%), while the rate between age categories differed by no more than 11% observed in the youngest age category (21–39 years) compared to the oldest (80 years and older; 6% vs. 17%). However, there was not a significant difference in binary EAT-10 total scores (< 3, ≥ 3) across age categories (p = .53) or between sexes (p = .79). No interaction was found between the age category and sex variables in the logistic regression model (p = .65).
Table 1.
Participant Demographics
| Variable | Total (N = 167) |
|---|---|
| Age (years) | |
| Mean ± SD | 45.7 ± 17.2 |
| Range | 21–89 |
| Sex | |
| Female | 93 (55.7) |
| Male | 74 (44.3) |
| Race | |
| White/Caucasian | 121 (72.5) |
| Black/African American | 41 (24.6) |
| Asian | 1 (0.6) |
| More than 1 race | 3 (1.8) |
| Unknown/not reported | 1 (0.6) |
| Ethnicity | |
| Non-Hispanic/Non-Latino | 163 (97.6) |
| Hispanic/Latino | 4 (2.4) |
| Age category | |
| 21–39 years (n = 66) | 66 (39.5) |
| 40–59 years (n = 57) | 57 (34.1) |
| 60–79 years (n = 38) | 38 (22.8) |
| 80 years and older (n = 6) | 6 (3.6) |
Note. Data presented in frequencies (percentages) unless otherwise reported.
Table 2.
EAT-10 Total Scores Between Sexes and Across Age Categories
| 0 | 126 (75) | 58 (78) | 68 (73) | 56 (79) | 42 (74) | 28 (74) | 4 (67) |
| 1 | 15 (9) | 8 (11) | 7 (8) | 6 (9) | 6 (11) | 3 (8) | 0 (0) |
| 2 | 11 (7) | 2 (3) | 9 (10) | 4 (6) | 3 (5) | 3 (8) | 1 (17) |
| 3 | 7 (4) | 3 (4) | 4 (4) | 3 (5) | 3 (5) | 1 (3) | 0 (0) |
| 4 | 5 (3) | 2 (3) | 3 (3) | 1 (2) | 2 (4) | 1 (3) | 1 (17) |
| 5 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 6 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 7 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 8 | 1 (<1) | 1 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (3) | 0 (0) |
| 9 | 1 (<1) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 1 (3) | 0 (0) |
| 10 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 11 | 1 (<1) | 0 (0) | 1 (1) | 0 (0) | 1 (2) | 0 (0) | 0 (0) |
| Grouped | |||||||
| 0–2 | 152 (91) | 68 (92) | 84 (90) | 66 (94) | 51 (89) | 34 (89) | 5 (83) |
| 3–11 | 15 (9) | 6 (8) | 9 (10) | 4 (6) | 6 (11) | 4 (11) | 1 (17) |
Note. Data presented in frequencies (percentages) unless otherwise reported. EAT-10 = Eating Assessment Tool-10.
Post-Hoc Analysis
To further investigate study findings, additional data were extracted from the normative database to determine associations between EAT-10 total scores and performance on additional swallowing measures, including the 3-ounce water swallow challenge (Suiter & Leder, 2008), bolus airway invasion as measured by the PAS (Rosenbek, Robbins, Roecker, Coyle, & Wood, 1996), and participants who self-reported a diagnosis of gastroesophageal reflux disease. For the 15 participants with an abnormal EAT-10 total score of 3 or greater, each participant passed a 3-ounce water swallow challenge. Nine participants demonstrating EAT-10 total scores < 3 failed the 3-ounce water swallow challenge, including two participants with change in vocal quality and seven with throat clear/cough after administration. Despite the failed performance on the 3-ounce water swallow challenge, each of the nine participants received PAS scores of 1 across swallowing tasks observed under videofluoroscopy.
Three participants were observed during videofluoroscopy to penetrate (PAS scores of 3, 3, and 4, respectively) during self-administered sequential swallowing thin and nectar-thickened liquid tasks (Figure 1a). The remaining 12 participants with scores of 3 or greater were observed to have PAS scores < 3. Twelve penetration and three aspiration events were observed in participants earning an EAT-10 total score of < 3 (Figure 1b). Spearman’s rank correlation failed, however, to reveal a significant relationship between EAT-10 total scores and worst (highest) PAS score (rs = −.04, p = .61).
Figure 1A-B.
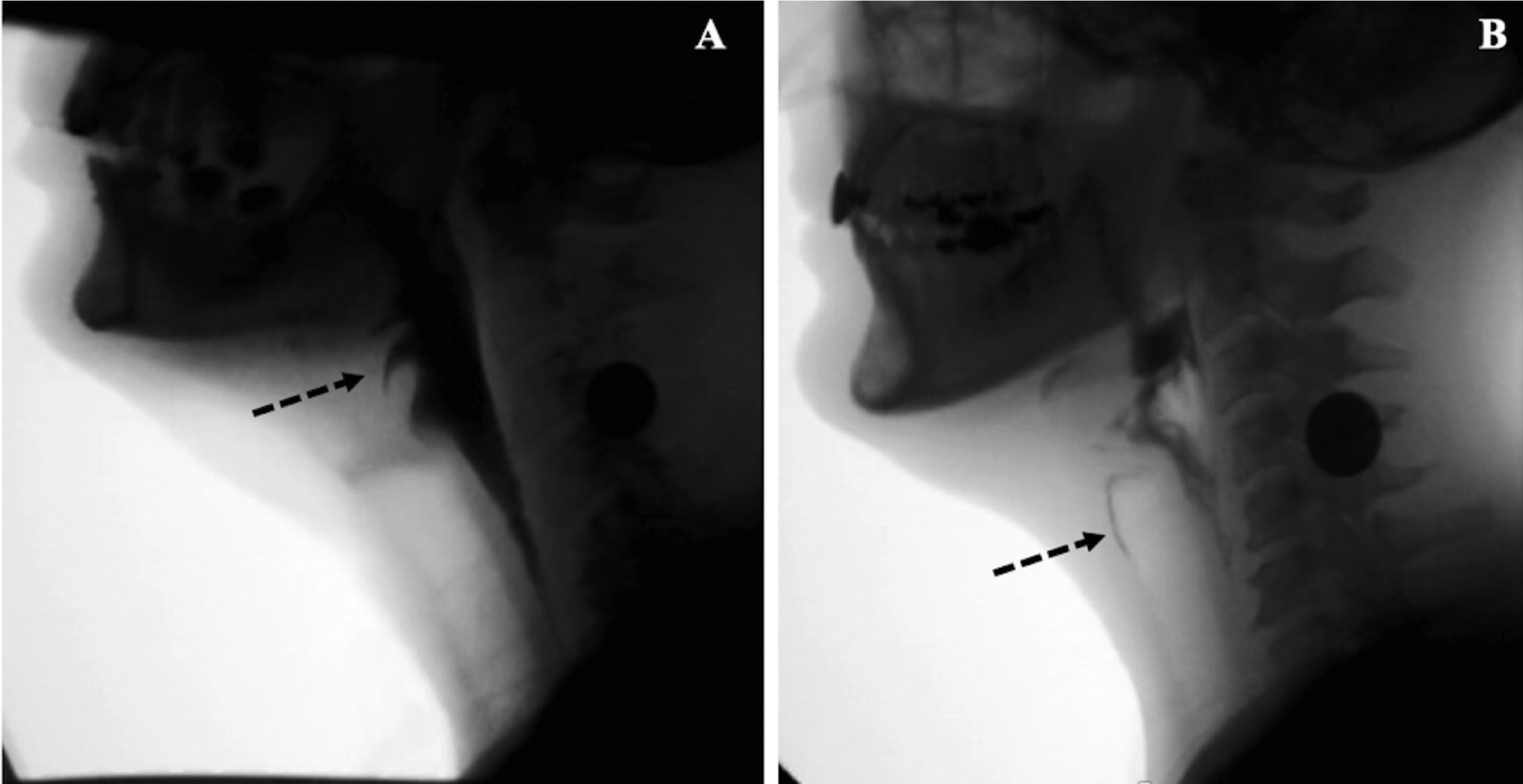
A) 66-year-old male participant with an Eating Assessment Tool-10 (EAT-10) total score of 8 demonstrating penetration (Penetration-Aspiration Scale [PAS] score of 3) during thin liquid sequential swallowing task. B) 48-year-old female participant with an EAT-10 total score of 0 and aspiration (PAS score of 7) during teaspoon thin liquid swallowing task. All remaining swallowing tasks received a PAS score of 1.
To investigate potential of reflux on EAT-10 scores, participants who self-reported a diagnosis of gastroesophageal reflux disease (n = 28, 16 women) were also extracted from the normative database. The mean age (± SD) in the current participant sample who self-reported reflux was 55 (± 16) years. These scores were compared with findings from the reflux sample (n = 66) reported by Belafsky et al. (2008), although further demographic information was unavailable. Participants in the current cohort who self-reported a history of reflux had a higher average score than participants who did not report reflux (1.9 ± 3.9 vs. 0.6 ± 1.6). However, EAT-10 total scores for participants who reported reflux in the current study had significantly lower scores than reported in the Belafsky et al. study (1.9 ± 3.9 vs. 11.7 ± 3.9; p < .001).
Discussion
The purpose of this study was to describe performance on the EAT-10 in a large sample of healthy, non-dysphagic and non-reflux community-dwelling adults and explore the potential influence of age and sex on total scores. The majority of individuals earned a score of 0 (75%), although variability was observed (range 0–11). However, study results failed to find age- or sex-related effects on EAT-10 total scores.
Two items from the EAT-10 that contributed to the highest percentage of participants reporting a score greater than 0 included “swallowing pills takes extra effort” (Question 5) and “when I swallow, food sticks in my throat” (Question 8). When examining previous literature, a population survey reported 40% of adults reported difficulty with swallowing pills (Harris Interactive Survey, n.d., as cited in Fields, Go, & Schulze, 2015), with similar findings reported in a study by Fields et al. (2015). Larger pills and pills without a coating were among chief complaints of adults (Harris Interactive Survey, n.d., as cited in Fields et al., 2015), although a small subset of their study population also complained of difficulty with swallowing solids. Our findings support previous studies demonstrating community-dwelling adults experience difficulty with taking pills. However, whether the reported difficulty in swallowing pills is due to fear/anxiety or true pathologic impairment has not been elucidated in previous studies. Further, the potential relationship between difficulty taking pills and solid food dysphagia is interesting and worth exploring.
Another possibility for higher scores reported for Questions 5 and 8 may relate to the presence of dry mouth or hyposalivation contributing to perceived increased effort for pills and globus sensation for solids. Polypharmacy is common among older adults, with the majority consuming at least one medication causing salivary hypofunction (Turner & Ship, 2007). Further contributing factors include systemic diseases and their treatments and other medical conditions, including dehydration. While our stringent criteria excluded medical diseases that are often associated with dysphagia, it may not have been an exhaustive listing to include conditions that may contribute to a salivary disorder. When comparing rates of scores greater than zero across the age groups for these two EAT-10 questions, however, no discernable differences emerged for either question, suggesting that such self-reported difficulties were represented across the adult lifespan and may not exclusively result from aging.
A critical outcome of swallowing dysfunction is entry of a bolus into the airway. Airway invasion in healthy individuals has been previously documented, particularly in healthy older individuals (Butler, Stuart, Markley, Feng, & Kritchevsky, 2018; Butler, Stuart, Markley, & Rees, 2009; Garand et al., 2019; Robbins, Coyle, Rosenbek, Roecker, & Wood, 1999). This study failed to find a significant relationship, however, between worst (highest) PAS scores and EAT-10 total scores. Further, participants without airway invasion observed during videofluoroscopy in the current study earned a median score of 3 (range 1–11), which would be considered an “abnormal” score according to the validation study by Belafsky et al. (2008). Thus, these findings suggest that airway invasion events may not impact a healthy individual’s perception of swallowing difficulty and that a perceived impaired perception of swallowing function may not translate to actual airway invasion.
When examining the influence of reflux on perceived swallowing difficulty as measured by EAT-10, the current study sample reported less perceived difficulty than patients with reflux as reported by Belafsky et al. (2008). One possible explanation for the differences in EAT-10 total scores reflux findings between participants with reflux in the validation study (Belafsky et al., 2008) and our non-dysphagic cohort who self-reported reflux is the participants in the validation study were undergoing treatment for voice and swallowing disorders. Therefore, these participants may have been experiencing reflux that manifested itself in primary voice or swallowing symptoms. Further, reflux was self-reported in this study, so it remains unknown who provided the diagnosis of reflux and what assessment (if any) was completed to confirm the diagnosis.
When Belafsky et al. (2008) applied mean plus 2 SD to yield the upper limit of normal in their study, their data supported the use of ≥ 3 score as abnormal. The mean (± SD) age of the normal cohort (n = 100) reported by Belafsky et al. was similar to that in the current cohort (48 ± 16 years vs. 46 ± 17 years, respectively). Sex distribution was also similar, with men comprising 53% and 44% of the sample in Belfasky et al. and the current study, respectively. The mean (± SD) EAT-10 total score for the current study was 0.6 (± 1.6). Thus, when using the mean plus 2 SD formula as applied in the Belafsky et al. study, the current data supports the use of a score of 4 or higher (i.e., 0.6 + 3.2 = 3.8) to be considered abnormal. This one-point difference is likely attributed to how we sampled participants since in the current study, we stratified by age category while Belafsky et al. did not. The validation study by Belafsky et al. also did not consider the implications of age on scores. Further, Rofes, Arreola, Mukherjee, and Clavé (2014) found increased sensitivity of identification of oropharyngeal dysphagia observed during videofluoroscopy when reducing the cutoff score to 2 to reduce rates of false negatives (i.e., patients with dysphagia misclassified as healthy). The sample size in the Rofes et al. study only included 14 healthy participants (8 men, 6 women), with all participants earning a total score of 0 on the EAT-10. Participants in the healthy cohort in the Rofes et al. study were younger compared to the current cohort (30.5 ± 6.1 compared to 48 ± 16 in the current study). Unfortunately, age was not a variable of interest in the Rofes et al. study.
Limitations
A primary limitation of our study includes the low number of participants in the oldest age category. When these participants were collapsed in the next youngest age category (60–79 years), differences across age categories remained non-significant. Further, a study by Cordier et al. (2017) using Rasch analysis revealed item redundancy, lack of easy/difficult items, and floor effect in the EAT-10; however, this tool is commonly reported in the literature and translated into other languages. Lastly, our healthy cohort may have occult impairments that had yet to be diagnosed, and thus, may have influenced severity of symptoms reported. Despite these limitations, this study further contributes to understanding typical swallowing in aging adults in helping to delineate typical or “normal” from true pathologic impairment. Although, overall EAT-10 scores were low in our study sample, there was a variability in scores (range 0–11). However, we failed to find any aging effects on EAT-10 scores, as well as failed to find sex effects or a significant relationship between EAT-10 total scores and PAS scores. For individuals who report perceived difficulty on EAT-10 scores, other considerations should be evaluated (e.g., influence of medications) especially in light of instrumentation revealing functional swallowing physiology.
Future Research
Future studies that include concurrent imaging (i.e., videofluoroscopy or fiberoptic endoscopic evaluation of swallowing function) with the EAT-10 tool will provide increased information regarding the sensitivity and specificity of the EAT-10 with instrumental findings of swallowing function, as well as investigate potential aging influence on EAT-10 total scores in older adults (80 years and older).
Conclusions
This study described EAT-10 total scores in a large sample of healthy, non-dysphagic and non-reflux community-dwelling adults. In summary, the majority of participants earned a score of 0, although variability in scores was observed. Investigation of sex and age-related effects did not reveal significant differences in EAT-10 total scores. Post-hoc analyses also failed to find a significant relationship between EAT-10 total scores and PAS score. Findings suggest that the subacute changes in the upper aerodigestive tract occurring during healthy aging do not necessarily contribute to changes in perceived difficulty of swallowing functions. Further, perceived impairment of swallowing function as captured by the EAT-10 may not translate to occurrence of bolus airway invasion observed on videofluoroscopy.
Acknowledgments
This work was supported by the Veterans Affairs (RR&D 1IK1RX001628-01A, PI: Garand), the National Institutes of Health (NIH/NCATS TL1R000061, PI: Brady, Project PI: [Focht] Garand, and NIH/NIDCD 1K24DC12801 [PI: Martin-Harris]), and the American Speech-Language-Hearing Foundation (PI: [Focht] Garand).
Footnotes
Disclosures
No conflicts of interest, financial or otherwise, are declared by the authors.
Contributor Information
Kendrea L. (Focht) Garand, University of South Alabama, Mobile, AL, USA
Elizabeth G. Hill, Medical University of South Carolina, Charleston, SC, USA
Kent Armeson, Medical University of South Carolina, Charleston, SC, USA.
Bonnie Martin-Harris, Northwestern University, Evanston, IL, USA.
References
- Baum BJ, & Bodner L (1983). Aging and oral motor function: Evidence for altered performance among older persons. Journal of Dental Research, 62, 2–6. doi: 10.1177/00220345830620010401 [DOI] [PubMed] [Google Scholar]
- Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, & Leonard RJ (2008). Validity and reliability of the Eating Assessment Tool (EAT-10). Annals of Otolology, Rhinology, & Laryngology, 117, 919–924. doi: 10.1177/000348940811701210 [DOI] [PubMed] [Google Scholar]
- Butler SG, Stuart A, Markley L, Feng X, & Kritchevsky SB (2018). Aspiration as a function of age, sex, liquid type, bolus volume, and bolus delivery across the healthy adult life span. Annals of Otolology, Rhinology, and Laryngology, 127, 21–32. doi: 10.1177/0003489417742161 [DOI] [PubMed] [Google Scholar]
- Butler SG, Stuart A, Markley L, & Rees C (2009). Penetration and aspiration in healthy older adults as assessed during endoscopic evaluation of swallowing. Annals of Otology, Rhinology, & Laryngology, 118, 190–198. doi: 10.1177/000348940911800306 [DOI] [PubMed] [Google Scholar]
- Cordier R, Joosten A, Clavé P, Schindler A, Bülow M, Demir N, … Speyer R (2017). Evaluating the psychometric properties of the Eating Assessment Tool (EAT-10) using Rasch analysis. Dysphagia, 32, 250–260. doi: 10.1007/s00455-016-9754-2 [DOI] [PubMed] [Google Scholar]
- Crary MA, Carnaby Mann GD, & Groher ME (2005). Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Archives of Physical Medicine and Rehabilitation, 86, 1516–1520. doi: 10.1016/j.apmr.2004.11.049 [DOI] [PubMed] [Google Scholar]
- DePippo KL, Holas MA, & Reding MJ (1992). Validation of the 3-oz water swallow test for aspiration following stroke. Archives of Neurology, 49, 1259–1261. doi: 10.1001/archneur.1992.00530360057018 [DOI] [PubMed] [Google Scholar]
- Ekberg O, & Feinberg MJ (1991). Altered swallowing function in elderly patients without dysphagia: Radiologic findings in 56 cases. American Journal of Roentgenology, 156, 1181–1184. doi: 10.2214/ajr/156.6.2028863 [DOI] [PubMed] [Google Scholar]
- Fields J, Go JT, & Schulze KS (2015). Pill properties that cause dysphagia and treatment failure. Current Therapeutic Research, 77, 79–82. doi: 10.1016/j.curtheres.2015.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garand KL, Hill EG, Amella E, Armeson K, Brown A, & Martin-Harris B (2019). Bolus airway invasion observed during videofluoroscopy in healthy, non-dysphagic community-dwelling adults. Annals of Otology, Rhinology, & Laryngology, 128, 426–432. doi: 10.1177/0003489419826141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland G, Jayasekeran V, Pendleton N, Horan M, Jones M, & Hamdy S (2011). Prevalence and symptom profiling of oropharyngeal dysphagia in a community dwelling of an elderly population: A self-reporting questionnaire survey. Diseases of the Esophagus, 24, 476–480. doi: 10.1111/j.1442-2050.2011.01182.x [DOI] [PubMed] [Google Scholar]
- Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, … Blair J (2008). MBS measurement tool for swallow impairment – MBSImp: Establishing a standard. Dysphagia, 23, 392–405. doi: 10.1007/s00455-008-9185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulheren RW, Azola AM, Kwiatkowski S, Karagiogos E, Humbert I, Palmer JB, & González-Fernández M (2018). Swallowing changes in community-dwelling older adults. Dysphagia, 33, 848–856. doi: 10.1007/s00455-018-9911-x [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, … Chertkow H (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53, 695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Robbins J, Coyle J, Rosenbek J, Roecker E, & Wood J (1999). Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia, 14, 228–232. doi: 10.1007/PL00009610 [DOI] [PubMed] [Google Scholar]
- Robbins J, Hamilton JW, Lof GL, & Kempster GB (1992). Oropharyngeal swallowing in normal adults of different ages. Gastroenterology, 103, 823–829. doi: 10.1016/0016-5085(92)90013-O [DOI] [PubMed] [Google Scholar]
- Rofes L, Arreola V, Mukherjee R, & Clavé P (2014). Sensitivity and specificity of the Eating Assessment Tool and the Volume-Viscosity Test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterology & Motility, 26, 1256–1265. doi: 10.1111/nmo.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, & Wood JL (1996). A penetration-aspiration scale. Dysphagia, 11, 93–98. doi: 10.1007/BF00417897 [DOI] [PubMed] [Google Scholar]
- Suiter DM, & Leder SB (2008). Clinical utility of the 3-ounce water swallow test. Dysphagia, 23, 244–250. doi: 10.1007/s00455-007-9127-y [DOI] [PubMed] [Google Scholar]
- Turner MD, & Ship JA (2007). Dry mouth and its effects on the oral health of elderly people. The Journal of American Dental Association, 138, 15S–20S. doi: 10.14219/jada.archive.2007.0358 [DOI] [PubMed] [Google Scholar]
- Yoshikawa M, Yoshida M, Nagasaki T, Tanimoto K, Tsuga K, Akagawa Y, & Komatsu T (2005). Aspects of swallowing in healthy dentage elderly persons older than 80 years. The Journals of Gerontology: Series A, 60, 506–509. doi: 10.1093/gerona/60.4.506 [DOI] [PubMed] [Google Scholar]


