Abstract
Urges for non-suicidal self-injury (NSSI) are important precursors to NSSI acts and may serve as a point of intervention. A close understanding of the phenomenology of NSSI urges and the contexts in which they occur is therefore warranted. We used ambulatory assessment to examine the environmental, interpersonal, and affective contexts of NSSI urges. We recruited 56 participants with borderline personality disorder who reported on urges and contexts for 21 days with six random daily prompts, resulting in 5,750 completed assessments. Twenty-two participants reported 160 NSSI urges. We provide extensive descriptive results characterizing the interaction partners, activities, and events participants reported in association with NSSI urges. Results from a logistic multilevel model using the full sample (testing associations between all contexts and urges simultaneously) revealed that urges were more likely to occur at higher levels of negative affect, when rejection was experienced, and later in the day. Urges were not associated with disagreements or feeling let down, being at home vs. away, being alone vs. in company, socializing vs. doing another activity, and it being a weekday vs. weekend. Additional growth curve analysis for negative affect using the subsample of 22 participants who reported urges showed that, over the course of urge days compared to non-urge days, negative affect increased prior to urges, peaked during the urge, and then decreased, approximating a quadratic curve. We conclude that urges occurred primarily in the context of negative affect and rejection, which is consistent with theories on intra- and interpersonal functions of NSSI.
Keywords: non-suicidal self-injury, urges, negative affect, ambulatory assessment, Borderline Personality Disorder
Introduction
Non-suicidal self-injury (NSSI), defined as the deliberate, self-inflicted damage of body tissue without suicidal intent (e.g. via cutting, burning, hitting), is present in approximately 6% of adults (Swannell, Martin, Page, Hasking, & St John, 2014), and around 2.7% of adults engage in repetitive NSSI (i.e., 5 or more times, lifetime Klonsky, 2011). Despite the absence of suicidal intent, NSSI is associated with an increased risk for suicide and accidental death (Ribeiro et al., 2016) and creates high costs for health care systems (Sinclair, Gray, Rivero-Arias, Saunders, & Hawton, 2011). There is a need to identify risk precursors to NSSI that may inform treatment strategies. NSSI urges, or the strong desire to engage in self-harm behavior, have been described as one such precursor (APA, 2013). Empirically, NSSI urges are frequent in samples prone to NSSI (Bresin, Carter, & Gordon, 2013; Zaki, Coifman, Rafaeli, Berenson, & Downey, 2013), predict the frequency of next-year NSSI acts (Turner, Baglole, Chapman, & Gratz, 2018) and NSSI frequency at discharge from treatment (Washburn, Juzwin, Styer, & Aldridge, 2010).
NSSI urges also temporally precede acts in daily life (Ammerman, Olino, Coccaro, & McCloskey, 2017; Andrewes, Hulbert, Cotton, Betts, & Chanen, 2017; Hughes et al., 2019; Kranzler et al., 2018; Turner et al., 2018), suggesting that urges could provide an important intervention point before acts occur. Existing treatments, such as Dialectical Behavior Therapy (DBT, Linehan, 1993) already recognize the importance of urges and teach patients how to track and tolerate urges until they decrease. Yet, despite the clinical value of tracking and targeting NSSI urges, little research has been conducted on their phenomenology. This is in sharp contrast to research examining other clinically relevant behaviors (e.g. craving and the development and treatment of substance use disorder; Robinson & Berridge, 1993; Skinner & Aubin, 2010). Therefore, the present study set out to characterize the environmental, interpersonal, and affective context in which urges occur in daily life using Ambulatory Assessment (AA). AA involves the collection of self-report data in real-life and near real time via smartphone, multiple times throughout the day (Trull & Ebner-Priemer, 2013).
Previous evidence on the phenomenology of NSSI urges in daily life reveals that research on the environmental context of urges is sparse. Two studies have found that adolescents and young adults most often reported urges during solitary activities (e.g., resting, doing homework), but that urges also occurred while socializing (Nock, Prinstein, & Sterba, 2009; Turner, Cobb, Gratz, & Chapman, 2016). Thus, it appears that urges occur both in contexts where NSSI acts would and would not be feasible. An additional aspect of the environmental context that has largely been overlooked is the temporal context (e.g., time of day, day of the week) of urges. Three studies have assessed when urges tend to occur and point to urge probability increasing in the afternoon (Andrewes et al., 2017; Lear, Wilkowski, & Pepper, 2019; Turner et al., 2018).
The interpersonal context of NSSI urges is particularly relevant since theory suggests that interpersonal factors play a role in the development of urges (e.g., Nock & Prinstein, 2004). Descriptively, Nock et al. (2009) found that adolescents were about equally likely to have urges while alone versus with others (mostly their mother or peers), whereas Turner and colleagues (2018) found that participants were alone 75% of the time when urges began. Beyond this, interpersonal conflict has been associated with same-day urge intensity (Turner et al., 2016) and participants indicated that interpersonal conflict preceded their urges in 21% (Andrewes et al., 2017) to 35% of events (Turner et al., 2016). Importantly, a recent study demonstrated that both perceived rejection and criticism also temporally precede urges (Victor, Scott, Stepp, & Goldstein, 2019).
The affective context of NSSI urges, specifically the association between negative affect and urges, has been assessed in several studies, though using a large variety of affect constructs. At the day level, urges were found to be positively associated with sadness (Bresin et al., 2013), guilt, and hostility (Lear et al., 2019). At the momentary level, urges were associated with concurrent anger (Humber, Emsley, Pratt, & Tarrier, 2013). Lagged analyses identified general negative affect (Andrewes et al., 2017; Kranzler et al., 2018) as well as ‘internalizing’ negative affect (e.g. ashamed, sad) and feeling anxious or overwhelmed (Kranzler et al., 2018) as a predictor of later NSSI urges. Moreover, several studies asked participants to report which affect occurred before the urge and found feelings of sadness/worthlessness, anger, and feeling overwhelmed to be most prevalent (Nock et al., 2009; Shingleton et al., 2013; Turner et al., 2016). The only previous study to track the whole affect trajectory found that negative affect increased before the urge, continued to rise after the urge, and then faded gradually (Snir, Rafaeli, Gadassi, Berenson, & Downey, 2015).
The present study
The present study used AA to assess the environmental, interpersonal, and affective context of NSSI urges in daily life. While previous studies have examined some of these contexts separately, none, to our knowledge, have examined them together. Doing so facilitates the examination of patterns across different factors. We additionally examined these factors in a sample of individuals with BPD. Although NSSI is broadly associated with psychopathology, it is characteristic of BPD (APA, 2013): most patients with BPD report NSSI over their lifetime (e.g., Dulit, Fyer, Leon, Brodsky, & Frances, 1994; Zanarini et al., 2008), and they report more frequent, recent, and severe NSSI compared to those without BPD who self-harm (Turner et al., 2015). We chose this clinical group, which is at high risk for NSSI, to increase the odds of observing NSSI urges during the assessment period and to provide sufficient observations for characterizing the context of NSSI urges. Moreover, despite the relevance of NSSI to BPD, only three studies have used AA to examine NSSI urges in those with BPD (Ammerman et al., 2017; Andrewes et al., 2017; Snir et al., 2015), thus there is also a need for more specific evidence for this at-risk population.
The first aim of this study was to examine the environmental context of NSSI urges. We examined time of day and whether urges were more likely to occur during the week versus the weekend. Additionally, to examine whether urges were more likely to occur in situations relatively more conducive to engaging in self-harm, we examined whether urges were more likely to occur at home, socializing, or with others. Due to the sparse previous evidence, we considered the examination of environmental context to be exploratory. Second, we assessed the interpersonal context of NSSI urges. Based on theory about the interpersonal function of NSSI (e.g., Nock & Prinstein, 2004) and previous findings (e.g., Turner et al., 2016; Victor et al., 2019), we hypothesized a positive concurrent association between NSSI urges and interpersonal stressors. Third, we investigated the affective context of urges in order to replicate previous findings of a positive association between NSSI urges and various types of negative affect (Andrewes et al., 2017; Bresin et al., 2013; Humber et al., 2013; Kranzler et al., 2018; Lear et al., 2019; Shingleton et al., 2013; Snir et al., 2015; Turner et al., 2016). We accomplished this in two ways, first examining the concurrent, momentary association between negative affect and NSSI urge endorsement (present or absent). Second, we examined the pattern of momentary negative affect before, during, and after an NSSI urge using a multilevel growth curve to examine the pattern of affective change over time. We expected that negative affect would increase prior to an urge, then peak and gradually decrease. Supplementary analyses were conducted for subscales of negative affect (hostility, sadness, and fear), to examine the consistency of findings. 1
Method
Participants
We included 56 participants who met criteria for BPD according to the Structured Interview for DSM-IV Personality (SIDP, Pfohl, Blum, & Zimmerman, 1994). Thirty-one participants (55.4%) fulfilled the NSSI/suicidality criterion of BPD. Participants were required to endorse the affective instability criterion of BPD to be eligible, but no participant was excluded due to this requirement (i.e., there were no participants that met for BPD diagnosis but not for affective instability). Clinical interviews were performed by clinical psychology graduate students. Interrater reliabilities were computed for a subsample (n = 20) that were rated by a second diagnostician, who watched a videotape of the initial interview. Reliabilities were excellent for the diagnosis of BPD (κ = 0.88).
Participants were required to be in some form of mental health treatment at the time of the study and were recruited through community advertisements (n = 11; 19.6%), from re-contacting participants who enrolled in prior studies (n = 4; 7.1%), and through treatment clinics (n = 41; 73.2%). The sample reported here is part of a larger parent study (Lane, Carpenter, Sher, & Trull, 2016) that assessed drinking behaviors in BPD and community drinkers. The overall inclusion criteria were: a) reporting consuming alcohol an average of at least once a week; b) not being in treatment or interested in seeking treatment for alcohol use; c) not currently experiencing withdrawal symptoms related to cutting down on alcohol use in the past year; d) not having a history of psychosis, intellectual disability, or head trauma that affected mood or concentration; e) being between 18 and 45 years old; and, f) (if female) not being pregnant or planning on becoming pregnant. Other publications using this dataset have assessed associations between interpersonal problems and negative affect, the context of alcohol consumption, the rate of alcohol consumption, and the experience of momentary pain in this sample (Carpenter, Tragesser, Lane, & Trull, 2018; Carpenter et al., 2017; Hepp, Lane, Wycoff, Carpenter, & Trull, 2018; Lane et al., 2016).
Participants included 82.1% women (n = 46) who ranged in age from 18 to 45 (M = 26.0, SD = 7.2). The majority of participants were Caucasian (83.9%), were single/never married (73.2%) and were currently employed (78.6%). Co-occurring disorders were assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders (First, Spitzer, Gibbon, & Williams, 1995). Thirty-six participants (64.3%) had a current anxiety disorder, twenty-nine (51.8%) another personality disorder, twenty-two (39.3%) a current mood disorder, twenty-two (39.3%) a current substance use disorder, and four (7.1%) a current eating disorder. Detailed sample characteristics for the whole sample and for the subgroup of 22 participants that reported NSSI urges during the AA assessment period (used for growth curve analyses described below) are displayed in Table 1.
Table 1.
Demographics and comorbid conditions in the full borderline personality disorder sample and in the subset of subjects reporting NSSI urges.
| Full BPD Sample (N = 56) |
Subset w. NSSI Urges (n = 22) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Racial/Ethnic Status | ||||
| Caucasian | 47 | 83.9% | 19 | 86.4% |
| Other | 4 | 7.1% | 1 | 4.5% |
| African-American | 3 | 5.4% | 1 | 4.5% |
| Hispanic | 1 | 1.8% | 0 | 0% |
| Asian-American | 1 | 1.8% | 1 | 4.5% |
| Marital Status | ||||
| Single or never married | 41 | 73.2% | 15 | 68.2% |
| Married | 7 | 12.5% | 2 | 9.1% |
| Divorced or separated | 7 | 12.5% | 5 | 22.7% |
| Cohabitating | 1 | 1.8% | 0 | 0% |
| Current Axis-I Comorbidity | ||||
| Any anxiety disorder | 36 | 64.3% | 13 | 59.1% |
| Any mood disorder | 21 | 37.5% | 9 | 40.9% |
| Any substance use disorder | 22 | 39.3% | 8 | 36.4% |
| Any eating disorder | 4 | 7.1% | 2 | 9.1% |
| Current Axis-II Comorbidity | ||||
| NSSI/suicidality criteriona | 31 | 55.4% | 14 | 63.6% |
| Any PD other than BPD | 29 | 51.8% | 12 | 54.5% |
| Antisocial PD | 11 | 19.6% | 4 | 18.2% |
| Avoidant PD | 9 | 16.1% | 6 | 27.3% |
| Obsessive Compulsive PD | 9 | 16.1% | 4 | 18.2% |
| Narcissistic PD | 5 | 8.9% | 1 | 4.5% |
| Paranoid PD | 6 | 10.7% | 4 | 18.2% |
| Schizotypal PD | 2 | 3.6% | 0 | 0% |
| Dependent PD | 2 | 3.6% | 2 | 9.1% |
| Histrionic PD | 1 | 1.8% | 1 | 4.5% |
| Schizoid PD | 0 | 0.0% | 0 | 0% |
Number of participants who endorsed the NSSI/suicidality criterion for BPD.
Procedure
The study was approved by the Institutional Review Board of the University of Missouri (Protocol 1133597). After an initial screening for eligibility, participants provided written informed consent and completed the diagnostic interviews. During an initial orientation session, participants completed baseline self-report measures and were issued an electronic diary and instructed in its use (ED; Palm Tungsten E2©). Participants were asked to carry the ED, programmed with customized software, for approximately 21 days (M = 21.6, SD = 2.1).
During the study period, participants responded to seven different types of prompts. Participants made morning reports each day after waking and had to complete these by 12:00pm. Random prompts notified participants (starting after their morning report or after 12:00pm) to fill out survey measures an average of six times each day. These random prompts were scheduled to occur at least 60 minutes apart and would not occur within 30 minutes of any other type of scheduled prompt. Participants also completed event-contingent drinking reports after finishing their first drink of a drinking episode. If reports of alcohol consumption were recorded on random prompts or on initial drink reports, participants completed drinking follow-up prompts, which were administered 30, 60, 120, and 180 minutes after logging an initial drink. These follow-up assessments were extended 60 minutes for each subsequent drink logged. Similarly, participants were instructed to initiate initial self-harm reports if they engaged in any self-harm behavior and were then prompted with self-harm follow-up prompts 30, 60, and 90 minutes following the initial endorsement of self-harm. Finally, participants in the sample who reported smoking cigarettes at baseline were administered cigarette prompts after smoking an initial cigarette. In these analyses, we only included data from the random prompts, initial drink reports, and the drinking follow-up prompts because NSSI urges were not assessed on the morning reports or cigarette prompts and because the inclusion of the initial self-harm reports and self-harm follow-up prompts would mean that subsequent NSSI urges and affect would be influenced by the previous NSSI act2.
Participants provided a total of 5,750 completed assessments, which corresponded to a high compliance with an average completion rate of 89.3% for the random prompts. Participants were paid weekly in accordance with their compliance. They received $50 at each weekly visit for completing at least 80% of the previous week’s random survey prompts and payment was reduced by $10 for each 10% reduction in compliance.
Measures
NSSI Urges:
At each prompt, participants were asked to indicate if they had experienced any urges to harm themselves on purpose since the last assessment (yes/no).
Time:
The times and dates that participants filled out survey prompts were recorded by the electronic diaries in a time-stamp. We extracted information from the time-stamps to create a variable that indicated the amount of time that had passed since the participant woke (centered on noon), a variable for day of the week, a variable for study day (from 1 to 21), and a variable that indicated whether it was a weekend day, beginning at 5:00pm on a Friday lasting until 5:00pm Sunday.
Location:
At each prompt, participants indicated their current location. Participants were allowed to check all location options that were applicable to them. Location options included being at school, work, a bar or restaurant, home, in their vehicle or some other location.
Activities:
At each prompt, participants indicated which activities they were participating in at the moment. Participants were allowed to check all options that were applicable to them. Options included watching TV/listening to music, socializing, working/studying, being on the phone, sleeping, walking, or other.
Alcohol consumption:
At each prompt, participants indicated whether they had been drinking alcohol since the last assessment (yes/no).
Interaction partners:
At each prompt, participants indicated whom they had spent time with in the past 15 minutes. Participants were allowed to check all options that were applicable to them. Options included having spent time with a romantic partner, friend, coworker, child(ren), parent, another family member, and someone else. If participants endorsed any of the above options, we coded them as being with someone versus being alone.
Interpersonal stressors:
These items were only assessed during random prompts. Participants indicated if they had experienced a “disagreement with anyone since the last prompt,” “felt rejected since the last prompt,” or “felt let down by someone they depend on since the last prompt”. Participants could choose between different interaction partners (romantic partner, boss, co-worker, roommate, friend, parent, sibling, child, family member) and check any that applied. For each perceived rejection, disagreement, and feeling of being let down, we created a single dichotomous variable that indicated whether any rejection, disagreement or feeling let down (independent of the interaction partner) had taken place since the last prompt. If any rejection/ disagreement/let down had occurred, the variable was coded 1 and if none occurred it was 0. These three momentary variables were then averaged within person, within day to create three day-level variables indicating the proportion of prompts within a day where rejection/ disagreement/ let down were reported (ranging from 0 to 1). Likewise, these day-level scores were averaged for each participant, indicating the proportion of days in the study on which a participant endorsed these interpersonal stressors.
Negative Affect:
Participants rated negative affect at each prompt using 21 items from the Positive and Negative Affect Schedule-Extended version (PANAS-X; Watson & Clark, 1994). Participants indicated their level of affect with reference to the past 15 minutes on a scale from 1 (very slightly/not at all) to 5 (extremely) and a mean negative affect score was created. For supplementary analyses, the items were used to create hostility (6 items), sadness (5 items), and fear (6 items) scales.
Data Analysis
Descriptive analyses:
Following the approach taken by Nock et al. (2009), we computed percentages for how often participants endorsed each environmental, affective, and interpersonal context during prompts where NSSI urges were reported vs. non-urge prompts.
Multilevel model:
Augmenting the descriptive analyses, we computed a logistic multilevel model (MLM) using momentary NSSI urges (1 = present, 0 = absent) as the criterion and entered all context variables simultaneously as predictors. This way, we were able to test which contexts were significantly associated with NSSI urges. We included data from the full sample for this analysis, as we used context variables to predict whether or not urges occurred at a given prompt. We included participants who did not report urges, but whom we considered at risk of experiencing urges (because they met criteria for BPD) in these analyses to provide models with more information about the context of moments where participants are not experiencing urges. This is consistent with the approach of previous studies (e.g., Snir et al., 2015; Victor et al., 2019). Within the MLM, we employed a logit link function and modelled random intercepts for each person. Analyses were performed in R using the glmer function from the package lme4 (Bates, Maechler, Bolker, & Walker, 2014). Significance tests were conducted using the package lmerTest (Kuznetsova, Brockhoff, & Christensen, 2014). To assess temporal context, we included the number of hours since the participant awoke (centered on noon) and a dummy variable coding whether it was a weekday or weekend (5PM Friday through 5PM Sunday) as predictors. To assess environmental context, we included dummy variables coding whether the participant was at home or elsewhere, whether they were socializing, whether they reported any alcohol consumption, and whether they were with another person at the time of assessment or not. The model further included indicators of interpersonal context, that is, dummies for whether any momentary rejection, disagreement, or instances of feeling let down had occurred. Lastly, we included momentary negative affect to model the affective context. All momentary predictors were centered on the participant’s day mean. While our primary interest was in these moment-level effects, day- (person mean centered) and person-level (grand mean centered) effects for all predictors were also included. This was done to adjust for the fact that moments were nested within days, which were nested within people. Adjusting for the day- and person-level means of the predictor variables allowed us to disaggregate moment-, day-, and person-level effects (see Curran & Bauer, 2011 for further details on disaggregating different levels of analyses).
Growth curve model:
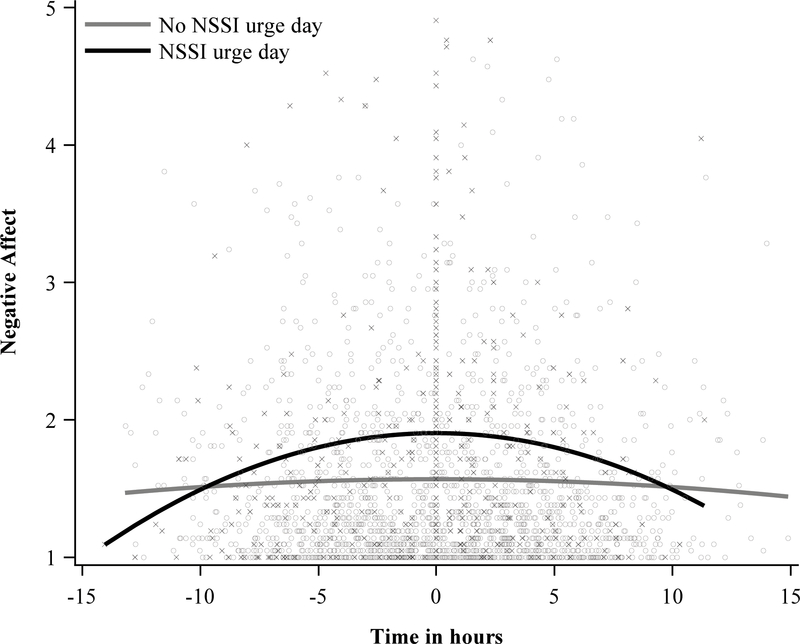
To more closely characterize the pattern of negative affect in relation to urges, we modeled the negative affect trajectory surrounding NSSI urges using a multilevel growth curve model. This analysis used the subset of 22 participants that reported at least one urge throughout the study period (nobservations = 2,312). For days where participants reported an urge (ndays = 83), we first created a time variable that calculated the number of minutes each prompt was before or after an urge. Prompts where an urge was reported had a value of zero, prompts that occurred prior to the urge had a negative value, and prompts that occurred after had a positive value.3 Linear and quadratic effects of this time variable then served as predictors and negative affect was the criterion. This allowed us to examine the pattern of affect across a day in which an NSSI urge occurred. We were particularly interested in the quadratic effect of time, as we hypothesized that negative affect would increase prior to the NSSI urge, and peak during or shortly after the urge and then decrease. The model included a random intercept and random slopes for linear and quadratic time effects at the person level and were performed using the PROC MIXED procedure in SAS® 9.4 (SAS Institute, 2014), using restricted maximum likelihood estimation.
Additionally, in order to ensure that the observed trajectories of affect were specific to NSSI urge days, we also included non-urge days (ndays = 375) in the model as a comparison. For non-urge days, we centered time for these days around the average time at which urges occurred for each participant. We then included in the models a dummy variable for NSSI urge day (coded 1) or non-urge day (coded 0), as well as interaction terms for the urge day variable with linear and quadratic effects of time. Study day, weekend vs. weekday, and time elapsed since participant woke were included as covariates.
Results
Descriptive Results
Twenty-two participants (39.3%) reported 160 NSSI urges over the course of the study. The majority of NSSI urges (71.9%) occurred on random prompts, with 6.3% of reported NSSI urges occurring on initial drink reports, and 21.9% occurring on drinking follow-up prompts. Table 2 shows the percentage of NSSI urge prompts (contrasted to non-urge prompts) for different locations, activities, interpersonal stressors, and times during the day and week. Descriptively, most NSSI urges were endorsed in the evenings (6:00pm-1:00am; 79.1%), and participants were most often at home when reporting urges (74.4%). With regard to activities participants were performing when they reported urges, participants most often chose an ‘other’ category (70.6%) and also reported watching TV or listening to music (64.4%) or socializing (43.1%). On 30% of prompts where participants endorsed NSSI urges, they indicated also having consumed alcohol. During prompts where NSSI urges were reported, participants reported being with another person in 65.5% of cases and were most often with a friend (40%) or their romantic partner (32.3%). Both rejection (21.7%) and disagreement (11.3%) were substantially endorsed during NSSI urges, whereas feeling let down was not (5.2%).
Table 2.
Contexts with whom, where, when, and during which activities NSSI urges occurred.
| Percent (%) endorsement |
||
|---|---|---|
| prompts with NSSI urges | prompts without NSSI urges | |
| Interaction partner | ||
| Friend | 40.00% | 27.10% |
| Romantic partner | 32.25% | 16.71% |
| Any other person | 19.38% | 9.50% |
| Other family member | 11.88% | 5.25% |
| Child | 11.88% | 8.35% |
| Parent | 2.50% | 4.76% |
| Co-worker | 0.62% | 10.91% |
| Anyone (aggregated) | 65.63% | 58.93% |
| Interpersonal stressora | ||
| Disagreement | 11.30% | 7.53% |
| Felt Rejected | 21.74% | 7.57% |
| Felt let down | 5.22% | 3.31% |
| Current location | ||
| Home | 74.38% | 56.57% |
| Work | 3.13% | 10.81% |
| School | 2.50% | 5.56% |
| Bar/restaurant | 1.88% | 5.46% |
| Vehicle | 4.38% | 8.23% |
| Other location | 15.63% | 19.00% |
| Temporal context | ||
| Weekday | 70.00% | 69.21% |
| Weekend | 30.00% | 30.79% |
| Morning (5:00am-11:00am) | 7.50% | 12.79% |
| Afternoon (12:00pm-5:00pm) | 35.63% | 40.47% |
| Evening (6:00pm-1:00am) | 79.13% | 46.74% |
| Current activity | ||
| TV/music | 64.38% | 41.36% |
| Socializing | 43.12% | 36.40% |
| Work/study | 30.00% | 31.23% |
| On phone | 7.50% | 7.89% |
| Resting | 4.38% | 6.03% |
| Walking | 3.75% | 6.62% |
| Other activity | 70.62% | 37.64% |
| While drinking alcohol | 30.00% | 14.97% |
Interpersonal stressors were only assessed at random prompts, so percentages were calculated using total number of random prompts as the denominator. These variables are missing for 45 urges.
Multilevel model results
To assess the associations between these contexts and NSSI urges more closely, we conducted a MLM, using contexts as predictors of urges. The results of this MLM are presented in Table 3. Note that by including all context predictors simultaneously, the individual odds ratios represent the effect of the predictor above and beyond the effects of all other included predictors. Results from the MLM showed a positive association between NSSI urges and momentary general negative affect. Additional analyses testing the associations between three specific negative affects (hostility, sadness, fear) are presented in the supplemental material and show that NSSI urges were also positively associated with each specific negative affect (see table S1). In addition to a positive association with negative affect, NSSI urges were also positively associated with momentary rejection. That is, higher levels of negative affect and the presence of a momentary rejection increased the probability of a participant reporting and NSSI urge (above and beyond the effects of any other context in the model). Additionally, results showed that the number of hours that had passed since a participant woke was significantly associated with the probability to experience an NSSI urge. Participants were more likely to experience an urge if it was later during their wake-time.
Table 3.
Results from a logistic multilevel model in which momentary NSSI urges were predicted by affective, interpersonal, and environmental context variables simultaneously.
| Predictor | OR | 95% CI | SE | p |
|---|---|---|---|---|
| Intercept | 0.00 | [0.00; 0.00] | 0.61 | <.001 |
| Momentary predictors | ||||
| Negative affect | 7.50 | [3.87; 14.52] | 0.34 | <.001 |
| Rejection | 4.28 | [1.67; 10.9] | 0.48 | .003 |
| Disagreement | 2.47 | [0.59; 10.26] | 0.72 | .213 |
| Feeling let down | 0.32 | [0.04; 2.44] | 1.03 | .272 |
| Alcohol consumption | 2.63 | [0.93; 7.45] | 0.53 | .069 |
| Being in company | 0.60 | [0.29; 1.24] | 0.37 | .166 |
| Being at home | 0.66 | [0.32; 1.37] | 0.37 | .267 |
| Activity socializing | 1.68 | [0.80; 3.55] | 0.38 | .171 |
| Hour after wake | 1.13 | [1.06; 1.21] | .032 | <.001 |
| Day-level average predictors | ||||
| Negative affect | 3.85 | [2.13; 6.96] | 0.30 | <.001 |
| Rejection | 3.40 | [0.72; 16.0] | 0.79 | .121 |
| Disagreement | 0.01 | [0.0; 0.26] | 1.73 | .006 |
| Feeling let down | 11.96 | [0.14; >999] | 2.26 | .271 |
| Alcohol consumption | 5.96 | [1.33; 26.6] | 0.76 | .019 |
| Being in company | 2.19 | [0.81; 5.9] | 0.50 | .122 |
| Being at home | 0.72 | [0.32; 1.64] | 0.42 | .438 |
| Activity socializing | 0.36 | [0.11; 1.21] | 0.62 | .098 |
| Weekend vs. weekday | 0.94 | [0.56; 1.60] | 0.27 | .830 |
| Person-level average predictors | ||||
| Negative affect | 5.00 | [1.01;24.6] | 0.81 | .048 |
| Rejection | >999 | [0.06; >999] | 6.68 | .121 |
| Disagreement | 0.00 | [0.00; 1.18] | 13.91 | .051 |
| Feeling let down | 65.54 | [0.00; >999] | 16.31 | .797 |
| Alcohol consumption | >999 | [30.04; >999] | 4.26 | .006 |
| Being in company | 4.74 | [0.10; 214.12] | 1.95 | .424 |
| Being at home | 24.26 | [0.37; >999] | 2.14 | .135 |
| Activity socializing | 0.00 | [0.00; 0.51] | 2.69 | .027 |
Note. OR = odds ratio, SE = standard error, CI = confidence interval. Momentary predictors were centered within day, day-level predictors were centered within person, and person-level predictors were centered within the grand mean. The model included day and person-level aggregates of each context variable in order to isolate momentary effects.
The other predictors (being at home vs. elsewhere, socializing vs. another activity, drinking vs. no drinking, being with someone vs. alone, weekdays vs. weekends) did not show significant associations with NSSI urges.4
Growth curve results for negative affect
We examined the pattern of negative affect across the day prior to, during, and following urges. The interaction of urge-day and the quadratic effect for time was significant (Table 4). This interaction indicated that, on urge days, negative affect increased prior to experiencing an NSSI urge and then decreased after the urge (see Figure 1). This pattern was not observed on non-urge days. Supplementary results found that this pattern also held for sadness and hostility, but not fear (Table S2).
Table 4.
Results from multilevel model examining the trajectory of negative affect over time on NSSI urge and non-urge days.
| Predictor | b | 95% CI | SE | p |
|---|---|---|---|---|
| Intercept | 1.74 | [1.46, 2.02] | 0.14 | <.0001 |
| Urge day | 0.34 | [0.27, 0.41] | 0.04 | <.0001 |
| Linear time | 0.03 | [0.01, 0.04] | 0.01 | .000 |
| Linear time x urge day | 0.004 | [−0.01, 0.02] | 0.01 | .603 |
| Quadratic time | −0.001 | [−0.002, 0.001] | 0.001 | .272 |
| Quadratic time x urge day | −0.003 | [−0.005, −0.001] | 0.001 | .016 |
Note. nobservations = 2,298. CI = confidence interval, SE = standard error. Time on urge days was centered around the occurrence of an NSSI urge. For non-urge days, time was centered around the average time at which each participant experienced urges on urge days. The model adjusted for main effects of study day, weekend, and time elapsed since the participant awoke (centered on noon).
Figure 1.
Model-fit trajectories of negative affect over time relative to the experience of an urge on NSSI urge compared to non-urge days. For non-urge days, we centered time for these days around the average time at which urges occurred for each participant (“X”s indicate momentary reports from NSSI urge days, and “O”s indicate reports from non-urge days.)
Discussion
The present study assessed the environmental, interpersonal, and affective context of NSSI urges in daily life in a sample of BPD outpatients. To our knowledge, this was the first AA study to examine these contexts together in the same sample. We chose this sample, although not recruited specifically to examine NSSI, as one in which we would be likely to observe NSSI urges. Of the 56 included participants with BPD, 22 participants reported a total of 160 NSSI urges across the 21-day study period. By using AA, we were able to examine the association of within-person contextual factors with NSSI urges. The results provide a nuanced understanding of NSSI urges that builds upon previous work, showing that rejection experiences and negative affect were associated with experiencing an urge, while environmental factors were less so. As indicated by the supplementary lagged model (see Table S3 in online supplement), associations were largely contemporaneous in nature.
The environmental factors assessed were largely unassociated with NSSI urges. The primary exception was that urges were more likely to occur in the evening, consistent with findings by Turner et al. (2018). Examining the descriptive statistics for activities and location (Table 2), participants were also most frequently watching TV/listening to music and at home when they had an urge. In a sense, this is somewhat surprising, given that interventions such as DBT encourage patients to use activities to distract themselves from NSSI urges, and these activities include watching TV and listening to music. However, in the case of DBT, these activities are meant to be used actively in response to an urge that has already occurred. Though speculative, participants may have been engaging in these activities at home in a more “mindless” rather than “mindful” way.
Overall, however, we had limited success in capturing all of the activities participants were engaged in when they had an urge, as participants reported doing an “other activity” at 70.62% of the prompts where they had an urge (compared to 37.64% of non-urge moments). This suggests that future research on the context of NSSI urges should consider a broader array of activities. We were most interested in whether participants were more likely to experience urges while at home or alone, contexts in which NSSI acts may be most feasible. However, this was not the case and reinforces the idea that urges, unlike acts, are not restricted by context, but may occur both when it may be feasible to self-injure (e.g., alone, at home) and when it may not be (e.g., with others, away from home). This makes NSSI urges an important phenomenon to study in daily life, as the associations of urges and other constructs that are similarly unrestricted (e.g., negative affect), are less likely to be affected by contextual variables than are NSSI acts. In this way, examining NSSI urges may provide a fuller understanding of factors relevant to NSSI that might be obscured by only examining acts.
In addition to urges being more likely later in the day, we also found urges to be positively associated with negative affect. These findings are in line with previous work, replicating positive associations between momentary NSSI urges and negative affect (Andrewes et al., 2017; Humber et al., 2013; Kranzler et al., 2018; Nock et al., 2009; Shingleton et al., 2013; Turner et al., 2016). Findings regarding the pattern of negative affect across NSSI urge days, as compared to non-urge days, complement these concurrent affect findings. We observed a quadratic trajectory for negative affect around urges, such that participants reported more negative affect the nearer in time they were to experiencing the urge. This quadratic trajectory was significantly distinct from the pattern present over non-urge days. Supplementary analyses indicated that the pattern was specific to hostility and sadness, and not present for fear. Unlike Snir et al. (2015), we found that peak negative affect occurred at the time of the urge and declined immediately after the urge ceased.
The finding of a positive association between NSSI urges and rejection also replicates a previous findings (Victor et al., 2019) and underlines the importance of considering interpersonal events in relation to NSSI phenomena. It is unclear why disagreements and feeling let down were not associated with urges, though they were both endorsed much less frequently than rejection overall. It may also be that rejection is a more intense experience than disagreement or feeling let down, and, thus, more likely to be associated with NSSI urges. Assessing the intensity of interpersonal stressors (beyond the presence vs. absence assessed herein) may help further elucidate this in the future.
Overall, our findings suggest that NSSI urges often occur at moments of distress, whether interpersonal or affective. This is consistent with the four-function model of NSSI (Nock & Prinstein, 2004), which suggests that some individuals engage in NSSI to alleviate negative intrapersonal (e.g. negative affect) or negative interpersonal (e.g. rejection) experiences. In other words, the present findings that urges are more likely at time-points where higher negative affect or negative interpersonal experiences are endorsed, aligns well with theories suggesting that such events can trigger NSSI. Likewise, these findings are in line with evidence that individuals who self-harm frequently endorse affect regulation and/or interpersonal motivations for NSSI (Klonsky & Muehlenkamp, 2007; Taylor et al., 2018). Treatments, such as DBT (Linehan, 1993), that specifically target emotion dysregulation and interpersonal dysfunction, in addition to NSSI more directly, may thus also have positive indirect effects on reducing NSSI urges. Further, the pattern of negative affect on urge days suggests that changes brought about by treatment have the potential to prevent the development of urges long before they occur. Future research should examine whether training in emotion regulation and interpersonal effectiveness skills has downstream effects on NSSI.
Limitations
The current study has several strengths, most notably the use of AA to intensively sample NSSI urges and their environmental, interpersonal, and affective contexts longitudinally and within-person in a clinically-relevant group. Additionally, the study provides replication of several previously reported results, most notably for rejection and negative affect. There is a significant need for increased replication work in clinical psychology (e.g., Tackett, Brandes, King, & Markon, 2019).
However, there were also limitations. First, we were not able to examine NSSI acts in relation to urges. This was because few participants engaged in NSSI during the study period (8 participants reported 25 acts overall). In part, this is likely due to the fact that the sample was primarily recruited to examine alcohol consumption, and not NSSI urges or acts. However, it is also the case that NSSI acts are infrequent and may not be expected to be captured in large numbers over an AA period of several weeks. Nevertheless, the generalizability of the present findings to more actively self-harming individuals is not clear. At the same time, the finding that urges still occurred during this study period when most participants were not actively self-harming, has implications in and of itself. It suggests that these participants remain at elevated risk for NSSI and underlines the importance of assessing potentially negative outcomes of urges themselves. For example, the effort required to ignore or otherwise manage urges may sap cognitive resources or make it more difficult for individuals to engage in interpersonal interactions or function in the workplace.
A second, and related, limitation is that urges were assessed in a dichotomous fashion (present/absent). It is possible that participants mostly experienced urges of mild or moderate intensity that therefore did not lead to eventual engagement in NSSI. Likewise, contexts for mild versus severe urges may differ, which is something the present study was unable to address. From a clinical perspective, it would be particularly important to better understand high-urge contexts to determine interventions that may be applicable there. Thus, future studies should aim to capture the intensity of the urge to gain deeper insight into both then associations between urges and acts, and the contexts associated with more intense urges.
Third, as the current study was observational, none of the observed associations are causal. Additionally, with the exception of the trajectory analyses for negative affect, analyses were all concurrent in time (though see footnote 3 and Table S3 for lagged results). This renders the temporal ordering of events somewhat unclear, especially as urges and interpersonal problems were assessed since the last prompt, whereas negative affect and most environmental factors were assessed ‘right now’ or over the past 15 minutes. Therefore, it is possible that an NSSI urge occurred sometime before the prompt at which contexts were assessed. To account for the possibility that contexts had changed from the time participants experienced the urge until the time they report contexts, we looked at concordance rates for all context variables. The activities that we statistically tested as contexts for NSSI urges showed substantial concordance rates, with 82.2% for alcohol consumption and 69.2% for socializing. Looking at participants’ locations, being at home showed a concordance 67.2% and all other contexts showed concordance >80%. Concordance for the aggregated variable of having contact with anyone was 65.5% with substantially higher rates for individual interaction partners (all > 80%), indicating that specific interaction partners changed little from the prompt prior to the urge to the urge prompt. Nonetheless, we acknowledge that these different time frames were not ideal for the assessment of environmental context and future studies could remedy this by specifically asking about all current context variables upon urge reports.
Fourth, our recruitment strategy may have introduced several limitations. The recruitment strategy did not require participants to have an NSSI history or impose any other threshold for NSSI urges or behaviors but rather sampled BPD participants that endorsed the affective instability criterion of BPD and regularly consumed alcohol (inclusion criteria of the parent study, see Lane et al., 2016). Thus, only 31 participants (55.4% of the sample) fulfilled the NSSI criterion of BPD, and a subset of 22 participants reported urges throughout the study period (39% of the sample). While this number is low, it is comparable to urge endorsements in other samples. For example, Snir et al. (2015), who similarly did not require participants to be actively experiencing NSSI urges, found only 35% of participants with BPD reported an urge. Similarly, Victor et al. (2019) found 45% of participants reported an urge. Additionally, while the total number of urges reported in the sample was also low (n = 160; 2.8% of all prompts), it was similarly comparable to Snir et al. (2015) and Victor et al. (2019). Beyond the prevalence of NSSI urges in the sample, the recruitment strategy may also have influenced the base rates for negative affect and drinking behavior in this sample and therefore could have inflated the association between these constructs and NSSI urges. With regard to affective instability, however, this is less concerning as no participants were excluded for not meeting this requirement. In addition, the present sample was relatively small and mostly white and female. It is, thus, unclear to what extent the findings generalize beyond the current sample and more research is needed on the daily life context of NSSI urges in individuals with and without BPD.
Conclusion
The present study examined the environmental, interpersonal, and affective context of NSSI urges in a sample of outpatients with BPD in their daily lives, using AA. We found that urges tended to occur later during a participant’s wake-time, when participants experienced high levels of negative affect, and when they endorsed feeling rejected by someone. Over the course of days with NSSI urges, negative affect followed a quadratic trajectory, rising prior to the urge and falling afterward. These findings are in line with the intrapersonal and interpersonal negative reinforcement functions of NSSI (Nock & Prinstein, 2004), which posit that individuals self-harm to alleviate negative affective or interpersonal experiences. We demonstrated that these exact contexts also were associated with NSSI urges, which again suggests that understanding the context in which NSSI urges occur may eventually help to better prevent and treat NSSI behavior.
Supplementary Material
Acknowledgments
Conflicts of Interest and Source of Funding: The authors identify no conflicts of interest. This research was supported by the National Institutes of Health (National Institute on Alcohol Abuse and Alcoholism) research grants P60 AA11998, and T32 AA007459.
Footnotes
The present study was a secondary data analysis of existing data and, while we expected that BPD participants would report NSSI urges, the sample was not recruited specifically to examine NSSI.
Eight Participants reported a total of only 25 NSSI acts over the course of the study. The majority of these events (17) were reported on initial self-harm reports, five NSSI events were endorsed on random prompts and two were endorsed on initial drink reports. Due to the small number of NSSI events, their association with urges in this sample was not further assessed and self-initiated NSSI prompts were excluded from the analyses.
If there were multiple urges across consecutive prompts, time did not advance until the participant no longer reported an urge. Results did not differ if, instead, time advanced on the prompt after the first prompt where an urge was reported. Additionally, there were rare occasions where urges were reported on nonconsecutive prompts within a day (e.g., in the morning and in the evening). All “secondary” urges and following prompts (n = 12) were removed from the growth curve analyses, but results did not differ if they were included. If an urge occurred on the first prompt of a day, it was still included in all the models, however, in this case, there would be no information about negative affect and other constructs prior to the urge. Similarly, if an urge was reported at the last prompt of the day, there would be no information about negative affect after the urge. Multilevel models are able to adjust for missing data like this across days and persons, therefore all urge data points were retained.
In the Supplemental Material, we report the results of a lagged version of the model reported here, which included the previous-moment report of all variables as additional predictors. Time-lagged analyses can clarify the temporal ordering of events, but their interpretation becomes complicated when the temporal spacing between assessments varies over time, as was the case in the present data. Additionally, lags tended to be relatively distant, with random prompts an average of about two hours apart, and it is not clear that we would expect events or experiences to be associated with urges hours later. Nevertheless, lagged analyses can provide useful information. As presented in Table S3, results from the lagged model were highly consistent with those in Table 3. All significant associations in the concurrent-only model were significant in the lagged model. Lagged momentary disagreement was the only lagged predictor associated with NSSI urges.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5™. Washington, DC: American Psychiatric Asociation. [Google Scholar]
- Ammerman BA, Olino TM, Coccaro EF, & McCloskey MS (2017). Predicting Nonsuicidal Self-Injury in Borderline Personality Disorder Using Ecological Momentary Assessment. Journal of Personality Disorders, 31(6), 844–855. doi: 10.1521/pedi_2017_31_278. [DOI] [PubMed] [Google Scholar]
- Andrewes HE, Hulbert C, Cotton SM, Betts J, & Chanen AM (2017). Ecological momentary assessment of nonsuicidal self-injury in youth with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 8(4), 357–365. doi: 10.1037/per0000205 [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B, & Walker S (2014). lme4: Linear mixed-effects models using Eigen and S4. R package (Version 1.1–7). Retrieved from http://CRAN.R-project.org/package=lme4 [Google Scholar]
- Bresin K, Carter DL, & Gordon KH (2013). The relationship between trait impulsivity, negative affective states, and urge for nonsuicidal self-injury: A daily diary study. Psychiatry Research, 205(3), 227–231. doi: 10.1016/j.psychres.2012.09.033. [DOI] [PubMed] [Google Scholar]
- Carpenter RW, Tragesser SL, Lane SP, & Trull TJ (2018). Momentary assessment of everyday physical pain in outpatients with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 10, 143–153. doi: 10.1037/per0000304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter RW, Trela CJ, Lane SP, Wood PK, Piasecki TM, & Trull TJ (2017). Elevated rate of alcohol consumption in borderline personality disorder patients in daily life. Psychopharmacology, 234(22), 3395–3406. doi: 10.1007/s00213-017-4727-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. doi: 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulit RA, Fyer MR, Leon AC, Brodsky BS, & Frances AJ (1994). Clinical correlates of self-mutilation in borderline personality disorder. The American Journal of Psychiatry, 151(9), 1305–1311. doi: 10.1176/ajp.151.9.1305 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured Clinical Interview for DSM-IV Axis I disorders - patient ed. (SCID-I/P, version 2). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Hepp J, Lane SP, Wycoff AM, Carpenter RW, & Trull TJ (2018). Interpersonal stressors and negative affect in individuals with borderline personality disorder and community adults in daily life: A replication and extension. Journal of Abnormal Psychology, 127(2), 183–189. doi: 10.1037/abn0000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes CD, King AM, Kranzler A, Fehling K, Miller A, Lindqvist J, & Selby EA (2019). Anxious and overwhelming affects and repetitive negative thinking as ecological predictors of self-injurious thoughts and behaviors. Cognitive Therapy and Research, 43(1), 88–101. doi: 10.1007/s10608-019-09996-9 [DOI] [Google Scholar]
- Humber N, Emsley R, Pratt D, & Tarrier N (2013). Anger as a predictor of psychological distress and self-harm ideation in inmates: A structured self-assessment diary study. Psychiatry Research, 210(1), 166–173. doi: 10.1016/j.psychres.2013.02.011. [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2011). Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychological Medicine, 41(9), 1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, & Muehlenkamp JJ (2007). Self-injury: A research review for the practitioner. Journal of Clinical Psychology, 63(11), 1045–1056. doi: 10.1002/jclp.20412 [DOI] [PubMed] [Google Scholar]
- Kranzler A, Fehling KB, Lindqvist J, Brillante J, Yuan F, Gao X, … Selby EA (2018). An ecological investigation of the emotional context surrounding nonsuicidal self-injurious thoughts and behaviors in adolescents and young adults. Suicide and Life-Threatening Behavior, 48(2), 149–159. doi: 10.1111/sltb.12373. [DOI] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2014). lmerTest: Tests in Linear Mixed Effects Models (Version 2.0–20). Retrieved from http://cran.r-project.org/web/packages/lmerTest/index.html [Google Scholar]
- Lane SP, Carpenter RW, Sher KJ, & Trull TJ (2016). Alcohol craving and consumption in Borderline Personality Disorder: When, where, and with whom. Clinical Psychological Science, 4(5), 775–792. doi: 10.1177/2167702615616132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lear MK, Wilkowski BM, & Pepper CM (2019). A daily diary investigation of the defective self model among college students with recent self-injury. Behavior Therapy, 50(5), 1002–1012. doi: 10.1016/j.beth.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive behavioral therapy of borderline personality disorder (Vol. 51): New York: Guilford Press. [Google Scholar]
- Nock MK, & Prinstein MJ (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. doi: 10.1037/0022-006X.72.5.885 [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba SK (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfohl B, Blum N, & Zimmerman M (1994). Structured interview for DSM-IV personality disorders. Iowa City: University of Iowa Hospitals and Clinics. [Google Scholar]
- Ribeiro J, Franklin J, Fox KR, Bentley K, Kleiman EM, Chang B, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236. doi: 10.1017/S0033291715001804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, & Berridge KC (1993). The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Research Reviews, 18(3), 247–291. [DOI] [PubMed] [Google Scholar]
- Shingleton RM, Eddy KT, Keshaviah A, Franko DL, Swanson SA, Jessica SY, … Herzog DB (2013). Binge/purge thoughts in nonsuicidal self- injurious adolescents: An ecological momentary analysis. International Journal of Eating Disorders, 46(7), 684–689. doi: 10.1002/eat.22142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair JM, Gray A, Rivero-Arias O, Saunders KE, & Hawton K (2011). Healthcare and social services resource use and costs of self-harm patients. Social psychiatry and psychiatric epidemiology, 46(4), 263–271. doi: 10.1007/s00127-010-0183-5. [DOI] [PubMed] [Google Scholar]
- Skinner MD, & Aubin H-J (2010). Craving’s place in addiction theory: contributions of the major models. Neuroscience & Biobehavioral Reviews, 34(4), 606–623. doi: 10.1016/j.neubiorev.2009.11.024 [DOI] [PubMed] [Google Scholar]
- Snir A, Rafaeli E, Gadassi R, Berenson K, & Downey G (2015). Explicit and inferred motives for nonsuicidal self-injurious acts and urges in borderline and avoidant personality disorders. Personality Disorders: Theory, Research, and Treatment, 6(3), 267–277. doi: 10.1037/per0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St John NJ (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide and Life-Threatening Behavior, 44(3), 273–303. doi: 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Brandes CM, King KM, & Markon KE (2019). Psychology’s replication crisis and clinical psychological science. Annual Review of Clinical Psychology, 15, 579–604. doi: 10.1146/annurev-clinpsy-050718-095710 [DOI] [PubMed] [Google Scholar]
- Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, & Dickson JM (2018). A meta-analysis of the prevalence of different functions of non-suicidal self-injury. Journal of Affective Disorders, 227, 759–769. doi: 10.1016/j.jad.2017.11.073 [DOI] [PubMed] [Google Scholar]
- Trull TJ, & Ebner-Priemer U (2013). Ambulatory assessment. Annual Review of Clinical Psychology, 9, 151–176. doi: 10.1146/annurev-clinpsy-050212-185510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Baglole JS, Chapman AL, & Gratz KL (2018). Experiencing and resisting nonsuicidal self-injury thoughts and urges in everyday life. Suicide and Life-Threatening Behavior. doi: 10.1111/sltb.12510. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Cobb RJ, Gratz KL, & Chapman AL (2016). The role of interpersonal conflict and perceived social support in nonsuicidal self-injury in daily life. Journal of Abnormal Psychology, 125(4), 588–598. doi: 10.1037/abn0000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Dixon-Gordon KL, Austin SB, Rodriguez MA, Rosenthal MZ, & Chapman AL (2015). Non-suicidal self-injury with and without borderline personality disorder: Differences in self-injury and diagnostic comorbidity. Psychiatry Research, 230(1), 28–35. doi: 10.1016/j.psychres.2015.07.058. [DOI] [PubMed] [Google Scholar]
- Victor SE, Scott LN, Stepp SD, & Goldstein TR (2019). I want you to want me: Interpersonal stress and affective experiences as within-person predictors of nonsuicidal self-injury and suicide urges in daily life. Suicide and Life-Threatening Behavior, 49(4), 1157–1177. doi: 10.1111/sltb.12513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn JJ, Juzwin K, Styer DM, & Aldridge D (2010). Measuring the urge to self-injure: Preliminary data from a clinical sample. Psychiatry Research, 178(3), 540–544. doi: 10.1016/j.psychres.2010.05.018. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1994). The PANAS-X: Manual for the positive and negative affect schedule-expanded form.
- Zaki LF, Coifman KG, Rafaeli E, Berenson KR, & Downey G (2013). Emotion differentiation as a protective factor against nonsuicidal self-injury in borderline personality disorder. Behavior Therapy, 44(3), 529–540. doi: 10.1016/j.beth.2013.04.008. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, & Gunderson JG (2008). The 10-year course of physically self-destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatrica Scandinavica, 117(3), 177–184. doi: 10.1111/j.1600-0447.2008.01155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.