Abstract
Introduction
In response to the COVID-19 pandemic in Detroit, an earlier termination of resuscitation protocol was initiated in March 2020. To characterize pre-hospital cardiac arrest careduring COVID-19 in Detroit, we analyzed out-of-hospital cardiac arrest (OHCA) rate of ROSC (return of spontaneous circulation) and patient characteristics before and during the COVID-19 pandemic.
Methods
OHCA data was analyzed between March 10th, 2020 – April 30th, 2020 and March 10th, 2019 – April 30th, 2019. ROSC, patient demographics, arrest location, initial rhythms, bystander CPR and field termination were compared before and during the pandemic. Descriptive statistics were utilized to compare arrest characteristics between years, and the odds of achieving vs. not achieving ROSC. 2020 vs. 2019 as a predictor for ROSC was assessed with logistic regression.
Results
471 patients were included. Arrests increased to 291 during the pandemic vs. 180 in 2019 (62% increase). Age (mean difference + 6; 95% CI: +2.4 to +9.5), arrest location (nursing home OR = 2.42; 95% CI: 1.42–4.31; public place OR = 0.47; 95% CI: 0.25–0.88), BLS response (OR = 0.68; 95% CI: 0.47–0.99), and field termination of resuscitation (OR = 2.36; 95% CI: 1.36–4.07) differed significantly in 2020 compared to 2019. No significant difference was found in the confounder-adjusted odds of ROSC in 2020 vs 2019 (OR = 0.61; 95% CI: 0.34–1.11).
Conclusion
OHCA increased by 62% during COVID-19 in Detroit, without a significant change in prehospital ROSC. The rate of ROSC remained similar despite the implementation of an early termination of resuscitation protocol in response to COVID-19.
Keywords: Cardiac arrest, Out-of-hospital cardiac arrest, Emergency medical services, SARS-CoV-2, COVID-19
1. Background
In 2002, the out-of-hospital cardiac arrest (OHCA) survival rate in Detroit was merely 0.2%, a nearly uniform fatal event [1]. In 2013, the city filed for the largest municipal bankruptcy in the nation. As few as 6 functioning emergency medical service (EMS) units were in service some days during that period. Since 2013, Detroit has made significant improvements in out-of-hospital cardiac arrest care, from the implementation of non-transporting fire units in a medical role, priority dispatch, dispatch-assisted cardiopulmonary resuscitation (CPR) and community bystander CPR trainings [2]. The ability to track OHCA data improved significantly after participation in the SaveMIHeart collaborative and the Cardiac Arrest Registry to Enhance Survival (CARES). The data, in turn, was utilized to implement swift modifications in OHCA protocols.
The COVID-19 pandemic drastically altered the landscape of OHCA in Detroit - an area covering 142.9 miles where approximately 670,000 people reside [2,3]. The first positive case of COVID-19 was identified in Detroit, Michigan on March 10th, 2020. One day later, the World Health Organization (WHO) declared COVID-19 a pandemic [4]. By March 30th, 2020, Michigan had the fourth highest death toll due to the virus in the nation [5]. Over 80% of cases in Michigan were from the city of Detroit [5]. Detroit had 1666 COVID-19 cases per 100,000 population and 208 COVID-19 deaths per 100,000 [6].
The International Liaison Committee on Resuscitation recommends a proper balance between early resuscitation and risk of COVID-19 transmission to rescuers [7]. Effects of changes to resuscitation protocol in OHCA during the COVID-19 era are not clear as the literature remains sparse. Therefore, we conducted a rigorous, strict comparison of patients with non-traumatic OHCA during the COVID-19 period to the same time frame in the previous year. The primary endpoint was to determine if there were any changes in pre-hospital ROSC in the pandemic period. We also aimed to identify changes in demographics, comorbidities, bystander CPR, and field termination in hopes of providing insight into management of OHCA during the COVID-19 pandemic and concurrently update the unique situation in Detroit, Michigan.
2. Methods
Data for the current study was obtained from the Detroit Cardiac Arrest Registry including CARES data. CARES is a component of the Detroit Cardiac Arrest Registry and was reviewed by the Wayne State University Institutional Review Board (IRB) as exempt.
To measure the outcomes and progress of patients who experience OHCA, the Center for Disease Control and Prevention collaborated with the Emory University School of Medicine in 2004 to develop a national registry of OHCA data (CARES). CARES adopts Utstein-style reporting guidelines, which provide a standard, structured framework to collect and report data of patients with cardiac arrest. CARES is one of the largest OHCA registries and quality improvement programs in the world, with >1800 hospitals and 1400 EMS agencies from 23 participating states.
The study included patients 18 years and older with non-traumatic OHCA and excluded patients if no resuscitation was attempted or the arrest was deemed to be traumatic in nature in the city of Detroit. The CARES database excludes patients that did not undergo resuscitation measures. Every OHCA patient is extracted from the Detroit EMS database and automatically uploaded into CARES. The site CARES coordinator performs a quality check to ensure any missing arrests have been input and reviews every OHCA to confirm data were correctly transferred from the EMS database. Data are reviewed by the site CARES coordinator and by the physicians leading the project and performing the analysis.
The Detroit Fire Department functions with 6 non-transporting squads and 27 fire engines, all licensed at the medical first-responder level. There are 27 Basic Life Support (BLS) ambulances and 9 Advanced Life Support (ALS) ambulances operated by the fire department. There are also 8 ambulances provided by 4 private companies that provide coverage during peak hours and are appropriately dispatched by the city. Each call for service that is prioritized at the echo or delta level dispatches the nearest ambulance and MFR apparatus. Preferential dispatch of ALS units is absent because of the small number available and the size of the response area [2].
Cardiac arrest care is performed under medical control authority protocols and all cases where resuscitation is attempted are included in the Detroit CARES data, including those that were terminated in the field. There are standard dead-on-scene protocols when no resuscitation will be attempted, in which case the patients were not included in the dataset. There are advanced life support (ALS) and basic life support (BLS) protocols for cardiac arrest with BLS units performing 3 initial cardiopulmonary resuscitation (CPR) cycles (6 min) on scene before preparing for transport and calling medical control. In addition, patients not achieving ROSC must have resuscitation efforts continued for 30 min, at which point medical control can be contacted for termination of resuscitation. The cardiac arrest protocols have been adjusted due to COVID-19.
In response to the pandemic, the state of Michigan created state model protocols, which were adopted by the Detroit Medical Control Authority (DEMCA) [8]. These protocols modified resuscitation in an attempt to enhance safety for first responders while maintaining a high level of patient care. These protocols included limiting airway interventions to basic life support (BLS) procedures. Bag-valve-mask and supraglottic airways were the only airway interventions allowed that did not warrant a call to medical control for permission. In addition, 10 min of CPR without return of spontaneous circulation (ROSC) would warrant a call to medical control for possible termination of resuscitation, and transportation of a patient would only occur if ROSC was sustained for more than 5 min.
OHCA characteristics were recorded retrospectively. ROSC is defined as whether pulse was sustained for 20 or more minutes or if a pulse was achieved prior to end of EMS care. Response time is calculated as the time of the ambulance on scene subtracted by the time EMS arrived at the patient side. The current analysis encompasses the time period between the first positive case of COVID-19 in Detroit (March 10th, 2020) and April 30th, 2020. April 30th, 2020 was chosen as the end date of the peak as arrests declined in May and June. The comparison involves the same time frame from 2019 as our non-pandemic reference. Patient demographics, location of arrests, initial rhythm, comorbidities, bystander CPR and field termination were compared between the two time points.
Descriptive statistics were utilized to compare characteristics of arrests in 2020 compared to 2019. Univariate comparisons for continuous and categorical data were analyzed as mean difference (MD) or odds ratio (OR), respectively, with 95% confidence intervals (95% CI). Logistic regression was used to compare the odds of ROSC for 2019 vs. 2020, after adjusting for age, gender, race, BLS vs ALS, shockable vs. unshockable rhythm, presence vs. absence of bystander CPR, and the arrest being unwitnessed vs. witnessed by bystander vs. witnessed by EMS. All data were analyzed using the R platform (Rstudio V.1.2.5). Requests for access to the study's analytical code and data can be directed to the corresponding author.
3. Results
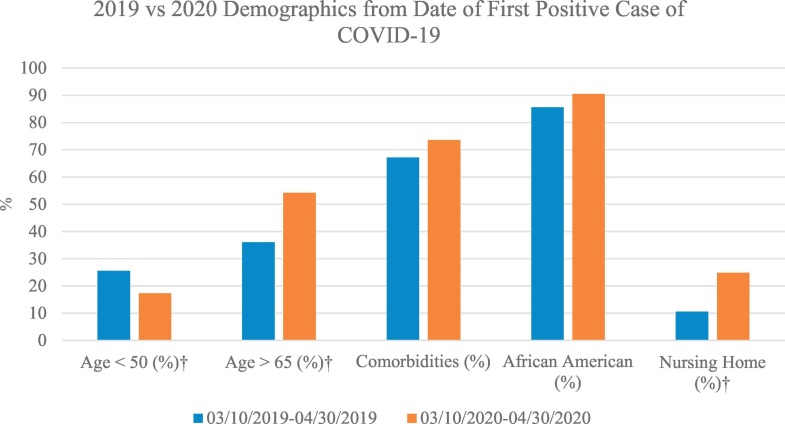
A total of 490 patients were treated by EMS for OHCA. Traumatic arrests numbered 10 and 9 in 2019 and 2020, respectively, leaving 471 patients in the analysis. 180 OHCA occurred from March 10th, 2019 – April 30th, 2019 whereas 291 OHCA occurred from the same dates in 2020 (62% absolute increase). Patients in 2020 vs. 2019 were older (mean difference + 6; 95% CI: +2.4 to +9.5). No statistical differences were observed in gender, race, pre-existing conditions or witnessed / unwitnessed arrest by year. Table 1 and Fig. 1 displays the characteristics of patients with non-traumatic out-of-hospital cardiac arrests who underwent EMS resuscitation.
Table 1.
Patient demographics and medical history, out of hospital cardiac arrests in the pandemic period (2020) vs. the pre-pandemic period (2019).
| Characteristic | 2020 (n = 291) | 2019 (n = 180) | Odds Ratio or Mean Difference (95% CI) |
|---|---|---|---|
| Age (years)⁎ | 64.5 (18.1) | 58.5 (19.8) | +6 (+2.4 to +9.5) |
| Gender = Female | 43% (126) | 48% (87) | 0.82 (0.56–1.19) |
| Race/Ethnicity = Non-White | 92% (267) | 88% (158) | 1.55 (0.83–2.87) |
| Heart Disease | 25% (72) | 18% (33) | 1.46 (0.93–2.34) |
| Diabetes | 24% (69) | 17% (30) | 1.55 (0.97–2.52) |
| Hypertension | 34% (100) | 33% (60) | 1.05 (0.71–1.56) |
| Renal Disease | 12% (34) | 9% (16) | 1.34 (0.73–2.59) |
| Respiratory Disease | 14% (40) | 18% (32) | 0.74 (0.44–1.23) |
| Stroke | 5% (15) | 6% (11) | 0.83 (0.37–1.92) |
CI: confidence interval.
p < 0.05.
Fig. 1.
Effects of the COVID-19 Pandemic on OHCA Care in Detroit.
OHCA demographics before the pandemic period (2019) and during the pandemic (2020).
Demographics of out-of-hospital cardiac arrest (OHCA) were compared as an absolute percentage (%) before the pandemic period (2019) and during the pandemic (2020) in Detroit, Michigan. †p < 0.05.
OHCA = out-of-hospital cardiac arrest.
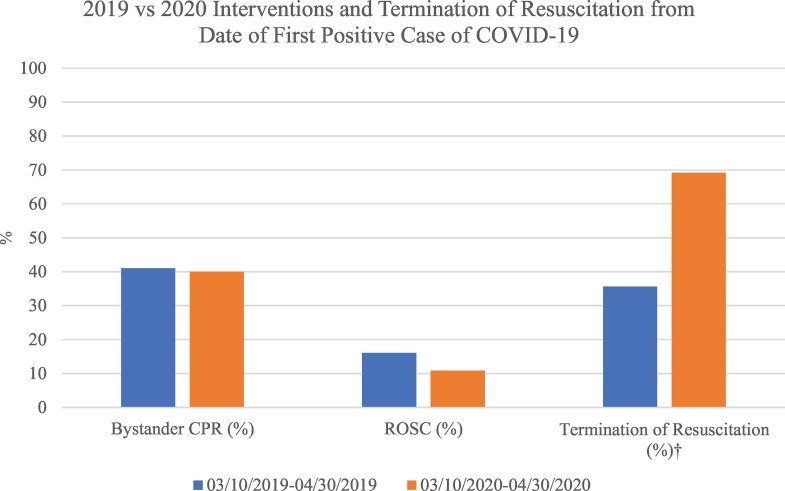
Compared to 2019, patients in 2020 were more likely to arrest in a nursing home (OR = 2.42; 95% CI: 1.42–4.31) and less likely to arrest in a public place (OR = 0.47; 95% CI: 0.25–0.88). In 2020 arrests were more likely to be terminated in the field (OR = 2.36; 95% CI: 1.36–4.07), and less likely to be a BLS response (OR = 0.68; 95% CI: 0.47–0.99). No differences were observed in bystander CPR, rhythms and ROSC. Table 2 and Fig. 2 displays additional interventions and rhythms for patients who underwent EMS resuscitation during each period.
Table 2.
Prehospital characteristics and outcomes, out of hospital cardiac arrests in the pandemic period (2020) vs. the pre-pandemic period (2019).
| Characteristic | 2020 (n = 291) | 2019 (n = 180) | Odds Ratio or Mean Difference (95% CI) | |
|---|---|---|---|---|
| EMS Type⁎ | Advanced Life Support (ALS) | 49% (142) | 39% (71) | Ref |
| Basic Life Support (BLS) | 51% (149) | 61% (109) | 0.68 (0.47–0.99) | |
| ALS Initial Rhythm | Asystole/Idioventricular/PEA | 94% (133) | 92% (65) | Ref |
| Ventricular Tachycardia/Ventricular Fibrillation | 6% (9) | 8% (6) | 0.73 (0.25–2.30) | |
| BLS Initial Rhythm | Unknown Unshockable Rhythm | 90% (134) | 87% (95) | Ref |
| Unknown Shockable Rhythm | 10% (15) | 13% (14) | 0.76 (0.35–1.68) | |
| Unshockable vs. Shockable | Asystole/Idioventricular/PEA or Unknown Unshockable | 92% (267) | 89% (160) | Ref |
| Ventricular Tachycardia/Ventricular Fibrillation or Unknown Shockable | 8% (24) | 11% (20) | 0.72 (0.38–1.36) | |
| Time To Patient | Ambulance On Scene To EMS At Patient Side (Min) |
1.7 (2.6) | 1.6 (1.7) | −0.2 (−0.5 to +0.2) |
| Witnessed | Unwitnessed Arrest | 55% (161) | 52% (94) | Ref |
| Arrest Witnessed by EMS | 14% (42) | 10% (18) | 1.36 (0.75–2.55) | |
| Arrest Witnessed by Bystander | 30% (88) | 38% (68) | 0.76 (0.50–1.14) | |
| Bystander CPR | Yes | 40% (117) | 41% (73) | Ref |
| No | 60% (174) | 59% (107) | 1.01 (0.69–1.48) | |
| Arrest Location⁎ | Home/Residence | 69% (201) | 74% (133) | Ref |
| Nursing Home | 24% (70) | 11% (19) | 2.42 (1.42–4.31) | |
| Public Place | 7% (20) | 16% (28) | 0.47 (0.25–0.88) | |
| End of the Event⁎ | Pronounced Dead in ED | 14% (41) | 17% (31) | Ref |
| Termination of Resuscitation in the Field | 69% (200) | 36% (64) | 2.36 (1.36–4.07) | |
| Ongoing Resuscitation in ED | 17% (50) | 47% (85) | 0.45 (0.25–0.80) | |
| ROSC | Yes | 11% (32) | 16% (29) | Ref |
| No | 89% (259) | 84% (151) | 1.56 (0.90–2.68) |
EMS = emergency medical services; ALS = advanced life support; BLS = basic life support; PEA = pulseless electrical activity; CPR = cardiopulmonary resuscitation; ED = emergency department; ROSC = return of spontaneous circulation; CI = confidence interval.
p < 0.05.
Fig. 2.
Effects of the COVID-19 Pandemic on OHCA Care in Detroit.
OHCA interventions and termination of resuscitation before the pandemic period (2019) and during the pandemic (2020).
Bystander CPR return of spontaneous circulation (ROSC) and termination of resuscitation of out-of-hospital cardiac arrests (OHCA) were compared as an absolute percentage (%) before the pandemic period (2019) and during the pandemic (2020) in Detroit, Michigan.
†p < 0.05.
OHCA = out-of-hospital cardiac arrest; CPR = cardiopulmonary resuscitation; ROSC = return of spontaneous circulation.
11% of patients achieved prehospital ROSC in 2020 compared to 16% in 2019 (p = 0.14, Table 2). Before adjusting for confounders, BLS response (OR = 0.42; 95%CI: 0.24–0.73) and arrest in a nursing home (OR = 0.44; 95%CI: 0.16–0.99) were associated with lower odds of achieving ROSC (Table 3 ). ROSC was significantly more likely before adjustment with a shockable initial rhythm (OR = 3.32, 95% CI: 1.57–6.69) and if the arrest was witnessed by a bystander (OR = 2.34. 95% CI: 1.26–4.42) or by EMS personnel (OR = 3.9; 95%CI: 1.83–8.22). After adjusting with logistic regression for age, gender, race, BLS vs ALS, shockable or unshockable rhythm, bystander CPR, and witnessed vs. unwitnessed arrest, there was no significant difference in the odds of ROSC in 2020 vs 2019 (OR = 0.61; 95% CI: 0.34–1.11). By contrast, BLS response (OR = 0.38; 95% CI: 0.21–0.70), unshockable rhythm (OR = 0.32; 95% CI: 0.14–0.72), and arresting in the presence of EMS (OR = 2.41; 95% CI: 1.02–5.77) all remained significant predictors of ROSC after logistic regression (Table 4 ).
Table 3.
Patient demographics, medical history, arrest characteristics, and year (pre-pandemic/2019 vs. pandemic/2020) for pre-hospital patients achieving or not achieving ROSC.
| Characteristic | No ROSC (n = 410) | ROSC (n = 61) | Odds Ratio or Mean Difference (95% CI) | |
|---|---|---|---|---|
| Year (During March–April) | 2019 | 37% (151) | 48% (29) | Ref |
| 2020 | 63% (259) | 52% (32) | 0.64 (0.37–1.12) | |
| Age | Years | 62.4 (18) | 60.9 (22) | −1.5 (−7.4 to +4.4) |
| Gender | Male | 55% (225) | 54% (33) | Ref |
| Female | 45% (185) | 46% (28) | 1.03 (0.60–1.77) | |
| Race/Ethnicity | White | 10% (40) | 10% (6) | Ref |
| Non-White | 90% (370) | 90% (55) | 0.97 (0.42–2.68) | |
| Heart Disease | Yes | 22% (89) | 26% (16) | Ref |
| No | 88% (321) | 74% (45) | 0.78 (0.43–1.48) | |
| Diabetes | Yes | 21% (87) | 20% (12) | Ref |
| No | 79% (323) | 80% (49) | 1.09 (0.57–2.24) | |
| Hypertension | Yes | 34% (140) | 33% (20) | Ref |
| No | 66% (270) | 67% (41) | 1.06 (0.60–1.91) | |
| Renal Disease | Yes | 11% (45) | 8% (5) | Ref |
| No | 89% (410) | 92% (56) | 1.35 (0.56–4.08) | |
| Respiratory Disease | Yes | 15% (60) | 20% (12) | Ref |
| No | 85% (350) | 80% (61) | 0.70 (0.36–1.44) | |
| Stroke | Yes | 6% (23) | 5% (3) | Ref |
| No | 94% (387) | 95% (58) | 1.10 (0.37–4.94) | |
| EMS Type⁎ | Advanced Life Support (ALS) | 42% (174) | 39% (39) | Ref |
| Basic Life Support (BLS) | 58% (236) | 61% (22) | 0.42 (0.24–0.73) | |
| Unshockable vs. Shockable† | Asystole/Idioventricular/PEA or Unknown Unshockable | 92% (379) | 79% (48) | Ref |
| Ventricular Tachycardia/Ventricular Fibrillation or Unknown Shockable | 8% (31) | 21% (13) | 3.32 (1.57–6.69) | |
| Witnessed⁎ | Unwitnessed Arrest | 57% (235) | 33% (20) | Ref |
| Arrest Witnessed by EMS | 11% (45) | 25% (15) | 3.90 (1.83–8.22) | |
| Arrest Witnessed by Bystander | 32% (130) | 43% (26) | 2.34 (1.26–4.42) | |
| Bystander CPR | Yes | 40% (164) | 43% (26) | Ref |
| No | 60% (246) | 57% (35) | 0.90 (0.52–1.56) | |
| Arrest Location⁎ | Home/Residence | 70% (286) | 79% (48) | Ref |
| Nursing Home | 20% (83) | 10% (6) | 0.44 (0.16–0.99) | |
| Public Place | 10% (41) | 11% (7) | 1.03 (0.40–2.32) |
EMS = emergency medical services; PEA = pulseless electrical activity; CPR = cardiopulmonary resuscitation; ROSC = return of spontaneous circulation; CI = confidence interval.
p < 0.05.
Table 4.
Logistic regression for the odds of ROSC in the pre-pandemic (2019) and pandemic (2020) periods, adjusted for suspected confounders.
| Predictor | Adjusted Odds Ratio (95% CI) for Obtaining Return of Spontaneous Circulation |
|---|---|
| Year = 2020 | 0.61 (0.34–1.11) |
| Age (per 10 year increase) | 0.99 (0.86–1.15) |
| Gender = Male | 0.87 (0.49–1.56) |
| Arrest Location = Nursing Homea | 0.56 (0.19–1.45) |
| Arrest Location = Public Placea | 0.92 (0.34–2.21) |
| EMS Type = BLS | 0.38 (0.21–0.70)⁎ |
| Initial Rhythm = Unshockable | 0.32 (0.14–0.72)⁎ |
| Bystander CPR = Yes | 1.70 (0.86–3.36) |
| Race = Whiteb | 0.91 (0.31–2.29) |
| Arrest Witnessed By EMSc | 2.41 (1.02–5.77)⁎ |
| Arrest Witnessed By Bystanderc | 0.62 (0.31–2.29) |
EMS = emergency medical services; PEA = pulseless electrical activity; CPR = cardiopulmonary resuscitation; ROSC = return of spontaneous circulation; CI = confidence interval.
p < 0.05.
Compared to location of Home/Residence.
Compared to Non-White Race.
Compared to unwitnessed cardiac arrest.
4. Discussion
The consequences of OHCA during coronavirus disease of 2019 (COVID-19) are evident on a global level. COVID-19 is a global pandemic affecting nearly 185 countries and infecting greater than 3 million people worldwide as of April 28, 2020 with more than 210,000 deaths related to the virus [9]. Northern Italy reported a 58% increase in OHCA during the current pandemic in comparison to the same time period in 2019 [10]. In New York City, there was a 10-fold increase in OHCA during COVID-19 compared to the equivalent time period in 2019 [11]. France indicated a two-times increase in OHCA with a reduction in survival during the pandemic compared to the same time period in previous years [12]. Rate of OHCA and corresponding treatments and outcomes are suspect to a high degree of variability due to geographic disparities [13]. The variability is found at a state and national level prior to the pandemic and is further illuminated amidst the COVID-19 pandemic [[14], [15], [16], [17], [18], [19]].
There was a 62% increase in OHCA cases in the city of Detroit during the peak of the COVID-19 pandemic compared to the previous period. A number of factors potentially could have made Detroiters particularly susceptible to an increase in OHCA during the pandemic. Risk factors for illness severity with the virus included comorbidities, older age and minority status/ethnicity [3]. A majority of the Detroit population are of African American race, a large proportion have multiple comorbidities, and 36% live in poverty [3,[20], [21], [22]].
Indirect effects of COVID-19 could have also affected the increase in OHCA. In Hong Kong, patients with STEMI's delayed receiving medical care and there were also delays in evaluating patients once they arrived at the hospital due to COVID-19 rules and regulations [23]. In Ontario, Canada there was a 20% drop in the number of code strokes after the first COVID-19 case appeared and a similar decrease in clinic referrals due to changed hospital policies [24]. Similar declines in overall Emergency Department visits were seen in the United States when compared to a 4-week interval in 2019 [25]. The indirect effects of statewide stay-at-home orders mean that individuals may be more likely to refrain from essential health care due to concern of contracting the contagious virus.
Patient consultations and outpatient visits have been postponed because of fear of exposure and risk of contamination. The emergence of telehealth for follow-ups and emergency medical services have garnered attention in the period of the pandemic. Low priority cases that are seen by a physician may be advised not to present to the hospital unless individuals require emergent medical attention. Patients were also frequently discharged from emergency departments with suspected COVID-19 but no confirmatory tests were available [26,27].
While we could not directly assess if patients avoided or were diverted from hospital care, we did note that a larger proportion of cardiac arrests occurred at home compared to public places in 2020 vs. 2019. While this is almost certainly due to stay-at-home orders, this change in the location of arrests did not seem to have an effect of the odds of ROSC. The psychological stress of a global pandemic, including fear of contracting the virus, could potentially have been expected to result in a lower rate of bystander CPR (a known predictor of favorable OHCA outcomes) [10,12]. However, we did not note such an effect in our city (Table 2, Table 4) which was consistent with bystander CPR data in King County, Washington [28]. It is important to acknowledge that although we did not find significant effects of ROSC due to increased OHCA rates, the city of Detroit as well as country-wide health systems should reinforce the cruciality of seeking urgent medical care for conditions, such as myocardial infarction, that could result in serious harm and death.
The crisis standard of care COVID-19 CPR protocol instituted by our medical control authority included the ability to request termination of resuscitation in suspected COVID-19 cases after 10 min of CPR without ROSC. The previous protocol required 30 min of CPR without ROSC prior to requesting termination. As a result, termination of resuscitation rates nearly doubled in the time of the pandemic (Fig. 2). This is not surprising, since resuscitations were terminated up to 20 min earlier in 2020 rather than 2019.
A decreased chance of ROSC could have been expected due to this protocol change, as well as several other potential effects of the pandemic. First, previous studies have reported high rates of respiratory arrests due to COVID-19 [12,29], which in turn could result in more non-shockable rhythms. Non-shockable rhythms are associated with higher mortality and lower survival to hospital discharge [[30], [31], [32]]. However, no significant differences in initial rhythm were found in our population between 2019 and 2020. Although we did not find significant differences in initial rhythm, there may have been small or even clinically significant differences in both shockable rhythms and non-shockable rhythms which we were underpowered to detect. However, the absolute point estimate differences in ROSC and shockable vs. non-shockable rhythms are nevertheless lower than what has been observed in similar studies of other municipalities, including an analysis of the national CARES database [14]. Detroit may have had an attenuated effect on rate of initial rhythms and ROSC compared to other municipalities because baseline rates of non-shockable rhythms were already high, and baseline ROSC was lower, compared to national averages [14]. France reported a significant decrease in shockable rhythms. On the other hand, New York City reported a decrease in ventricular rhythms and an increase in asystole as the presenting rhythm similar to our EMS system [11,12]. Second, increased PPE requirements and caution in the COVID-19 era could have had an adverse effect on outcomes due to an increase in EMS on-scene to EMS at patient time. Nevertheless, we observed no such difference in time despite these changes, even with the modified resuscitation protocol. By the same token, a potential increase in scene time may have been mitigated by the modification in termination of resuscitation efforts. Third, given a lower rate of arrests in public places, one may have expected a lower rate of bystander CPR, which is associated with increased rates of ROSC [33,34]. This too was not significantly different between years. Fourth, as more people were at home due to the stay-at-home orders, access to an AED may have been less likely compared to OHCA in a public place. Nevertheless, no significant difference in the 2019 vs. 2020 rates of ROSC were noted, even after adjusting for noted confounders.
The noted increase in cardiac arrests in Detroit is consistent with the experience of other cities hit hard in the early months of the pandemic, but unlike other cities we did not note a significant decrease in ROSC [7,35,36]. In New York City, which experienced a peak in COVID-19 cases roughly contemporaneous with Detroit, a similarly designed study showed a significant decrease in ROSC and increase in non-shockable rhythms attributed to the pandemic. It is possible that our study was underpowered to detect a difference in ROSC or non-shockable rhythms, which could account for this discrepancy [14]. Although this may have been underpowered, there was nevertheless a clinically significant difference between absolute change in ROSC in our data compared to other cities such as NY, which had a 14% decrease, and the country, which had an 18% decrease, as an average [11,14]. Baseline differences in OHCA care and outcomes are markedly heterogenous between localities prior to the pandemic. By extension, the effect of the pandemic on those outcomes in different localities would also be expected to differ. In other words, a pandemic which increased non-shockable rhythms and decreased rates of ROSC overall may have had greater effects in places where those metrics were already more favorable, and less effect in places like Detroit. Analysis of the baseline differences between the Detroit and New York OHCA populations would seem to support this interpretation. Notably, the pre-COVID rate of prehospital ROSC in New York City was 35% compared to just 16% in Detroit [11]. Similarly, the pre-COVID rate of ALS shockable rhythms in New York was 11–14%, but just 8% in Detroit [11]. Though Detroit has made strides in EMS OHCA care, the previous criteria for termination of resuscitation may have favored a population less likely to achieve ROSC regardless of COVID-19. Put differently, the initiation of an early termination protocol in response to COVID-19 could have aligned patient selection for termination of resuscitation in Detroit more closely towards what was already occurring in other cities. The fact that an earlier termination protocol was initiated in Detroit, a significant increase (over double) in terminations was observed, and ROSC rates were nevertheless similar, would seem to further support this interpretation.
Objective factors such as bystander CPR, as well as subjective ethical concerns should be evaluated further. The medical control physician is the decision maker on whether crisis standards of care are appropriate, as there are no specific triggers identified in the state model protocol to initiate crisis standards of care. The day to day situation of patient volume during the pandemic was extremely variable. Assessing attitudes and aggressiveness of care of responders and medical control physicians is worth additional study.
Patients may be fearful of contracting the virus in the ambulance or a hospital setting and therefore refuse care. The refusal of care could lead to a missed diagnosis or undiagnosed condition, eventually contributing to an out-of-hospital cardiac arrest. Adjudicating each refusal and adjudicating patients who arrive to the hospital with no COVID-19 testing data will be beneficial to determine whether there are other factors to consider in out-of-hospital cardiac arrests during this time. Furthermore, linkage to COVID-19 testing data will be an important step for further understanding our data set and comparing which patients were affected by COVID-19 prior to an out-of-hospital cardiac arrest.
5. Limitations
There are several limitations to our data that are shared among other reports of out-of-hospital cardiac arrest in the COVID-19 era. First, the out-of-hospital cardiac arrests discussed in our study cannot be directly or indirectly attributed to COVID-19 due to numerous complex factors. Only rarely was post-mortem testing conducted, therefore, it will most likely be difficult to definitively prove that COVID-19 was related to deaths in out-of-hospital cardiac arrests. However, our noted increase in OHCA is consistent with what has been observed in other cities and countries during local pandemic surges [11]. Additionally, we did not include patients who did not have resuscitation attempted as the CARES database excludes these patients from the registry. Based on preliminary findings from our EMS database, there is also an increase in patients with no resuscitation attempted which warrants further exploration. Second, our results are not generalizable to all other urban areas in the U.S. with sufficiently different socioeconomic, demographic, geographic, and population health characteristics to Detroit. However, we see a large strength of the study as this exact finding: Detroit's rate of ROSC as a function of the pandemic may have been less affected than other localities precisely because of Detroit's baseline status as an outlier in U.S. OHCA outcomes at baseline. Other municipalities which are more similar to Detroit in baseline rates of ROSC and non-shockable rhythms may more closely reflect the results of our analysis than those of places like New York, or of the CARES database on average. This may help such municipalities more closely target their own changes in termination protocols to local situations, by acknowledging the nuance of the pandemic's effects as a function of local baselines in OHCA care. We were unable to directly evaluate the relationship between these characteristics across specific time periods coinciding with COVID-19 disease burden (e.g. standardized by weekly new case rates) or by geographic distributions within the city. Third, all retrospective, registry-based data has limitations, including potential for data entry errors, missing data, and other reporting biases from the organizations providing data to CARES. While reporting bias and/or missing data can be an issue with large databases, in general, we noted no fields in the CARES database left unanswered and CARES has explicit, objective definitions for their reporters to record data appropriately to mitigate potential biases. Fourth, we compared only a single timeframe (March–April 2019) to the COVID-19 era. While we can identify no reason that 2019 may have differed from previous years that could have been used as alternative baselines for comparison, we cannot exclude this possibility. Finally, while we noted no change in the rate of ROSC between years after adjusting for known confounders, our analysis may have been underpowered to detect modest differences. However, as discussed, the absolute 2019 vs. 2020 differences in ROSC and shockable vs. non-shockable rhythms were less than those observed in other places and may reflect heterogenous effects of the pandemic on OHCA outcomes as a function of baseline differences between Detroit and other places.
6. Conclusion
COVID-19 appears to have had a profound effect reflected not only in the number of infected cases, but also the number of deaths due to out-of-hospital cardiac arrests. The 62% increase in OHCA compared to the same time frame in 2019 can likely be attributed to the pandemic and adds to an expanding body of literature suggesting an increase in pre-hospital death during the pandemic [[10], [11], [12]]. In addition to the current literature, we found that arrests were more likely to occur in nursing homes and less likely to occur in public places in 2020, compared to 2019. Furthermore, we report a statistically significant difference in age; however, other demographic characteristics sustained similarity between the time periods. Interestingly, our bystander CPR rates did not wane in the pandemic time frame.
The unpredictable and rapidly evolving health crisis presents a unique challenge in the pre-hospital setting. Implementation of resuscitation protocols that provide a balance between optimal patient care and mitigating exposure to rescuers are necessary to manage such a crisis.
The modifications in resuscitation protocol due to the effects of COVID-19 led to an increase in field termination of resuscitation. Notably, ROSC rates in Detroit remained similar, despite a shortened CPR time protocol change; however, our sample size may be underpowered to conclude the absence of a statistically significant difference.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclaimers
None.
Declaration of Competing Interest
None.
Acknowledgements
The authors would like to acknowledge the Detroit Fire Department and all the providers that support prehospital care and are serving on the frontlines in the city of Detroit. The views expressed in this article are the authors' and do not reflect the official position of the Detroit city government or its fire department.
References
- 1.Dunne R.B., Compton S., Zalenski R.J., Swor R., Welch R., Bock B.F. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007;72:59–65. doi: 10.1016/j.resuscitation.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 2.May S., Zhang L., Foley D., et al. Improvement in non-traumatic, out-of-hospital cardiac arrest survival in Detroit from 2014 to 2016. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.009831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Budzynska K., West P., Savoy-Moore R.T., Lindsey D., Winter M., Newby P. A food desert in Detroit: associations with food shopping and eating behaviours, dietary intakes and obesity. Public Health Nutr. 2013;16:2114–2123. doi: 10.1017/S1368980013000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Couper K., Taylor-Phillips S., Grove A., et al. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020;151:59–66. doi: 10.1016/j.resuscitation.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chapman M., Bosman J., Eligon J. New York Times; 2020. Coronavirus Sweeps Through Detroit, a City That Has Seen Crisis Before.https://www.nytimes.com/2020/03/30/us/coronavirus-detroit.html [accessed 4 October 2020] [Google Scholar]
- 6.COVID-19 Dashboard. 2020. https://codtableau.detroitmi.gov/t/DHD/views/CityofDetroit-PublicCOVIDDashboard/TimelineCasesDashboard?%3AisGuestRedirectFromVizportal=y&%3Aembed=y; [accessed 15 October 2020]
- 7.Perkins G.D., Couper K. COVID-19: long-term effects on the community response to cardiac arrest? Lancet Public Health. 2020;5:e415–e416. doi: 10.1016/S2468-2667(20)30134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bureau of EMS, Trauma & Preparedness Michigan *EMERGENCY* COVID-19 RESPONSE CARDIAC ARREST IN A PATIENT WITH SUSPECTED OR CONFIRMED COVID-19. 2020. https://www.michigan.gov/documents/mdhhs/14.08_nCoV_Resuscitation_4.24.2020_688755_7.pdf; [accessed 15 July 2020]
- 9.Clerkin K.J., Fried J.A., Raikhelkar J., et al. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 10.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5:1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coute R.A., Shields T.A., Cranford J.A., et al. Intrastate variation in treatment and outcomes of out-of-hospital cardiac arrest. Prehosp Emerg Care. 2018;22:743–752. doi: 10.1080/10903127.2018.1448913. [DOI] [PubMed] [Google Scholar]
- 14.Chan P.S., Girotra S., Tang Y., Al-Araji R., Nallamothu B.K., McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.6210. Published online November 14, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nichol G. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girotra S., van Diepen S., Nallamothu B.K., et al. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carr B.G., Kahn J.M., Merchant R.M., Kramer A.A., Neumar R.W. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80:30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Liu J.M., Yang Q., Pirrallo R.G., Klein J.P., Aufderheide T.P. Hospital variability of out-of-hospital cardiac arrest survival. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2008;12:339–346. doi: 10.1080/10903120802101330. [DOI] [PubMed] [Google Scholar]
- 19.Sasson C., Magid D.J., Chan P., et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.QuickFacts Detroit Michigan Population Estimates, July 1, 2019. 2019. https://www.census.gov/quickfacts/fact/table/detroitcitymichigan,MI/PST045219 [accessed 15 October 2020]
- 21.QuickFacts Detroit Michigan Population, Percent Change - April 1–2010 to July 1, 2019. 2019. https://www.census.gov/quickfacts/fact/table/detroitcitymichigan/PST120219;
- 22.Smitherman H.C., Kallenbach L., Aranha A.N. Detroit Area Agency on Aging; 2020. Dying Before Their Time III: 19-year (1999–2017) comparative analysis of excess mortality in Detroit (PSA 1-A)https://www.docdroid.com/w7ygR0O/dying-before-their-time-iii-daaa-2020-final-pdf; [accessed 5 August 2020] [Google Scholar]
- 23.Tam C.-C.F., Cheung K.-S., Lam S., et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bres Bullrich M., Fridman S., Mandzia J.L., et al. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci J Can Sci Neurol. 2020;47:693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whitmer G., Gordon R. Department of Health and Human Services. 2020. https://www.michigan.gov/documents/lara/Medical_Provider_Letter_Disparities_Final_Formatted_042020_687891_7.pdf; [accessed 4 October 2020]
- 27.Sharfstein J.M., Becker S.J., Mello M.M. Diagnostic testing for the novel coronavirus. JAMA. 2020;323:1437. doi: 10.1001/jama.2020.3864. [DOI] [PubMed] [Google Scholar]
- 28.Sayre M.R., Barnard L.M., Counts C.R., et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander cardiopulmonary resuscitation. Circulation. 2020;142:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 29.Scquizzato T., Landoni G., Paoli A., et al. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: a systematic review. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.10.020. Published online October 29, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Engdahl J., Bång A., Lindqvist J., Herlitz J. Factors affecting short- and long-term prognosis among 1069 patients with out-of-hospital cardiac arrest and pulseless electrical activity. Resuscitation. 2001;51:17–25. doi: 10.1016/S0300-9572(01)00377-X. [DOI] [PubMed] [Google Scholar]
- 31.Peberdy M.A., Kaye W., Ornato J.P., et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of cardiopulmonary resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/S0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 32.Meaney P.A., Bobrow B.J., Mancini M.E., et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 33.Xiong Y., Zhan H., Lu Y., et al. Out-of-hospital cardiac arrest without return of spontaneous circulation in the field: who are the survivors? Resuscitation. 2017;112:28–33. doi: 10.1016/j.resuscitation.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 34.Hasselqvist-Ax I., Riva G., Herlitz J., et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 35.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;4132:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shekhar A.C., Mercer C., Blumen I., Narula J. Suboptimal rates of return of spontaneous circulation with prehospital CPR in the COVID-19 era. Resuscitation. 2020;154:50–51. doi: 10.1016/j.resuscitation.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]