Abstract
Background
In 2016, Oregon introduced a policy to improve back pain treatment among Medicaid enrollees by expanding benefits for evidence-based complementary and alternative medical (CAM) services and establishing opioid prescribing restrictions.
Objective
To examine changes in CAM utilization following the policy and variations in utilization across patient populations.
Design
A retrospective study of Oregon Medicaid claims data, examining CAM therapy utilization by back pain patients pre- vs post-policy. We used an interrupted time series analysis to evaluate changes in CAM use and examined the association between patient characteristics and CAM use post-policy using linear regression models.
Participants
Adult Medicaid patients with back pain.
Intervention
The Oregon Medicaid back pain policy, administered through Coordinated Care Organizations (CCOs).
Main Measures
Use of CAM services.
Key Results
Use of any CAM service increased from 7.9% (95% CI 7.6–8.2%) prior to the policy to 30.9% (95% CI 30.4–31.3%) after the policy. Acupuncture increased from 0.3 to 5.6%, chiropractic from 0.3 to 11.1%, massage from 1.6 to 14.8%, PT/OT from 6.0 to 17.7%, and osteopathic from 1.4 to 1.9%. Interrupted time series showed an overall increase in proportion of back pain patients who used CAM service following the policy. Among those who accessed CAM, the policy did not appear to increase the number of services used. In the post period, CAM services were accessed more often by female and older enrollees and urban populations. Black, American Indian/Alaska Native, and Hispanic enrollees were less likely to access CAM services; for Black enrollees, this was true for all types of services.
Conclusions
CAM service utilization increased among back pain patients following implementation of Oregon’s policy. There was significant heterogeneity in uptake across service types, CCOs, and patient subgroups. Policymakers should consider implementation factors that might limit impact and perpetuate health disparities.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-020-06352-6.
KEY WORDS: back pain, complementary and alternative medical therapy, policy
INTRODUCTION
Back pain is one of the most common pain complaints. Approximately one-fourth of US adults report having low back pain in the past 3 months,1 Thirteen percent report neck pain in the past 3 months,1 and 13% report chronic back pain.2 The treatment of back pain is not always focused on evidence-based therapies: for example, despite the lack of proven efficacy of opioids for non-cancer pain,3,4 its established harms, and the effectiveness of non-opioid medications such as anti-inflammatories,5 as many as 61% of patients with back pain in an ambulatory care setting receive opioids.6 In a 2016 statewide study of Medicaid participants, neck and back pain represented two of the top three complaints related to opioid prescriptions.7
A variety of other effective therapeutic options for pain management are becoming more available over time. Nonpharmacologic complementary and alternative medical (CAM) therapies have demonstrated evidence of effectiveness for the treatment of back pain and other pain conditions in terms of pain control and/or functioning.8–10 Recently, there has been general expansion of CAM services nationally.11,12 However, coverage has been inconsistent,13 and limited among Medicaid plans compared to commercial payers, partly due to the cost of the services.11
In Oregon, increased coverage of CAM services was implemented as part of a novel state policy to provide effective back pain care among Medicaid patients (Table 1) by expanding benefits for evidence-based treatments.14 Starting in July 2016, a variety of services previously only available for back pain with radiculopathy, including acupuncture, chiropractic manipulation, cognitive behavioral therapy (CBT), osteopathic manipulation, and physical and occupational therapy, were covered for any patients with back pain and expanded to include additional CAM therapy services such as yoga, intensive rehabilitation, massage, and supervised exercise therapy, as available. At the same time, the use of opioid therapy was discouraged through a number of measures, including a higher clinical threshold for initiating long-term therapy.
Table 1.
Overview of Oregon Health Plan’s 2016 Back Pain Policy
| Acupuncture, chiropractic manipulation, cognitive behavioral therapy, osteopathic manipulation, physical/occupational therapy | • Expanded coverage |
| Yoga, intensive rehabilitation, massage, exercise therapy | • Covered under some plans |
| Risk assessment prior to opioid prescribing |
• Use of a validated assessment tool (e.g., STarT Back Assessment Tool) prior to prescribing opioids • Verify risk assessment (e.g., PDMP data) |
| Restrictions on opioid prescribing for acute and subacute back pain |
• 7-day limit, short-acting only; extended use only with evidence of improved function • First-line therapies (e.g., NSAIDs) must be used first • Prescribed in conjunction with nonpharmacologic (CAM) therapies |
| Required tapering plan for patients on chronic opioids for back pain |
• Individual treatment plan must be developed by Jan 1, 2017 • End to opioid therapy no later than Jan 1, 2018 |
The Oregon back pain policy therefore represents a statewide effort to improve back pain care by shifting treatment of back pain towards CAMs. However, there are numerous reasons this policy could have null, minimal, or inconsistent effects across the Medicaid population. Benefit changes do not guarantee that practice patterns will shift, that patients will be receptive to changes in practice patterns, nor that there will be adequate numbers of local CAM providers to meet increased demand, which could limit service uptake, particularly in rural and remote areas. Further, CAM uptake in general tends to be variable based on race, ethnicity, and gender.15
Additionally, such policies may have variable impact depending on the details of the benefit strategies, which in this case were not standardized. In Oregon, Medicaid is administered through Coordinated Care Organizations (CCOs), locally governed organizations with similarities to managed care organizations (MCOs) and accountable care organizations (ACOs).16 While the state mandated general expanded coverage of these services, individual CCOs retained flexibility in tailoring benefits to their members and in how they implemented and supported specific elements of the policy, including which CAM services would be made available, and specific prior authorization criteria.
We studied whether the Oregon back pain policy led to an increase in CAM utilization among Medicaid enrollees with back pain. We examined how the policy may have had variable impact on CAM utilization across specific patient populations, based on service type, CCO, rural and urban residence, and other demographic characteristics.
METHODS
Study Design and Data Source
This was a retrospective analysis of Oregon Medicaid claims and enrollment data between January 1, 2014, and December 31, 2018. This period included 10 calendar-quarters before the Oregon back pain policy was implemented (Jan 2014–Jun 2016), and 10 calendar-quarters after the policy was implemented (Jul 2016–Dec 2018). Data were obtained from the Oregon Health Authority’s Health Systems Division.
Patient Population
We included all adult (19–64 years old) Medicaid patients with back pain at any level (cervical, thoracic, or lumbosacral), defined by ICD-9 or ICD-10 codes, within each quarter. We excluded patients with conditions that are typically exempt from opioid prescribing restrictions, including cancer-related pain, sickle cell disease, and spinal fracture and dislocation. We also excluded patients who are dually eligible for Medicaid and Medicare, as well as medical claims may be incomplete for these patients. We also excluded patients who were not enrolled in a Coordinated Care Organization (CCO), as well as quarters where a patient was enrolled in Medicaid for less than 3 of the previous 12 months.
Study Variables
Information about patient’s age, gender, race-ethnicity, and primary spoken language, as well as the CCO providing Medicaid coverage, was obtained from enrollment data. Rural or urban residence was assessed based on whether each patient’s zip code of residence was designated as rural or urban by the Oregon Office of Rural Health.17 Variables indicating 1-year history of patient health conditions were created using the Chronic Illness and Disability Payment System (CDPS), a risk adjustment system based on diagnosis codes in claims that is widely used by Medicaid programs.18
Outcome measures included complementary and alternative medicine (CAM) services, defined as a medical claim with (1) a CPT code for acupuncture, chiropractic therapy, physical and occupational therapy (PT/OT), osteopathic manipulative treatment (OMT), or massage, and (2) an ICD-9 or ICD-10 code for back pain. The primary outcome variables were coded as 1 if a patient had at least one CAM service in a given calendar-quarter, and 0 otherwise. A secondary outcome variable was the total number of CAM services received by a patient in each calendar-quarter.
Analysis
We first described statewide trends in CAM service use among the study population between 2014 and 2018. We conducted interrupted time series analyses to determine the effect of implementing the policy on CAM services, using 60 consecutive months (20 patient quarters) of data. We carried out this analysis for proportion of back pain patients using CAM services, as well as the average number of CAM services used (among those who used CAM services at least once). We then examined trends in CAM service use by CCO. CCOs with ≥ 70% urban patients were classified as urban, those with ≤ 30% were classified as rural, and all other CCOs were classified as mixed.
Subsequent analyses were restricted to observations in 2017 and 2018, after the policy was fully implemented. We compared demographic and health characteristics of patients who used any CAM services to those who did not use any CAM services during 2017–2018. We then used linear regression models to assess the association between use of CAM services and patient demographics. Coefficients and confidence intervals represent mean difference in the probability of receiving CAM services compared to a reference group (reported as percentage points). Models were adjusted for patient demographics (age, gender, race/ethnicity, primary spoken language, rural or urban residence) and health conditions, and standard errors were clustered at the member level. Finally, we examined the distribution of CAM services across providers. All data management and analyses were completed in R version 3.6.2 (2019).18
RESULTS
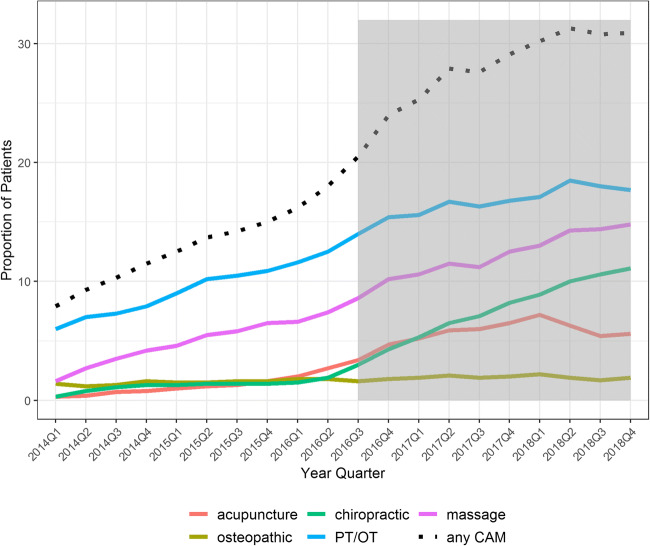
We observed increases in the proportion of Medicaid beneficiaries with back pain who used CAM therapies over the study period (Fig. 1), and this change was associated with the policy (Fig. 2). There was an increase of 23 percentage points in the proportion of back pain patients who used any CAM therapy, from 7.9% (95% CI 7.6–8.2%) to 30.9% (95% CI 30.4–31.3%). All CCOs appeared to experience some increases in CAM use (Suppl. A).
Figure 1.
Statewide proportion of back pain patients using CAM services.
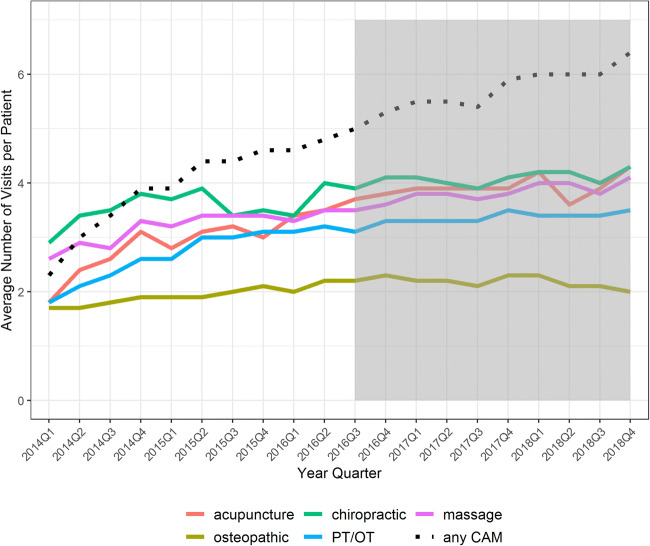
Figure 2.
Statewide average number of CAM visits among back pain patients (conditional on having at least 1 visit).
Type of Therapy
Change in uptake varied by therapy (Fig. 1) and was particularly large for acupuncture and chiropractic treatments. Results from the interrupted time series analysis (Table 2) suggest that the Oregon back pain policy was associated with a discrete (level) increase in the use of acupuncture by 2.2 percentage points (95% CI 1.0–3.5%) from a baseline use rate of 0.3%, an increase in massage of 0.8 percentage points (95% CI 0.2–1.5%) from a baseline use rate of 1.6%, and an increase in chiropractic services by 0.7 percentage points (95% CI 0.2–1.2%), with a large increase in the post-policy slope (0.8 percentage points per quarter), compared to a baseline use rate of 0.3%. Physical and occupational therapy increased substantially (1.9 percentage points; 95% CI 1.1–2.7%, relative to a baseline rate of 6.0%) with the policy but demonstrated slight decreases in the post-policy trend, relative to the pre-period trend. The policy was not associated with significant changes in osteopathic therapy, a finding that was consistent across CCOs (Suppl. E).
Table 2.
Interrupted Time Series Assessing Changes in CAM Use After Policy Implementation
| Any CAM service | Acupuncture | Osteopathic | Chiropractic | PT/OT | Massage | |
|---|---|---|---|---|---|---|
| Time | 1.0 (0.8, 1.3) | 0.2 (0.1, 0.4) | 0.1 (0.0, 0.1) | 0.1 (0.1, 0.2) | 0.7 (0.6, 0.8) | 0.6 (0.5, 0.7) |
| Level | 4.2 (2.3, 6.1) | 2.2 (1.0, 3.5) | 0.1 (− 0.2, 0.3) | 0.7 (0.2, 1.2) | 1.9 (1.1, 2.7) | 0.8 (0.2, 1.5) |
| Slope | 0.0 (− 0.3, 0.4) | 0.0 (− 0.2, 0.2) | 0.0 (− 0.1, 0.0) | 0.8 (0.7, 0.9) | − 0.3 (− 0.5, − 0.2) | 0.1 (− 0.1, 0.2) |
*Time captures the linear trend; Level captures the change in the level of the outcome following implementation of the policy;
Slope captures the change in slope of the linear trend following implementation of the policy
Urban vs Rural vs Mixed Areas
There was heterogeneity based on type of region (urban vs rural). Increase in acupuncture utilization, for example, was most marked in predominantly urban areas (Suppl. B); other services, like PT/OT (Suppl. D) and massage (Suppl. F), increased more evenly across predominantly urban and rural areas.
Coordinated Care Organizations
Differences in adoption of CAM therapies also appeared to vary by CCO (Suppl A–F). For example, CCO M demonstrated sharp increases in use of chiropractic, PT/OT, and massage services, whereas CCO J had only minor increases across all services; both CCOs serve a predominantly rural region.
Number of Services
When looking at the number of CAM services used among patients with back pain who used these services at least once, we again found an overall increase over time, but the increase did not appear to be associated with the policy and no rate of increase after the policy (Fig. 2).
Patient Populations
Compared to back pain patients who did not use any CAM services in 2017/2018, patients who did use CAM services in 2017/2018 were more likely to be women (66.0% vs 59.7%) and live in an urban area (63.0% vs 57.8%) (Table 3), and less likely to be in the youngest age (19–26 years old) group (12.6% vs 15.7%). In regression models (Table 4), Black, American Indian/Alaska Native, and Hispanic enrollees were less likely to access any CAM service than White enrollees (− 8.4, − 3.4, and − 2.2 percentage points, respectively). For Black enrollees, this finding was particularly consistent: this group was less likely than White enrollees to access every individual type of CAM service.
Table 3.
Characteristics of Back Pain Patients Who Did and Did Not Use CAM Services During 2017/2018
| CAM (N = 49,231) | No CAM (N = 102,842) | |
|---|---|---|
| Age group—N (%) | ||
| 19–26 | 6223 (12.6) | 16,164 (15.7) |
| 27–34 | 10,929 (22.2) | 21,622 (21.0) |
| 35–49 | 16,999 (34.5) | 33,526 (32.6) |
| 50–64 | 15,080 (30.6) | 31,530 (30.7) |
| Gender (female)—N (%) | 32,505 (66.0) | 61,421 (59.7) |
| Race/ethnicity—N (%) | ||
| White | 35,861 (72.8) | 73,565 (71.5) |
| Hispanic | 2961 (6.0) | 7707 (7.5) |
| Black | 1521 (3.1) | 4421 (4.3) |
| Asian/HI/PI | 1182 (2.4) | 2358 (2.3) |
| AIAN | 708 (1.4) | 1793 (1.7) |
| Other/unknown | 6998 (14.2) | 12,998 (12.6) |
| Primary spoken language—N (%) | ||
| English | 46,650 (94.8) | 96,824 (94.1) |
| Spanish | 963 (2.0) | 2842 (2.8) |
| Other | 1618 (3.3) | 3176 (3.1) |
| Place of residence—N (%) | ||
| Urban | 31,036 (63.0) | 59,445 (57.8) |
| Rural | 18,195 (37.0) | 43,397 (42.2) |
| History of health conditions—N (%) | ||
| Psychiatric | 20,401 (41.4) | 36,440 (35.4) |
| Skeletal and connective | 19,132 (38.9) | 28,979 (28.2) |
| Cardiovascular | 13,987 (28.4) | 30,775 (29.9) |
| Gastrointestinal | 10,224 (20.8) | 20,633 (20.1) |
| Pulmonary | 7125 (14.5) | 17,070 (16.6) |
| Nervous system | 6121 (12.4) | 11,202 (10.9) |
| Diabetes | 5507 (11.2) | 11,451 (11.1) |
| Renal | 3964 (8.1) | 7027 (6.8) |
| Metabolic | 3571 (7.3) | 7644 (7.4) |
| Genital | 3492 (7.1) | 6160 (6.0) |
| Pregnancy | 3329 (6.8) | 6685 (6.5) |
| Other infectious disease | 2640 (5.4) | 7153 (7.0) |
| Skin | 2246 (4.6) | 5473 (5.3) |
| Eye | 1646 (3.3) | 2824 (2.7) |
| Hematological | 966 (2.0) | 2303 (2.2) |
| Cerebrovascular | 213 (0.4) | 551 (0.5) |
| HIV/AIDs | 216 (0.4) | 506 (0.5) |
| Developmental disability | 141 (0.3) | 386 (0.4) |
CAM services include acupuncture, osteopathic, chiropractic, PT/OT, and massage
Table 4.
Association of Patient Characteristics with Use of CAM Services During 2017/2018
| Any CAM service | Acupuncture | Osteopathic | Chiropractic | PT/OT | Massage | |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| 19–26 | ref | ref | ref | ref | ref | ref |
| 27–34 | 4.9 (4.1, 5.7) | 3.4 (3.0, 3.9) | 0.4 (0.1, 0.7) | 0.9 (0.3, 1.5) | 1.0 (0.4, 1.6) | 2.5 (1.9, 3.1) |
| 35–49 | 2.8 (2.0, 3.5) | 3.1 (2.7, 3.5) | 0.2 (0.0, 0.5) | − 0.9 (− 1.4, − 0.3) | 0.2 (− 0.4, 0.8) | 1.6 (1.1, 2.2) |
| 50–64 | 1.2 (0.4, 2.0) | 2.6 (2.2, 3.1) | 0.0 (− 0.2, 0.3) | − 2.3 (− 2.9, − 1.7) | − 0.1 (− 0.7, 0.5) | 0.9 (0.3, 1.4) |
| Female gender | 4.3 (3.8, 4.8) | 2.0 (1.7, 2.3) | 0.8 (0.6, 0.9) | 0.8 (0.4, 1.1) | 1.6 (1.2, 1.9) | 2.0 (1.7, 2.4) |
| Race-ethnicity | ||||||
| White | ref | ref | ref | ref | ref | ref |
| AI/AN | − 3.4 (− 5.1, − 1.7) | − 0.8 (− 1.7, 0.2) | − 0.3 (− 0.8, 0.3) | − 2.0 (− 3.0, − 1.0) | − 1.9 (− 3.1, − 0.6) | − 1.7 (− 2.9, − 0.5) |
| Asian/HI/PI | 1.2 (− 0.5, 2.9) | 2.4 (1.1, 3.6) | − 0.5 (− 1.0, 0.1) | − 2.1 (− 3.1, − 1.1) | 1.5 (0.2, 2.8) | − 0.1 (− 1.3, 1.1) |
| Black | − 8.4 (− 9.5, − 7.3) | − 2.4 (− 3.0, − 1.8) | − 1.6 (− 1.8, − 1.4) | − 4.8 (− 5.4, − 4.2) | − 1.4 (− 2.2, − 0.5) | − 4.3 (− 5.1, − 3.6) |
| Hispanic | − 2.2 (− 3.2, − 1.2) | − 0.9 (− 1.5, − 0.3) | − 0.5 (− 0.8, − 0.2) | − 1.8 (− 2.4, − 1.1) | 0.2 (− 0.5, 1.0) | − 0.5 (− 1.2, 0.3) |
| Other/unknown | 4.4 (3.6, 5.1) | 1.5 (1.0, 2.0) | 0.1 (− 0.2, 0.4) | 1.5 (0.9, 2.0) | 2.3 (1.7, 2.8) | 1.9 (1.4, 2.5) |
| Primary spoken language | ||||||
| English | ref | ref | ref | ref | ref | ref |
| Other | 0.3 (− 1.0, 1.7) | − 0.2 (− 1.0, 0.6) | − 0.3 (− 0.7, 0.1) | − 2.3 (− 3.1, − 1.5) | 2.5 (1.4, 3.6) | 0.8 (− 0.2, 1.8) |
| Spanish | − 5.1 (− 6.6, − 3.6) | − 2.1 (− 2.9, − 1.2) | − 0.7 (− 1.1, − 0.3) | − 4.1 (− 4.9, − 3.3) | − 0.9 (− 2.1, 0.4) | − 1.4 (− 2.6, − 0.3) |
| Calendar year 2018 | 3.1 (2.7, 3.4) | 0.1 (− 0.1, 0.3) | − 0.1 (− 0.2, 0.0) | 3.2 (3.0, 3.4) | 1.4 (1.1, 1.7) | 2.6 (2.3, 2.9) |
| Urban residence | 6.5 (6.0, 6.9) | 4.3 (4.0, 4.5) | 0.6 (0.4, 0.8) | 0.3 (0.0, 0.6) | 2.6 (2.3, 3.0) | 0.6 (0.2, 0.9) |
Model is adjusted for history of health conditions defined by the Chronic Illness & Disability Payment System (CDPS) including cardiovascular, pulmonary, skeletal and connective, nervous system, gastrointestinal, diabetes, metabolic, hematological, skin, eye, genital, renal, psychiatric, substance abuse, developmental disability, pregnancy, cerebrovascular, HIV/AIDs, and other infectious diseases. AI/AN, American Indian/Alaska; Native, HI/PI Hawaiian/Pacific Islander; PT/OT, physiotherapy/occupational therapy
Distribution Across Providers
Examination of the providers of CAM services was limited due to missing data on provider type. Overall, we found that the distribution of service providers was skewed: 25% of CAM providers provided 50% or more of services, and 50% of CAM providers provided nearly all of the acupuncture, chiropractic, and osteopathic services (Appendix Fig. G).
DISCUSSION
Identifying and promoting effective strategies to improve health outcomes among patients with common types of pain are a critical part of the national effort to reduce the harms of opioid use. While federal and state agencies have advocated and implemented strategies directed at limiting opioids,19–21 many approaches do so without also supporting safe and effective alternatives for pain management. Thus, current policies have been criticized for creating an “innovation gap,” failing to create models of care in which clinicians are supported in caring for patients with chronic pain, and for creating a “reimbursement gap,” failing to cover pain treatments that might be maximally effective.22
A policy that expands coverage of CAM therapies—such as the policy under study—has the potential to empower clinicians to access the full arsenal of approaches to pain management as they pursue greater safety for their patients. In Oregon, we observed a quadrupling in the use of CAM services between 2014 and 2018, with rates of uptake for some services appearing to be low and stable in many CCOs in the period prior to the policy, and substantially increasing afterwards. Therefore, the policy seemed to have been successful in motivating clinicians to alter their practice patterns when treating back pain. However, the average number of services used by those who engaged with CAM providers did not increase in association with the policy. This may signal that more patients access CAM with the new policy, but once accessing CAM does not lead to more services per patient. The absence of a perceived increase in the intensity of use among those who access care may reflect an appropriate dosage or may be consistent with additional barriers in obtaining a higher volume of service.
Expanding coverage for CAM therapies within the Medicaid program has the potential to boost equity in access to a fuller range of evidence-based treatments for back pain.23 However, this is no guarantee that various types of inequities will not persist in the effort. As a case in point, we observed that racial and ethnic minority groups and men were less likely to receive these services in the post-policy period.
Racial disparities have been observed in previous studies on CAM use for a variety of clinical indications.12,15 Hypothesized mechanisms include variable awareness and acceptance of such therapies by patients and providers, patients’ cultural norms, expectations and stigmas about the therapies, and biased referral and counseling practices related to the therapies, including those driven by structural racism. Further work is needed to evaluate the factors that may have been most influential in the disparities we observed in this study.
We also observed decreased uptake of CAM services in rural populations, compared to urban populations. It is not surprising that insurance benefits and guidance might not overcome the many factors that prohibit a shift of treatment norms in rural settings. The number of CAM service providers in Oregon increased over the time of the study,24 something that may have facilitated increased use or have been driven by increased demand related to this policy. Nevertheless, local availability of services, necessitating scheduling and travel burdens, likely makes these services still impractical for many patients, particularly those in remote areas.
These access issues likely overlapped with implementation decisions and approaches by CCOs. Individual CCOs had autonomy to select all aspects of the extent and accessibility of increased CAM coverage, including covered services, caps on utilization, pre-authorization requirements, provision of information, education, and other supports for clinical decision making to clinics and individual health care providers, and incentives and tracking to ensure adherence to the new policy. Variability across these factors likely contributed to the overall and service-by-service differences we observed across CCOs.
Despite the increase in CAM utilization that we observed following the Oregon policy, many barriers exist to transitioning these services to be truly standard and first-line among patients with back pain. These include the readiness of CAM therapists to accept relatively low Medicaid reimbursement rates, the challenge of changing referral practices among primary care providers, lack of electronic health record (EHR) supports for new treatment algorithms, administrative burdens for placing referrals and, in some cases, completing pre-authorization processes, and unseen costs to the patient (transportation, scheduling, time out from work). While evidence demonstrates the mild to moderate efficacy of these therapies, the improvement in health outcomes for Oregon Medicaid patients receiving these CAM therapies may not be realized across the population until uptake is more widespread.
Limitations
We were not able to capture the use of some therapies covered under the policy (e.g., yoga) because the related codes in claims data are non-specific and/or not consistently co-coded with a physical back pain diagnosis. There may also be a slight underestimation of CAM use missed through a claims analysis because some CCOs may have offered select CAM services through alternative payment structures to avoid billing and credentialing issues that might make it challenging for the CAM service providers to participate in the care of Medicaid back pain patients. Our study population included patients who had at least 3 months of enrollment over the prior 12 months. Because a substantial percentage of Medicaid patients have discontinuity in coverage over the course of a year—especially lower income patients—we used inclusive criteria for our study population. Lack of use of CAM services within a given quarter may be due to lack of coverage. However, this should be consistent before and after the back pain policy and should not account for our findings.
This study was an examination of CAM use in Oregon and may therefore not be generalizable to other states. In addition, our analysis does not include a control state, which would strengthen support for the observed effects being due to the policy and not to secular trends. While we are not aware of any secular factors (other policies or market forces) that would influence CAM utilization in general during the time period of the study, it is possible that increases in service utilization have occurred independent of policy change. However, given the rate of change that is coincident with requirements for CCOs to newly cover these therapies, it seems likely that the observed phenomenon was related to the policy. Some of the increases occurred the quarter prior to the official policy implementation; this was likely an anticipatory effect, as the policy implementation date was initially planned25 for 6 months prior to the final implementation date.
CONCLUSIONS
Shifting care of back pain to evidence-based CAM therapies is a promising route to treating symptoms more effectively and avoiding treatments, such as opioid therapies, with low efficacy and potential harms. Oregon’s back pain policy appears successful in boosting use of CAM therapies in this patient population, although disparities in use were noted for minority patient populations, men, and those living in rural areas. The impact of policy-related uptake of these therapies on prescription opioid use and other health outcomes for patients with back pain remains to be seen.
Supplementary Information
(DOCX 390 kb)
Funding
This research was funded by NIH award 1R01DA044284-01A1 (NIDA) and 1R01MD011212 (NIMHD).
Compliance with Ethical Standards
Conflict of Interest
Dr. Choo is a co-founder of Equity Quotient, a company that provides metrics of healthcare company culture, especially with respect to gender and racial dynamics. Dr. Livingston is Associate Medical Director of the Health Evidence Review Commission and was involved in the development of the policy coverage change. She currently serves as Medical Director for one of the Oregon CCOs.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976) 2006;31(23):2724–2727. doi: 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 2.Shmagel A, Foley R, Ibrahim H. Epidemiology of Chronic Low Back Pain in US Adults: Data From the 2009-2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 2016;68(11):1688–1694. doi: 10.1002/acr.22890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350(1):g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chou R, Turner JA, Devine EB, et al. The Effectiveness and Risks of Long-Term Opioid Therapy for Chronic Pain: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162(4):276. doi: 10.7326/M14-2559. [DOI] [PubMed] [Google Scholar]
- 5.Chou R. Pharmacological Management of Low Back Pain. Drugs. 2010;70(4):387–402. doi: 10.2165/11318690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Deyo RA, Smith DHM, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of services. J Am Board Fam Med. 2011;24(6):717–727. doi: 10.3122/jabfm.2011.06.100232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim H, Hartung DM, Jacob RL, McCarty D, McConnell KJ. The Concentration of Opioid Prescriptions by Providers and Among Patients in the Oregon Medicaid Program. Psychiatr Serv. 2016;67(4):397–404. doi: 10.1176/appi.ps.201500116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 9.Chou R, Deyo R, Friedly J, et al.Noninvasive Treatments for Low Back Pain: Executive Summary. Comparative Effectiveness Review No. 169. Rockville, MD; 2016.
- 10.Moritz S, Liu M, Rickhi B, Xu T, Paccagnan P, Quan H. Reduced health resource use after acupuncture for low-back pain. J Altern Complement Med. 2011;17(11):1015–1019. doi: 10.1089/acm.2010.0619. [DOI] [PubMed] [Google Scholar]
- 11.Dorr H, Townley C. Chronic Pain Management Therapies in Medicaid: Policy Considerations for Non- Pharmacological Alternatives to Opioids. Natl Acad State Heal Policy. 2016.
- 12.Chao MT, Wade C, Kronenberg F, Kalmuss D, Cushman LF. Women’s Reasons for Complementary and Alternative Medicine Use: Racial/Ethnic Differences. J Altern Complement Med. 2006;12(8):719–720. doi: 10.1089/acm.2006.12.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heyward J, Jones CM, Compton WM, et al. Coverage of Nonpharmacologic Treatments for Low Back Pain Among US Public and Private Insurers. JAMA Netw Open. 2018;1(6):e183044. doi: 10.1001/jamanetworkopen.2018.3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oregon Health Plan: Back Policy Changes Fact Sheet. 2016.
- 15.Rhee TG, Evans RL, McAlpine D, Johnson PJ. Racial/Ethnic Differences in the Use of Complementary and Alternative Medicine in US Adults With Moderate Mental Distress. J Prim Care Commun Health. 2017;8(2):43–54. doi: 10.1177/2150131916671229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McConnell KJ. Oregon’s Medicaid Coordinated Care Organizations. JAMA. 2016;315(9):869. doi: 10.1001/jama.2016.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oregon Office of Rural Health Geographic Definitions.
- 18.Kronick R, Gilmer T, Dreyfus T, Lee L. Improving health-based payment for Medicaid beneficiaries: CDPS. Heal Care Financ Rev. 2000;21(3):29–64. [PMC free article] [PubMed] [Google Scholar]
- 19.Wachino V. CMCS Informational Bulletin: Best Practices for Addressing Prescription Opioid Overdoses, Misuse Addict 2016:15.
- 20.Keast SL, Pham T, Teel A, Nesser NJ. Incremental Effect of the Addition of Prescriber Restrictions on a State Medicaid’s Pharmacy-Only Patient Review and Restriction Program. J Manag Care Spec Pharm. 2017;23(8):875–883. doi: 10.18553/jmcp.2017.23.8.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dowell D, Haegerich T, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep. 2016;65(RR-1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 22.Olsen Y, The CDC Guideline on Opioid Prescribing. JAMA. 2016;315(15):1577. doi: 10.1001/jama.2016.1910. [DOI] [PubMed] [Google Scholar]
- 23.KJ M, CJ C, THA M, RM G, H K. Oregon’s Emphasis On Equity Shows Signs Of Early Success For Black And American Indian Medicaid Enrollees. Health Aff (Millwood). 2018;37(3). [DOI] [PMC free article] [PubMed]
- 24.U.S. Bureau of Labor Statistics. Occupational Employment Statistics. 2019.
- 25.Oregon Health Authority. Health Evidence Review Commission. Back Policy Changes Fact Sheet. 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 390 kb)