INTRODUCTION
The American Heart Association (AHA) and American College of Cardiology (ACC) published telemetry guidelines outlining indications for and duration of use.1 Misuse of telemetry monitoring is associated with increased costs, staff burdens, and misdiagnosis leading to unnecessary cardiovascular interventions.2 Resident physicians have low self-reported use of the AHA/ACC guidelines for telemetry.3 Curricula are needed to address this gap.
Our group developed an interactive, multimodal curriculum for internal medicine residents.4 The curriculum was modified to provide dedicated and protected teaching time for interns given inadequate results for interns in the prior iteration. Our study aims were to assess interns’ baseline knowledge and skills around inpatient telemetry and determine the effectiveness of our curriculum in improving these factors.
METHODS
We conducted a single-center cohort study at a large urban academic medical center in Chicago, IL, from July 2018 to June 2019. All categorical PGY-1 internal medicine residents were included. Participants completed a computer-based pre-test and were then provided with a previously described telemetry curriculum4 during an academic half-day free of clinical duties. Briefly, the curriculum included a 20-min video reviewing the AHA/ACC indications for telemetry and provided a step-by-step review of proper interrogation and interpretation of telemetry monitors at our institution. Subsequently, learners engaged in an interactive case-based presentation and hands-on deliberate practice on real-time inpatient telemetry monitors to solidify knowledge. Interns then completed a post-test. Confidence with skills related to telemetry monitoring on a scale from 0 (cannot do at all) to 100 (highly certain can do) was assessed.
Paired samples t test was used to compare pre- and post-test scores for participants. Chi-squared analysis was used to compare achievement of mastery level (86% correct on the test) pre- and post-curricular intervention. Data analysis was performed using Stata v.12 (StataCorp, College Station, TX) and R version 3.6.0. This study was approved by the Institutional Review Board of Northwestern University Feinberg School of Medicine.
RESULTS
Seventy-one percent of categorical internal medicine interns (n = 27) completed the pre- and post-tests and were included in the analysis. Mean score on the pre-test was 73.1% and increased to 83.2% in the post-test (p < 0.001). Figure 1 shows the box plot of test scores comparing the percent correct pre-curriculum to post-curriculum. Mastery level performance (score of 86% or higher) improved from 15% pre-curriculum to 44% post-curriculum after one teaching session (p = 0.015). Table 1 shows confidence scores for each of the ten questions pertaining to telemetry knowledge and skills. Notably, confidence significantly increased from pre- to post-curriculum.
Fig. 1.
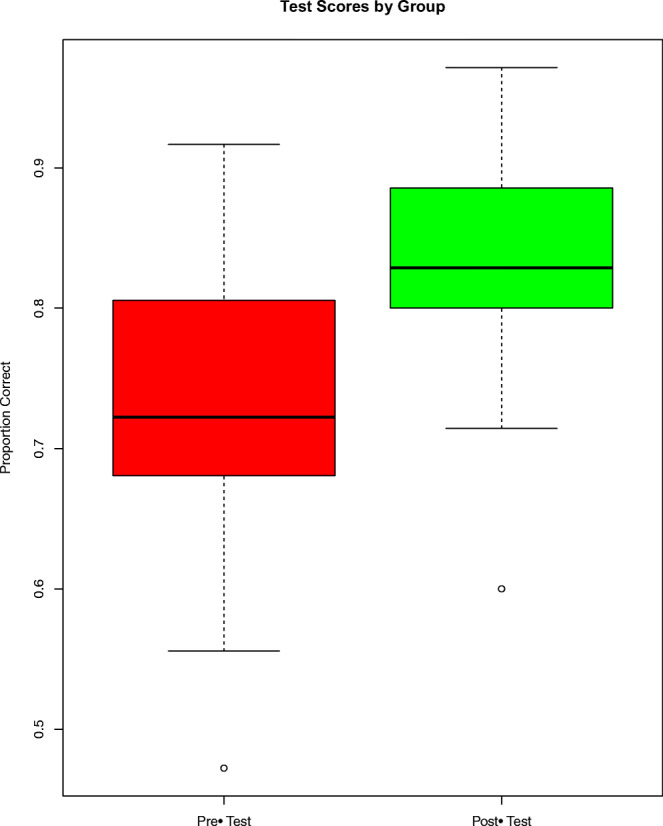
Test Scores Pre- and Post-Curriculum.
Table 1.
Intern Confidence Scores Pre- and Post-Curriculum (n = 27)
| Statement | Pre-curriculum | Post-curriculum | p value |
|---|---|---|---|
| Naming the AHA/ACC guideline indications for proper initiation and discontinuation of inpatient telemetry monitoring. | 39 ± 6 | 71 ± 6 | < 0.001 |
| Categorizing current AHA/ACC guidelines for proper initiation of inpatient telemetry monitoring by strength of indication (Class I/II/III). | 24 ± 8 | 70 ± 7 | < 0.001 |
|
Utilizing the various functions on the telemetry monitor, including FD page, FD strip, calipers, events tab, and graphical trends. |
67 ± 7 | 86 ± 5 | < 0.001 |
| Manipulating the telemetry display to identify both the onset and termination of an arrhythmia. | 62 ± 10 | 89 ± 4 | < 0.001 |
| Identifying which arrhythmia is most likely based on the graphical trend display. | 57 ± 7 | 83 ± 5 | < 0.001 |
| Distinguishing true ventricular tachycardia from telemetry artifact. | 61 ± 8 | 86 ± 4 | < 0.001 |
| Using the functions on the telemetry monitor to determine what type of AV block is present. | 42 ± 11 | 80 ± 5 | < 0.001 |
| Distinguishing atrial fibrillation from all other arrhythmias based on the graphical trend display. | 53 ± 10 | 88 ± 4 | < 0.001 |
| Systematically reviewing a patient’s telemetry to determine if any clinically significant arrhythmia has taken place. | 65 ± 9 | 87 ± 4 | < 0.001 |
| Explaining the etiology of any arrhythmia identified on a patient’s telemetry. | 42 ± 8 | 75 ± 6 | < 0.001 |
ACC, American College of Cardiology; AHA, American Heart Association; AV, atrioventricular
DISCUSSION
Our multimodal curriculum focusing on teaching indications and interpretation of inpatient telemetry monitoring provided to internal medicine interns resulted in an improvement in overall test performance as well as a threefold increase in mastery level achievement. Confidence in identifying the guidelines and completing telemetry interpretation tasks improved significantly.
Prior work on improving proper telemetry utilization has focused on leveraging the electronic medical record to reduce improper telemetry prescription.5 By adjusting order sets to require the provider to identify the indication for ordering telemetry, investigators in one study saw an approximate 50% reduction in both mean telemetry orders and mean telemetry duration.5 However, such approaches while impactful on a systems level do not impact knowledge of trainees or ensure that telemetry is being properly interpreted even when it is being used appropriately. Other approaches to educate medical residents on proper telemetry use have embedded this skill in a broad curriculum containing multiple other educational objectives.6 Our approach differs in that it is solely focused on improving knowledge and skills around telemetry and utilizes deliberate practice methodology to achieve this objective.
We observed an increase in knowledge from 73 to 83%. Iterations of booster training with real-world experience ordering and interpreting telemetry monitoring are likely to raise the proportion of trainees achieving mastery.
This study’s generalizability to other institutions is limited by use of a single institution. In addition, only 71% of eligible interns completed both pre- and post-tests. We did not collect data on the longitudinal effect of this curriculum. In the future, we plan to investigate retention of skills, behavior change, and ideally determine downstream improvement in patient care.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations
None
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sandau Kristin E. Funk Marjorie, Auerbach Andrew, et al. Update to Practice Standards for Electrocardiographic Monitoring in Hospital Settings: A Scientific Statement From the American Heart Association. Circulation. 2017;136(19):e273–e344. doi: 10.1161/CIR.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 2.Knight BP, Pelosi F, Michaud GF, Strickberger SA, Morady F. Clinical consequences of electrocardiographic artifact mimicking ventricular tachycardia. N Engl J Med. 1999;341(17):1270–1274. doi: 10.1056/NEJM199910213411704. [DOI] [PubMed] [Google Scholar]
- 3.Brug AM, Hudson KM, Moore R, Chakraborti C. Choosing Telemetry Wisely: a Survey of Awareness and Physician Decision-Making Regarding AHA Telemetry Practice Standards. J Gen Intern Med. 2019;34(4):496–497. doi: 10.1007/s11606-018-4769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chuzi S, Cantey EP, Unger E, et al. Interactive Multimodal Curriculum on Use and Interpretation of Inpatient Telemetry. MedEdPORTAL. 14. [DOI] [PMC free article] [PubMed]
- 5.Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering Overuse of Cardiac Telemetry in Non–Intensive Care Unit Settings by Hardwiring the Use of American Heart Association Guidelines. JAMA Intern Med. 2014;174(11):1852–1854. doi: 10.1001/jamainternmed.2014.4491. [DOI] [PubMed] [Google Scholar]
- 6.Hom J, Kumar A, Evans KH, et al. A high value care curriculum for interns: a description of curricular design, implementation and housestaff feedback. Postgrad Med J. 2017;93(1106):725–729. doi: 10.1136/postgradmedj-2016-134617. [DOI] [PubMed] [Google Scholar]


