Abstract
BACKGROUND:
Stroke is a time-sensitive neurological disease and a life-threatening medical condition. Providing timely management for stroke patients is a crucial issue in healthcare settings. The primary objective of this study is to evaluate the effectiveness of an evidence-based educational program on healthcare providers’ (HCPs) overall knowledge of stroke.
METHODS:
A randomized block design with post-test only was used. A total of 189 HCPs (physicians, registered nurses, and paramedics) involved with treating stroke patients in the emergency were recruited. Participants were randomly assigned to either the intervention or waiting list control group. A one-session, stroke educational program was offered to the HCPs followed by a post-test designed to assess knowledge about stroke.
RESULTS:
A significant main effect on the profession type was found, with physicians having higher mean scores of stroke knowledge compared with nurses and paramedics (F [2, 183]=48.55, P<0.001). The implemented educational program had a positive effect on increasing the level of stroke knowledge among HCPs (F [1, 183]=43.31, P<0.001). The utilization of any evidence-based assessment tools for patients with suspected stroke was denied by 36% of the total sample.
CONCLUSIONS:
The implemented intervention can increase HCP’s knowledge regarding stroke. Stroke education should be considered as one of the essential requirements for professional development for all HCPs in the emergency.
Keywords: Stroke, Misdiagnosis, Healthcare providers’, knowledge, Stroke knowledge
INTRODUCTION
Stroke is a time-sensitive neurological disease and a life-threatening medical condition. According to the American Heart Association statistics, approximately 11.8% of worldwide deaths are due to stroke, which is considered as a global cerebrovascular problem.[1] Stroke is accompanied by intense negative impacts on survivors’ physical, psychological, and social functioning. Stroke is the second leading cause of death after heart disease and is a leading cause of permanent disability and handicaps in adults.[1] The World Health Organization (WHO) indicates that approximately 80% of stroke deaths occur in low- and middle-income countries (LMICs).[2] Regardless of major improvements in its management over the last few decades, stroke is still a deadly disease that is on the rise because of an aging population worldwide and the epidemiological transition in LMICs, and one of these countries is Jordan.[3,4] Approximately 12% of the total deaths in Jordan result from stroke, and it is the third leading cause of death in the country.[5] The burden of stroke is expected to continuously increase in the future in Jordan because of the expected demographic changes.
It is recommended that stroke diagnosis must be initiated within 25 minutes.[6,7] The reason is that every minute of delay in treating stroke may result in an average of 1.8 days of healthy life lost.[8] Delays in timely recognition and management of stroke could be attributed to at least two factors. Firstly, the process of conducting a proper assessment is lengthy and requires time. Secondly, it is common to misdiagnose stroke and confuse stroke with other common neurological conditions, such as seizures and migraine, which may lead to an unnecessary delay in providing proper treatment.[6] As a result, stroke becomes one of the most commonly misdiagnosed diseases.[9] Therefore, early and timely intervention by healthcare providers (HCPs) is vital to significantly reduce the severity and impact of stroke and reduce long-term disabilities.
The timely treatment of stroke enhances the opportunity of achieving excellent outcomes.[10] However, one of the most important factors that affect initiating appropriate treatment action by HCPs is to make an accurate diagnosis and a timely treatment plan.[11] Paramedics and emergency department (ED) personnel must be trained to accurately identify patients who are exhibiting symptoms of stroke using quick and standardized tests.[12] Triage at the ED after hospital arrival is also important. Surprisingly, some published reports suggest that paramedics may fail to recognize over half of stroke cases because pre-hospital scales are either less effective in clinical practice or are not utilized adequately by pre-hospital providers.[13,14] Surely, HCPs must utilize evidence-based knowledge and resources when providing care for patients suffering stroke to ensure optimistic clinical outcomes.
There is evidence that HCPs’ education regarding stroke is still fragmented.[15] Moreover, it is reported that there are many hospitals that do not force HCPs to implement and follow evidence-based protocols regarding stroke management.[16] Continuing education (CE) and professional development could facilitate preparing competent and well-trained HCPs capable of recognizing and providing high-quality care to stroke patients. Therefore, the primary objective of this study is to evaluate the effectiveness of an evidence-based educational program on HCPs’ knowledge of stroke, risk factors, warning signs, and proper course of diagnosis. The secondary objectives are to compare physicians’, nurses’ and paramedics’ abilities to identify stroke signs and symptoms, and to assess HCPs’ knowledge and utilization of evidence-based resources regarding stroke care.
METHODS
Design
The study was conducted using a randomized block design with post-test only. In this study, the researchers decided to divide the sample into three blocks (i.e., groups): physicians, nurses, and paramedics. This randomized block design removed the type of profession as a potential source of variability and as a potential confounding variable. Within each of the three blocks, the researchers assigned the participants into either the intervention or waiting list control group.
Setting
The study was done at the EDs of three major hospitals. In addition, paramedics from the Jordanian Civil Defense were involved in the study.
Sampling and participants
The purposive sampling method was used to recruit the study participants after explaining and discussing the study’s purpose, procedures, and potential benefits and risks with potential participants. HCPs (physicians, nurses, and paramedics) who met the following inclusion criteria were invited to participate in this study: (1) age ≥18 years; (2) willing to attend the designed educational intervention program; and (3) ≥ six months of work experience in either the ED or the Jordanian Civil Defense paramedic system.
The required sample size was calculated using G*Power analysis with an estimated overall sample size of 192 participants. Sixty-four participants for each group (physicians, nurses, and paramedics) were recruited in this study. Then, 32 participants in each group were randomly assigned to either the intervention or waiting list control group. Eligible participants in this study were randomly assigned in a 1:1 ratio to the intervention or the control group according to a random table schedule. Participants in the intervention group were asked to attend a two-hour stroke education program for each session. Participants in the waiting list control group were offered the opportunity to attend the stroke education program one-month post-data collection.
Intervention
The stroke education program was designed by the researchers and reviewed by HCPs who were experienced in neurological health problems and health professional education. It involved a PowerPoint presentation given by the researcher. A total of 10 educational sessions were delivered to the intervention group participants. Each educational session lasted for approximately two hours. During each presentation, the focus was on how to recognize stroke and its risk factors, as well as the warning signs and the appropriate medical intervention required to treat stroke in the emergency.
The following topics were covered in the educational sessions: (1) risk factors, types, mechanisms, clinical manifestations, and complications of stroke; (2) primary and secondary prevention of stroke; (3) screening and initial assessments of stroke patients; (4) appropriate medical intervention required to treat stroke in the emergency; and (5) helpful evidence-based practice guidelines and tools used to detect and treat stroke patients.
Procedure
Researchers approached eligible participants and explained the study and its procedure. Packets containing a cover letter explaining the study and informed consent were distributed to the participants. After the presentation of the educational sessions, participants in both groups were asked to individually complete a demographics questionnaire and a test on the knowledge of risk factors, signs and symptoms, diagnosis, and management of stroke. The test was reviewed by HCPs who experienced in neurology and health education. The test items were developed from evidence-based guidelines, professional recommendations, and an extensive review of the stroke literature. Eighteen items were on HCP’s knowledge of stroke, and the remaining two questions focused on the utilization of evidence-based resources. Possible scores on the test ranged from 0 to 18, with higher scores indicating a better level of stroke knowledge. Content validity was established by asking three experts to review the test and provide feedback regarding each item of the questionnaire. This panel of experts included professionals with expertise in emergency and neuroscience care as well as health professional education.
A two-way analysis of variance (ANOVA) was used to compare the mean scores of knowledge among three groups of the study using SPSS software (Version 25). Frequencies and descriptive statistics were also used.
RESULTS
Participants’ characteristics
A total of 189 HCPs (97 in the intervention group and 92 in the control group) completed the questionnaires, with 39% (n=74) being women and 61% (n=115) being men. Out of the 189 HCPs, 32% (n=61) were physicians, 34% (n=64) were nurses, and 34% (n=64) were paramedics.
ANOVA analysis
An independent and two-way ANOVA analysis was performed. Post-hoc and follow-up t-tests were also performed to detect the exact source of mean differences, when present. Using the two-way ANOVA, the average of the dependent variable (DV) and HCP’s knowledge were first compared among participants based on their professions and groups (intervention or control). The results showed a statistically significant effect on the profession types (F [2, 183]=48.55, P<0.001); a statistically significant effect on the groups (intervention or control) (F [1, 183]=43.31, P<0.001); and a non-significant interaction effect (F [2, 183]=0.07, P>0.050).
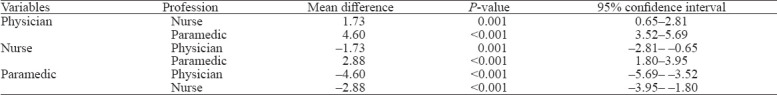
Post-hoc analysis using a Tukey test was performed to compare the mean scores of the DV for the participants based on the type of profession. The results of Tukey post-hoc revealed statistically significant mean differences among the study participants based on the type of profession; physicians had a significantly higher mean score on the stroke knowledge test compared with nurses and paramedics. The results are presented in Table 1.
Table 1.
Post-hoc analysis using a Tukey test
Because the main effects of the independent variables (IVs) were significant, follow-up analyses were also conducted to determine the exact source of difference for the two IVs: type of profession and group. To determine the source of mean differences in the HCP’s knowledge with respect to the profession according to the group, the researcher used the split method to classify the data based on the group, intervention or control. Then, one-way ANOVA analysis was performed twice after adjusting the significance value P<0.05÷2=0.025. The adjusted significance level was calculated to avoid the inflation of a type I error. The results revealed statistically significant main differences using the one-way ANOVA test: F (2, 89)=23.74, P<0.001 for the control group; and F (2, 94)=24.87, P<0.001 for the intervention group.
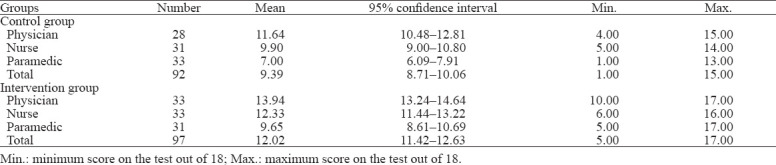
Furthermore, three independent t-tests were performed to examine the source of difference among HCPs with respect to the group, intervention or control group (Table 2). The significance level was adjusted again and was calculated as P<0.05÷3=0.016. The results of the independent t-tests showed that the intervention group of physicians had a higher score of stroke knowledge compared with the control group of physicians (t= –3.58, P=0.001). Nurses in the intervention group also had a statistically significant higher mean score compared with the control group of nurses (t= –3.91, P<0.001). Similarly, the intervention group of paramedics had higher mean scores of stroke knowledge compared with the control group (t=3.92, P<0.001), which indicated that there were significant positive improvements in knowledge of stroke in the intervention group compared with the control group.
Table 2.
Overall knowledge score differences for participants classified by groups
Regarding the utilization of evidence-based resources by HCPs, the researchers found that 36% of the total participants did not use any scale types in the initial assessment of a patient suspected with stroke. The most frequently used stroke assessment was the Face, Arm, Speech, and Time (FAST) scale.
DISCUSSION
The findings of the current study, consistent with the results of previous research, highlight the multifaceted nature of stroke HCPs’ experiences.[4] Understanding and evaluating the educational needs of HCPs regarding stroke is essential to establish beneficial interdisciplinary training. In addition, evaluating the standards and elements of stroke care, as carried out by HCPs in the emergency, facilitates achieving better health outcomes for stroke patients. A review of the literature on health service delivery demonstrates that active educational intervention is more likely to induce changes in practice.[17]
The overall program was successful with an improvement of the test scores between intervention and control groups. In addition, the study revealed statistically significant mean differences among the study participants based on the type of profession. Similarly, in Catangui’s study,[18] a training program developed by a team of professionals with expertise in stroke care aimed to teach each professional involved in many aspects of stroke care. The authors found that the training program was successful in increasing staff knowledge of the care for stroke patients, improving collaboration, and enhancing working practices. These findings were similar to and supported the results of the current study.
Much acquaintance between knowledge, practice, and performance measurement was reported in the literature.[19,20] HCPs involved with stroke management need to be attentive through regular updating of their own knowledge, as ongoing research in the field illuminates greater insights into improved management skills pertinent to stroke care. Despite the reported effectiveness of stroke education in improving health outcomes, Mason-Whitehead and colleagues[21] found that there was still insufficient stroke awareness and knowledge. Stroke education is not often provided and is not a prerequisite for emergency medical services (EMS) certification or CE in Jordan. Therefore, educating and training emergency dispatchers is warranted, as it could significantly improve the chances of recognizing stroke cases.[22]
It is reported in the literature that education strengthens nurses’ knowledge of their role in stroke and helps to define the roles of other HCPs.[23] Additionally, implementation of education directed at nurses was found to have a strong potential to increase acute intervention of in-hospital strokes.[24] George et al[24] stated that most of the acute stroke calls came from nurses. However, nurses were found in the current study to have lower levels of stroke knowledge compared with physicians. Thus, nurses, especially those who work at the ED, are required to stay updated regarding the most valid approaches of detecting and assessing stroke patients in a timely manner.
In the current study, physicians had the highest levels of stroke knowledge. However, the results showed that physicians should also update their stroke knowledge. Specifically, physicians’ knowledge regarding the utilization of evidence-based resources should be integrated into CE and certification requirements.
Limitations
Despite its strength and suitability for the current study, randomized block design has a number of threats to internal validity. Based on the results of the descriptive statistics, the intervention and control groups were, to an extent, comparable in terms of the major sociodemographic variables like age, experience, and education. A major threat to internal validity, however, was the mortality threat. The original plan of this study was to conduct follow-up tests at two weeks and then three months after implementing the educational sessions. The purpose of such planned follow-up tests was to examine the effectiveness of the implemented program in improving the retention of knowledge among HCPs, but none of these follow-up tests were conducted despite the researchers’ endeavors to do so. The participants declined to take the follow-up tests for various reasons, including: (1) job requirements and the busy schedule they had; (2) lack of interest with the study; (3) taking vacations; and (4) being busy preparing for the medical board exam. Regarding the external validity and generalizability of the results, the researcher was able to recruit a minimal number of participants in each group. However, the sample was obtained using a purposive sampling method. In addition, the study was conducted using a post-test only design. Using a pre- and post-test design in the future is warranted.
CONCLUSIONS
Stroke is a worldwide main concern that requires having a larger number of trained HCPs and collaboration among them. Advancing HCPs’ knowledge and skills about stroke management is the starting point to help reduce the overwhelming impact of stroke on patients, their family members, and the healthcare system. The results of this study show that there is a significant improvement in stroke knowledge among HCPs in the intervention group. HCPs should be provided with evidence-based resources on acute stroke care and opportunities to participate in CE. Interdisciplinary collaboration and interprofessional education could help in maximizing the identification of stroke cases and minimizing its impact. Finally, enhanced education and the development of training programs could make a difference in the future regarding stroke care.
ACKNOWLEDGEMENTS
The authors are gratefully thankful to Jordan University of Science and Technology staff for facilitating the process of obtaining the Institutional Review Board approvals from the different settings and their support throughout the process of conducting this research study.
Footnotes
Funding: This project was funded by the Directorate General of Civil Defense, Jordan.
Ethical approval: Before starting the study, approvals were obtained from the Institutional Review Board (IRB) at Jordan University of Science and Technology (IRB protocol #1-2018) followed by the approval of IRB committees of the University of Jordan Hospital, the directory of Jordanian Royal Medical services, the Ministry of Health, and Civil Defense.
Conflicts of interest: The authors declare that they have no competing interests.
Contributors: JAR proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.American Heart Association (AHA) Heart disease and stroke statistics 2017 at a glance. Available at https: //healthmetrics.heart.org/wp-content/uploads/2017/06/Heart-Disease-and-Stroke-Statistics-2017-ucm_491265.pdf .
- 2.World Health Organization. Global status report on noncommunicable diseases 2014:attaining the nine global noncommunicable diseases targets;a shared responsibility. Available at http: //apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf;jsessionid=C4977E9D2FEB5CA94CBB4A6A184747FA?sequence=1 .
- 3.Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010:findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245–55. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malik P, Anwar A, Patel R, Patel U. Expansion of the dimensions in the current management of acute ischemic stroke. J Neurol. 2020 May 20; doi: 10.1007/s00415-020-09873-6. doi:10.1007/s00415-020-09873-6. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Global health –Jordan. Available at https: //www.cdc.gov/globalhealth/countries/jordan/
- 6.Yew KS, Cheng E. Acute stroke diagnosis. Am Fam Physician. 2009;80(1):33–40. [PMC free article] [PubMed] [Google Scholar]
- 7.American Heart Association. Brain health. Available at http: //brainhealth.strokeassociation.org/
- 8.Lees KR, Walters MR. Acute stroke and diabetes. Cerebrovasc Dis. 2005;20(Suppl. 1):9–14. doi: 10.1159/000088232. [DOI] [PubMed] [Google Scholar]
- 9.Tarnutzer AA, Lee SH, Robinson KA, Wang ZY, Edlow JA, Newman-Toker DE. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: a meta-analysis. Neurology. 2017;88(15):1468–77. doi: 10.1212/WNL.0000000000003814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pourmand A, Pyle M, Yamane D, Sumon K, Frasure SE. The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients. World J Emerg Med. 2019;10(4):232–8. doi: 10.5847/wjem.j.1920-8642.2019.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caminiti C, Schulz P, Marcomini B, Iezzi E, Riva S, Scoditti U, et al. Development of an education campaign to reduce delays in pre-hospital response to stroke. BMC Emerg Med. 2017;17(1):20. doi: 10.1186/s12873-017-0130-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Brien W, Crimmins D, Donaldson W, Risti R, Clarke TA, Whyte S, et al. FASTER (Face, Arm, Speech, Time, Emergency Response):experience of Central Coast Stroke Services implementation of a pre-hospital notification system for expedient management of acute stroke. J Clin Neurosci. 2012;19(2):241–5. doi: 10.1016/j.jocn.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Adams HP, Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke:a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups:The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478–e534. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 14.Song S, Saver J. Growth of regional acute stroke systems of care in the United States in the first decade of the 21st century. Stroke. 2012;43(7):1975–8. doi: 10.1161/STROKEAHA.112.657809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bekelis K, Roberts DW, Zhou WP, Skinner JS. Fragmentation of care and the use of head computed tomography in patients with ischemic stroke. Circ Cardiovasc Qual Outcomes. 2014;7(3):430–6. doi: 10.1161/CIRCOUTCOMES.113.000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khatib R, Jawaada AM, Arevalo YA, Hamed HK, Mohammed SH, Huffman MD. Implementing evidence-based practices for acute stroke care in low- and middle-income countries. Curr Atheroscler Rep. 2017;19(12):61. doi: 10.1007/s11883-017-0694-6. [DOI] [PubMed] [Google Scholar]
- 17.Smith LN, Craig LE, Weir CJ, McAlpine CH. Stroke education for healthcare professionals:making it fit for purpose. Nurse Educ Today. 2008;28(3):337–47. doi: 10.1016/j.nedt.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Catangui EJ, Slark JL. Development and evaluation of an interdisciplinary training programme for stroke. British Journal of Neuroscience Nursing. 2012;8(1):8–11. [Google Scholar]
- 19.Kilbride C, Perry L, Flatley M, Turner E, Meyer J. Developing theory and practice:Creation of a community of practice through action research produced excellence in stroke care. J Interprof Care. 2011;25(2):91–7. doi: 10.3109/13561820.2010.483024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oufkir L, Fredj M, Kassou I. Performance measurement for knowledge management: designing a reference model. Journal of Organizational Knowledge Management. 2017 doi:10.5171/2017.733562. [Google Scholar]
- 21.Mason-Whitehead E, Ridgway V, Barton J. Passed without a stroke:a UK mixed method study exploring student nurses'knowledge of stroke. Nurse Educ Today. 2013;33(9):998, 1002. doi: 10.1016/j.nedt.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Viereck S, Møller TP, Iversen HK, Christensen H, Lippert F. Medical dispatchers recognise substantial amount of acute stroke during emergency calls. Scand J Trauma Resusc Emerg Med. 2016;24:89. doi: 10.1186/s13049-016-0277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindsay MP, Kelloway L, McConnell H. Research to practice:nursing stroke assessment guidelines link to clinical performance indicators. Axone. 2005;26(4):22–7. [PubMed] [Google Scholar]
- 24.George P, Wisco DR, Gebel J, Uchino K, Newey CR. Nurses are as specific and are earlier in calling in-hospital stroke alerts compared to physicians. J Stroke Cerebrovasc Dis. 2017;26(5):917–21. doi: 10.1016/j.jstrokecerebrovasdis.2016.10.003. [DOI] [PubMed] [Google Scholar]


