Abstract
Although in recent years adenotonsillectomy procedures have shown an overall reduction in number, this surgery continues to be the most frequently performed in our speciality, especially in pediatric age. The progressive improvement in both surgical techniques and devices and anaesthesia has made adenotonsillectomy a less risky manoeuvre, but this does not mean that it is free from potential adverse events or even an easy, routine and risk-free procedure, as presented by some para scientific literature and mass media. Here we address issues related to the complications that can arise when performing this surgical procedure, which can be very serious. (www.actabiomedica.it)
Keywords: adenotonsillectomy, children, complications
Introduction
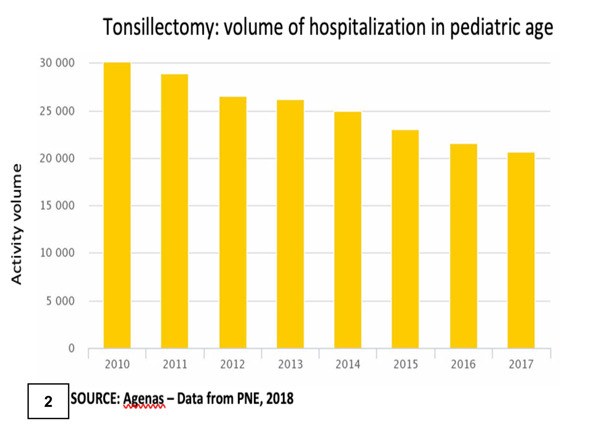
Adenotonsillectomy procedures, as can be seen in figures 1A, 1b, and 2, reporting PNE data, have shown a slow but progressive numerical reduction in recent years. Nonetheless, based on data from the SDO (Schede di Dimissione Ospedaliera), in the period 2007 to 2012 the mean incidence of post-surgical hemorrhages had a statistically significant increase, with geographical percentage variations between 0,02% and 1.38%, whereas, in 2013, homogeneous values of 0.69% were reported for the whole national territory.
Figure 1.
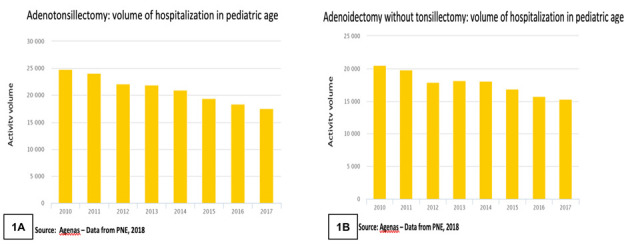
Figure 2.
Tonsillectomy has perioperative morbidity of approximately 2%. The overall incidence of post-surgical complications, as reported in the literature, ranges from 8% to 14% (1), whereas postoperative mortality is close to that of general anaesthesia alone, with one death per 10,000-35,000 cases (2.3). In Italy, in the three years 1999-2001 (Matter), one death per 95,000 was reported. However, it is difficult to obtain accurate data on real mortality based on scientific literature and data from the press.
The main mortality causes can be identified in complications related to anaesthesia and haemorrhage. Postoperative haemorrhage has an overall incidence between 0.5% and 24%. This wide range is because the various studies available in the literature are uneven: many authors only reported haemorrhages requiring surgical treatment, whereas other authors included also bleeding episodes that were managed in an outpatient setting with medical therapy alone. Blakely, in a review of 63 publications, reported a hemorrhagic incidence of 4.5%, with a standard deviation of 9.4%. Lowe, in an audit in the United Kingdom in 2007, reported a hemorrhagic incidence of 3.5% on a total of 34.000 tonsillectomies, but only 0.9% of cases required surgical hemostasis (4). Post-adenoidectomy haemorrhages have a lower incidence rate, approximately 0.8%, regardless of the surgical technique used.
The literature also shows that children under six years of age have approximately three times lower bleeding risk than children over six years of age. Males have a 1.3-fold higher hemorrhagic risk rate than females. Furthermore, different diagnoses present a different intrinsic risk: patients undergoing surgery for adenotonsillar hypertrophy have shown a lower hemorrhagic risk compared to patients undergoing surgery for recurrent infections. As far as the surgical technique is concerned, the use of cold instruments is related to a lower bleeding risk (1.2%) than the electrocauterization technique (6%) (5). Table 1 reports the classification of the main complications following surgery.
Table 1.
Complications classified on the time of onset as follows:
| Immediate onset | Medium onset | Late onset |
Anesthesiological:
|
Velo-pharyngeal insufficiency:
|
Chronic pharyngitis |
Hemorrhagic:
|
Voice alterations:
|
Facial pain and dysphagia due to ossification of the stylohyoid ligament (Eagle’s syndrome) |
Oral cavity lesions:
|
Neurological complications:
|
|
Local infections:
|
Compensatory hypertrophy of the remaining lymphatic tissue (lingual tonsil) | |
Regional infections:
|
Emotional trauma | |
| Subcutaneous emphysema or pneumomediastinum | ||
| Grisel’s syndrome |
Hemorrhagic complications
The tonsillar lodge presents a rich vascularization that comes from the external carotid artery (ECA). The main arterial blood supply is provided by the tonsillar artery, which originates from the ascending palatine artery and the ascending pharyngeal artery. These vessels can branch either from the lingual artery at a 90° angle or directly from the ECA. The palatine artery and the ascending pharyngeal artery give rise to the tonsillar arteriolar branches (polar branches), which perforate the pharyngeal constrictor muscle and run towards the tonsillar parenchyma. The veins form a tributary plexus of the pharyngeal plexus. Innervation is supplied by the tonsillar plexus, located on the lateral wall and formed by branches of the lingual nerve and the glossopharyngeal nerve.
Based on the time of onset, postoperative haemorrhages can be divided into:
immediate
delayed
late
or into:
primary: presenting in the first 24 hours (< 5%)
secondary: presenting within two weeks, but generally between the 6th and 10th postoperative day; bleeding episodes have been reported in the literature up to 55 days after surgery (6,7).
Immediate haemorrhages are usually complications of ineffective or incongruous intraoperative hemostasis due to inadequate cauterization of a blood vessel, imperfect arterial ligation, accidental detachment of a ligation snare, reduction or loss of the tensile strength of the suture from salivary stagnation, or a hypertensive peak or agitation upon awakening.
In the case of deficiency of coagulation factors or thrombocytopenia, it is important to provide adequate therapy or pre-intraoperative prophylaxis.
Late or secondary haemorrhages, on the other hand, are usually caused by eschar falling, generally occurring between the 6th and the 10th postoperative day, but inappropriate postoperative patient behaviour can also favour this process.
Among the causes, vascular disruptures should be taken into considerations as well. They can be caused by:
Local necrosis
Anomalous or aberrant vessels originating from the internal or external carotid artery
Arterial loops
Traumatic pseudoaneurysms
Septic arteritis
Exposition or rhexis of major vessels (facial artery, lingual artery, ascending palatine artery…)
Although the percentage of hemorrhagic complications is low in the various casuistries, it should not be forgotten that they may represent a dramatic emergency. Besides, recurrent late haemorrhages, albeit mild, should never be underestimated: for this reason, patients presenting even with a low-entity bleeding episode should always be hospitalized (7).
In case of a hemorrhagic event, the measures are very varied. Depending on the severity of the bleeding, local hemostasis by infiltration with a solution of 1% xylocaine with a vasoconstrictor may be sufficient, or surgical revision of the tonsillar lodge may be required. In the latter case, different procedures might be performed, ranging from ligation of tonsil pillars or tamponade of the tonsillar lodge to ligation of the ECA or embolization of one of its branches (8,9,6,10).
Respiratory complications
In recent years we have also seen an improvement in anaesthesia techniques, which has resulted in greater safety in some procedures, including tonsillectomy. Nonetheless, it should not be forgotten that, in this peculiar situation, the anaesthetist and the Otolaryngology surgeon are to interact on the same surgical field, so it is not infrequent that, during the surgical manoeuvres, the endotracheal tube can be bumped, bent or dislocated, so as to determine hypoventilation or even extubation of the patient (6,7,11,12).
Consequently, respiratory complications can result from hypoxic phenomena and suffocation caused by:
blood ab ingestis
irritative laryngeal spasm during haemorrhage
insufficiency or delays in orotracheal intubations
severe OSAS
obesity
drugs: promethazine, morphine and its derivatives, inducing breath depression, apnea, contractions and eventually cardiac arrest, etc.
Infectious complications
Infectious complications are now a rare occurrence, although data from the literature show an incidence between 6% and 41%, with a higher frequency in children affected by recurrent acute otitis media or recurrent pharyngotonsillitis (13). On the contrary, transient bacteremia is a frequent occurrence. The most commonly isolated pathogen is Haemophilus influenzae, but Streptococcus viridans, Streptococcus pneumoniae, and Staphylococcus aureus have been isolated from blood cultures with a certain frequency, as well. Minor complications reported in the literature include pneumonia and urinary tract infections, whereas, among the major complications, sporadic cases of meningitis (14), cerebral abscess, sepsis and osteomyelitis at distant sites (15) have been described. Cervical osteomyelitis can occur after tonsillectomy or adenoidectomy procedures. It is caused by the spreading of the infectious process either through the cervical planes, the blood vessels or the lymphatic system. The clinical onset is often insidious.
Internal jugular vein thrombosis, known as Lemierre Syndrome, has also been reported. This condition results from an initial thrombosis involving the tonsillar vein with subsequent spreading to the internal jugular vein and, occasionally, also to the cavernous sinus.
Traumatic complications
Traumatic complications, taken as a whole, are more frequent than previously considered. They are mostly due to patient positioning manoeuvres, incongruous tools, defective electrical insulation equipment, direct or inadequate heat transfer, and operator-related errors.
The most frequent complications are:
Grisel syndrome, i.e., subluxation or displacement of the atlantoaxial joint (C1 on C2). This occurrence is more frequent in children affected by Down’s syndrome due to increased ligament laxity (16,17);
perforation of the posterior tonsil pillar, velar or velopharyngeal injury;
dental trauma with rupture, dislocation or avulsion of dental elements;
dislocation of the temporomandibular joint (18);
hematoma of the tongue;
pseudoaneurysm of the lingual artery (19) or, more rarely, of the external or internal carotid arteries (20)
The late complications from surgical trauma include:
rhinolalia;
velar insufficiency, sometimes accompanied by dysphagia and nasal regurgitation of food (21);
oropharyngeal stenosis
Other complications
Haematological and metabolic complications are very rare, as well as neurological complications. The latter include the appearance of dysgeusia, and hypoglossal nerve or lingual nerve deficit caused by surgical or anesthesiological manoeuvres (20,21).
However, it is important to be aware of these potential complications as well, to make a timely diagnosis that allows early therapy.
Conclusions
Tonsillectomy is one of the oldest procedures in Otolaryngology: in fact, the first description dates back to 30 BC and is reported in the encyclopedic treatise on the medical art “De Medicina” by Aulus Cornelius Celsus. Despite the refinement and the evolution of surgical and anesthesiological techniques, this procedure should not be considered “banal and risk-free”: complications are not so rare and sometimes they can be serious, leading to the death of the patient. Therefore, it is of uttermost importance to assess the indications to tonsillectomy very carefully, using the available guidelines as a reference. The surgical and anesthesiological teams should be well-trained. During the surgical procedure, dissection should be performed carefully, avoiding extensive coagulation and manoeuvres which might result in potential local infectious complications. In case of a hemorrhagic complication, an immediate and correct diagnostic and therapeutic approach is essential; especially, recurrent hemorrhagic manifestations, albeit mild, should not be underestimated. In the end, organizational aspects must not be neglected. The hospitalization regimen in Italy varies from day surgery and one-day surgery to ordinary hospitalization, and the must go beyond the purely economic aspects of DRG (Diagnosis-Related Group) and LEA (Livelli Essenziali di Assistenza) tariffs. Not least the importance of obtaining appropriate Informed Consent, with a written form containing precise and punctual information to be provided to parents by the surgeon. Moreover, information regarding the clinical and surgical process should be addressed directly to the patient even in the case of a minor; such information must be adapted to the age of the young patient.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Randall D, Hoffer ME. Complications of tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surgery. 1998;118:61. doi: 10.1016/S0194-5998(98)70376-6. [DOI] [PubMed] [Google Scholar]
- 2.Har-El G, Nash M. Tonsillectomy and adenoidectomy. In: Krespi Y, Ossoff R, editors. Complications in head and neck surgery. Philadelphia: Sanders; 1991. pp. 75–98. [Google Scholar]
- 3.Kavanagh K, Beckford N. Adenotonsillectomy in children: indications and contraindications. South Med J. 1988;81:507–11. doi: 10.1097/00007611-198804000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Lowe D, Van der Meulen J, Cromwell D, et al. Key Messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117:717–24. doi: 10.1097/mlg.0b013e318031f0b0. [DOI] [PubMed] [Google Scholar]
- 5.Spector Z, Saint-Victor Kay DJ, Mandell DL. Risk factors for pediatric post-tonsillectomy haemorrhage. Int J Pediatr Othorhinolaryngol. 2016 May;84:151–5. doi: 10.1016/j.ijporl.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Ferrario F. La tonsillectomia: una tecnica che si rinnova Quadrni Monografici Aggiornamento AOOI. 2005 [Google Scholar]
- 7.Mansi N. Adenotonsillectomia: un problema ancora aperto Relazione Ufficiale XXIV Congresso Nazionale SIOP, Roma. 2017 [Google Scholar]
- 8.Arora R, Saraiya S, Niu X, Thomas RL, Kannicheswaran N. Post-tonsillectomy haemorrhage: who needs intervention? Int J Pediatr Othorhinolaryngol. 2015 Feb;79(2):165–9. doi: 10.1016/j.ijporl.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 9.Perkins JN, Liang C, Shultz L, Friedman NR. Risk of post-tonsillectomy haemorrhage by clinical diagnosis. Laryngoscope. 2012 Oct;122(10):2311–5. doi: 10.1002/lary.23421. [DOI] [PubMed] [Google Scholar]
- 10.Windfhur JP, Schloedorff G, Baburi D, Kremer B. Serious post-tonsillectomy haemorrhage with and without a lethal outcome in children and adolescents. Int J Pediatr Othorhinolaryngol. 2008 Jul;72(7):1029–40. doi: 10.1016/j.ijporl.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 11.SIAARTI (Società Italiana Anestesia Analgesia Rianimazione e Terapia Intensiva): raccomandazioni Clinico-Organizzative per l’Anestesia in Day Surgery. Minerva Anestesiol. 2000;66:915–926. [PubMed] [Google Scholar]
- 12.Sistema Nazionale per le Linee Guida: Appropriatezza e Sicurezza degli interventi di tonsillectomia e/o adenoidectomia. Istituto Superiore di Sanità, documento 15 marzo. 2008. www.snlg-iss.it .
- 13.Esposito S, Marchisio P, Capaccio P, Bellasio M, Semino M, Dusi E, Colombo R, Pignataro L, Principi N. Risk factors for bacteriemia during and after adenoidectomy and/or adenotonsillectomy. J Infect. 2009;58(2):113–8. doi: 10.1016/j.jinf.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka J, Kurosaki T, Kameyama Y, Mitsuda T, Ishiwada N, Kohno Y. Complications of adenotonsillectomy: a case report of meningitis due to dual infection with non-typeable Haemophilus influenza and Streptococcus peumoniae, and a prospective study of the rate of postoperative bacteriemia. Jpn J Antibiotic. 2013;66(4):205–10. [PubMed] [Google Scholar]
- 15.Wilson PF, Wannemuehler TJ, Matt BH. Invasive group A Streptococcus resulting in sepsis and abdominal wall abscess after adenotonsillectomy. Laringoscope. 2015 May;125(5):1230–2. doi: 10.1002/lary.24997. [DOI] [PubMed] [Google Scholar]
- 16.Sia KJ, Tang IP, Kong CK, Nasriah A. Grisel’s syndrome: a rare complication of tonsillectomy. J Laryngol Otol. 2012;126(5):529–31. doi: 10.1017/S0022215112000175. [DOI] [PubMed] [Google Scholar]
- 17.Spennato P, Nicosia G, Rapanà A, Cicala D, Donianni T, Scala S, Aliberti F, Cinalli G. Grisel Syndrome following adenoidectomy: Surgical Management in a case with delayed diagnosis. World Neurosurg. 2015;84(5):1494–7. doi: 10.1016/j.wneu.2015.04.060. [DOI] [PubMed] [Google Scholar]
- 18.Handa KK, Shunyu NB. Post-traumatic pseudoaneurysm of the lingual artery. Indian J Otolaryngol Head and Neck Surg. 2008;60(4):356–9. doi: 10.1007/s12070-008-0115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Nieuwenhove Y, Van den Branden P, van Tussenbroek F, Debing E, von Kemp K. Iatrogenic carotid artery pseudoaneurysm treated by an autologous vein-covered stent. Eur J Vasc Endovasc Surg. 1998 Sep;16(3):262–5. doi: 10.1016/s1078-5884(98)80230-x. [DOI] [PubMed] [Google Scholar]
- 20.Maini S, Osborne JE, Fadl HM. Et al, Temporomandibular joint dysfunction following tonsillectomy. Clin Otolaryngol Allied Scid. 2002;27:57–60. doi: 10.1046/j.0307-7772.2001.00528.x. [DOI] [PubMed] [Google Scholar]
- 21.Haapanen ML, Ignatius J, Rihkanem H, et al. Velopharyngeal insufficiency following palatine tonsillectomy. Eur ArchOtorhinolaryngol. 1994;251:186–9. doi: 10.1007/BF00181834. [DOI] [PubMed] [Google Scholar]


