Abstract
Background
The aim of this study was to investigate the clinical presentations, patterns of soft-tissue injuries, and outcomes of treatment of elbow dislocations in patients with preexisting cubitus varus.
Methods
Four cases of elbow dislocation in patients with preexisting cubitus varus, which were treated at 3 residency training hospitals, were retrospectively reviewed. Soft-tissue injury patterns were investigated using magnetic resonance imaging (MRI). Clinical outcomes were assessed at an average of 50.8 months (range, 34–82 months) after treatment using the Mayo Elbow Performance Score (MEPS) and the Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) score.
Results
The mean patient age was 49.5 years (range, 33–57 years). All patients had a posteromedial elbow dislocation, which was an indirect injury caused by a fall onto an outstretched hand. One patient had failed closed reduction; 3 others had redislocation or gross instability after closed reduction. Significant tears of the lateral collateral ligament complex and common extensor group were shown in MRI. All patients had surgical treatment including lateral complex repair only (n = 2), repair of both sides' complexes (n = 1), and corrective osteotomy with lateral complex repair (n = 1). At the final follow-up, the mean MEPS was 92.5 ± 8.7 and the mean QuickDASH score was 4.5 ± 6.4.
Conclusions
Elbow dislocation in patients with preexisting cubitus varus may present as posteromedial dislocation with acute instability. Surgical treatment of this injury led to acceptable clinical outcomes.
Keywords: Elbow, Varus deformity, Joint dislocation, Treatment outcome
Cubitus varus is the most common complication of pediatric supracondylar fractures. It not only is a cosmetic problem but also has important functional implications such as snapping medial triceps and posterolateral rotatory instability (PLRI), which is a common form of elbow instability.1) Lateral ulnar collateral ligament injury caused by substantial or minor repetitive trauma in patients with cubitus varus deformity may result in PLRI due to isochronous varus and external rotation forces.1)
Although the association between cubitus varus deformity and PLRI has been well documented,2,3,4) elbow dislocation in patients with preexisting cubitus varus is extremely rare and poorly characterized. Until now, only 3 cases of frank elbow dislocation in patients with preexisting cubitus varus have been reported.1,5,6) The aim of this study was to investigate the clinical presentations, soft-tissue injury patterns, and treatment outcomes of a series of elbow dislocations in patients with preexisting cubitus varus.
METHODS
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Keimyung University Dongsan Hospital (IRB No. 2019-04-014). Written informed consents were obtained. We conducted a retrospective review of 4 patients with preexisting cubitus varus who had been treated for frank elbow dislocation at 3 residency training hospitals between 2012 and 2017. Inclusion criteria were ipsilateral cubitus varus deformity caused by trauma in childhood and frank elbow dislocation confirmed by plain radiography at the initial injury or at ≤ 3 weeks after initial injury.
The initial treatment for all patients was closed reduction under sedation in the emergency department. For failed closed reduction or gross instability after closed reduction, surgical treatment was performed. Magnetic resonance imaging (MRI) was performed in all patients to evaluate injury patterns of soft tissues including ligaments, capsules, and muscles, as well as bone marrow edema patterns and associated intra-articular lesions.
The mean follow-up period was 50.8 months (range, 34–82 months). Clinical outcomes were assessed in terms of pain, joint stability, range of motion, and elbow function using the Mayo Elbow Performance Score (MEPS) and the Quick Disabilities of the Arm, Shoulder and Hand (Quick-DASH) score. The stability of the joint was estimated with valgus and varus stress tests and the pivot shift test. Complications were also evaluated.
RESULTS
Patient details are listed in Table 1. The mean age of the patients was 49.5 ± 11.1 years (range, 33–57 years), and there were 3 men and 1 woman. In 3 patients, the injury occurred in the non-dominant arm. One patient was injured in a fall from a standing position, 1 in a fall from a substantial height, 1 in a bicycle accident, and 1 in a fall downstairs. All patients reported a fall onto an outstretched hand, which caused an indirect injury.
Table 1. Details of the 4 Elbow Dislocations in Patients with Preexisting Cubitus Varus.
| Case | Age (yr) | Sex | Side | Injury type | Direction of dislocation | Closed reduction | Treatment | Side of operation | FU (mo) | MEPS | Quick DASH | Extension (°) | Flexion (°) | Pronation (°) | Supination (°) | Complication |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 54 | M | ND | Indirect | PM | ○ | S | Lat | 82 | 85 | 4.5 | 10 | 135 | 80 | 80 | |
| 2 | 33 | M | ND | Indirect | PM | ○ | S | Lat | 34 | 85 | 13.6 | 0 | 140 | 45 | 80 | |
| 3 | 54 | M | ND | Indirect | PM | ○ | S | Both | 38 | 100 | 0 | 5 | 135 | 80 | 80 | HO |
| 4 | 57 | F | D | Indirect | PM | × | S | Both | 49 | 100 | 0 | 0 | 140 | 80 | 80 |
FU: follow-up, MEPS: Mayo Elbow Performance Score, QuickDASH: Quick Disabilities of the Arm, Shoulder and Hand, ND: non-dominant, D: dominant, PM: posteromedial, S: surgery, Lat: lateral, HO: heterotopic ossification.
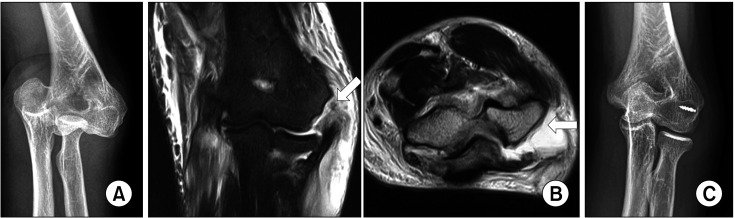
In all patients, posteromedial elbow dislocation was confirmed by plain radiography at the initial injury. None of them reported any discomfort or instability before dislocation except the cosmetic problem. One patient had failed closed reduction, 2 patients had redislocation after closed reduction, and 1 patient showed gross instability on physical examination after closed reduction. MRI revealed complete tears of the lateral collateral ligament (LCL) complex and common extensor group in all cases (100%). The lateral complex was retracted and torn from the lateral epicondyle (Fig. 1). On the medial side, a complete tear of the medial collateral ligament complex was shown in 1 case (25.0%) and partial tears in the remaining 3 cases (75.0%). The flexor-pronator group was intact without tears in 3 (75.0%) and was partially torn in the remaining 1 case (25.0%). The coronoid process had comminuted fractures of the anterolateral tip portion in 2 cases (50.0%) and avulsion fractures of the coronoid tip in the remaining 2 cases (50.0%). The capitellum had bony contusion in 2 cases (50.0%) (Table 2).
Fig. 1. (A) A 54-year-old man (case 1) with ipsilateral cubitus varus deformity (10°) in childhood trauma had posteromedial elbow dislocation. (B) Magnetic resonance images showing complete tears (white arrows) of the lateral collateral ligament complex and common extensor group. (C) Postoperative radiograph showing a congruent joint with varus deformity.
Table 2. Magnetic Resonance Imaging Findings for Injury Pattern.
| Case | MCL | Flexor/pronator | Trochlea | Coronoid | LCL complex | Common extensor | Radial head | Capitellum | Anterior capsule | Posterior capsule |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | P | N | N | A | T | T | N | N | T | P |
| 2 | P | N | N | A | T | T | N | C | P | P |
| 3 | T | P | N | F (AL tip) | T | T | N | N | T | T |
| 4 | P | N | N | F (AL tip) | T | T | N | C | T | T |
MCL: medial collateral ligament, LCL: lateral collateral ligament, P: partial tear, T: total tear, N: normal, A: avulsion, F: fracture, AL: anterolateral, C: contusion.
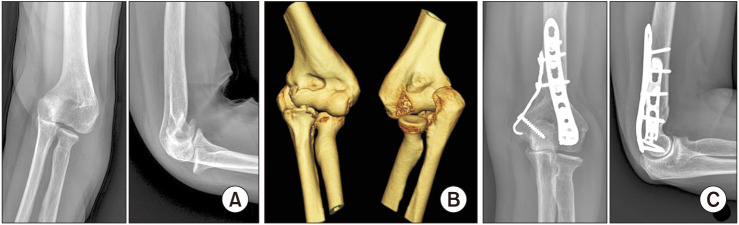
All patients had surgical treatment. The mean interval from the time of initial injury to surgery was 3.3 days (range, 1–5 days). Two patients had only LCL complex repair, and 1 had repair of both lateral and medial collateral ligament complexes. One patient had a corrective osteotomy for reducing the burden on the LCL after surgery with LCL complex repair and ulnar nerve anterior transposition (Fig. 2). All elbows were immobilized for postoperative 1 to 3 weeks in approximately 90° flexion. After immobilization, a hinged elbow brace was applied, and range of motion exercise was started.
Fig. 2. (A) A 57-year-old woman (case 4) with ipsilateral cubitus varus (23°) in childhood trauma had posteromedial elbow dislocation. (B) Three-dimensional computed tomographic images showing posteromedial elbow dislocation with comminuted fracture of the anterolateral coronoid tip portion. (C) Plain radiographs obtained after corrective osteotomy and repair of the lateral complex showing a congruent joint with correction of varus deformity.
At the final follow-up, the mean MEPS was 92.5 ± 8.7, and 2 patients were graded as excellent (50.0%) and 2 patients as good (50.0%). The mean QuickDASH score was 4.5 ± 6.4, and 3 patients were graded as excellent (75.0%) and 1 patient as good (25.0%). The mean range of motion was 3.8° ± 4.8° for extension, 137.5° ± 2.9° for flexion, 71.3° ± 17.5° for pronation, and 80° ± 0.0° for supination. No complications other than 1 case of heterotopic ossification without functional discomfort were observed.
DISCUSSION
In the present study, elbow dislocations in patients with preexisting cubitus varus were in a posteromedial direction with acute instability, which required surgical treatment. Surgical treatment of these injuries led to acceptable clinical outcomes. Also, clinical presentations and soft-tissue injury patterns on MRI allowed for inference of the sequential mechanism of elbow dislocation according to the direction of dislocation.
Elbow instability includes pathologic conditions ranging from a frank dislocation to the subtle PLRI.7) When a fall on the outstretched arm occurs, the preexisting pathology and abnormal mechanics of the elbow with cubitus varus deformity predispose the patient to PLRI or elbow dislocation. Regarding the mechanism of elbow dislocation, Rhyou and Kim8) suggested that the axial force applied through the forearm is likely to develop as the valgus distractive force due to the anatomical aspects of cubitus valgus, which helps to explain why posterolateral elbow dislocation is more common. They also insisted that posteromedial dislocation was caused by varus distractive rupture of the LCL complex and/or common extensor group with bony abutment at the medial aspect of the ulnohumeral joint.8) Then, pathologic forearm external rotation and a medial translational vector by the varus force against the upper arm might result in posteromedial dislocation.8) In the present study, all patients described a fall onto an outstretched hand, which caused an indirect injury, and posteromedial elbow dislocations were confirmed by plain radiography at the initial injury. These findings imply that major or minor traumatic events in patients with long-standing cubitus varus deformity may lead to posteromedial dislocation or PLRI because of anatomical alteration. We believe that cubitus varus deformity is vulnerable to varus force during a fall involving an outstretched hand and can easily result in posteromedial elbow dislocation. This is significant evidence that posteromedial dislocation starts from the lateral side by initial varus distractive force. Taken together, our results support the concept that the mechanism of posteromedial elbow dislocation starts from the lateral side with rupture of lateral structures induced by varus force and that it progresses to the medial side with subsequent variable energy dissipation.
Cho et al.9) reported that posteromedial elbow dislocations were correlated with a more severe soft-tissue injury, leading to a high rate of surgical treatment. In our study, significant tears of the LCL complex and/or common extensor group were shown in MRI in all cases. The torn LCL complex and common extensor group were retracted from the lateral epicondyle. These findings were also confirmed in the surgical field. However, the optimal surgical treatment for cubitus varus with elbow instability has not been established. O'Driscoll et al.4) reported 25 patients with coexisting cubitus varus and late-onset PLRI. Treatment mainly consisted of LCL reconstruction, corrective osteotomy, ulnar nerve anterior transposition, transfer of the medial head of the triceps tendon, or combinations. They observed that either ligament reconstruction alone or osteotomy alone produced a high failure rate in the presence of a varus deformity more than 15°. Thus, they recommended that the osteotomy be combined with ligament reconstruction for varus deformity more than 15°. Abe et al.2) reported that 4 patients with cubitus varus showed recurrent posterior dislocation of the radial head after further injury to the elbow. The recurrent dislocation was eliminated after tightening of the ligament and a supracondylar osteotomy of the humerus.
Osada et al.6) reported a case of constant PLRI after reduction of posterior dislocation of the elbow with ipsilateral preexisting cubitus varus. The patient was treated with closed reduction and plaster immobilization, but the elbow had a persistent PLRI with stiffness at 6 months after closed reduction and plaster immobilization. LCL complex reconstruction for PLRI and arthrolysis for stiff elbow were performed. On radiographs taken after closed reduction of this patient, the distal portion of the elbow joint was displaced medially and the radial head was subluxated posteriorly. Therefore, we think that it is reasonable to consider this as a posteromedial elbow dislocation. Arrigoni and Kamineni5) reported a case of PLRI, which was discovered after corrective osteotomy after reduction of posterior dislocation of the elbow with ipsilateral cubitus varus. They concluded that the PLRI was caused by the corrective osteotomy aimed at changing vectors rather than previous single elbow dislocation. In light of our results, we think elbow dislocation, rather than corrective osteotomy, might contribute to PLRI. Kontogeorgakos et al.1) reported a case of PLRI and snapping medial triceps in preexisting cubitus varus. The patient developed symptomatic PLRI at 8 years after injury, probably due to an additional trauma to the LCL complex following 2 posterior elbow dislocations. However, 3 previous studies for elbow dislocation in preexisting cubitus varus deformity did not mention precisely the direction of dislocation. In the present study, all patients had surgical treatment including lateral complex repair only in 2 patients, repair of both sides' complexes in 1 patient, and corrective osteotomy with lateral complex repair and ulnar nerve anterior transposition in 1 patient. Judging from these findings, PLRI may be a precursor or mild form of posteromedial elbow dislocation. We believe that PLRI can occur as a sequela of inadequate treatment of posteromedial elbow dislocation in patients with preexisting cubitus varus.
Our study has a few limitations. First, it is a retrospective study. Second, the treatment methods and outcomes could not be generalized because it was a multicenter study with a small sample. However, the significance of this study is that it investigated the clinical presentations, soft-tissue injury patterns, and treatment outcomes of a series of elbow dislocations in patients with preexisting cubitus varus.
Elbow dislocation in patients with preexisting cubitus varus may present as posteromedial dislocation and acute instability. Surgical treatment of these injuries led to acceptable clinical outcomes.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Kontogeorgakos VA, Mavrogenis AF, Panagopoulos GN, Lagaras A, Koutalos A, Malizos KN. Cubitus varus complicated by snapping medial triceps and posterolateral rotatory instability. J Shoulder Elbow Surg. 2016;25(7):e208–e212. doi: 10.1016/j.jse.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Abe M, Ishizu T, Nagaoka T, Onomura T. Recurrent posterior dislocation of the head of the radius in post-traumatic cubitus varus. J Bone Joint Surg Br. 1995;77(4):582–585. [PubMed] [Google Scholar]
- 3.O'Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation: a spectrum of instability. Clin Orthop Relat Res. 1992;(280):186–197. [PubMed] [Google Scholar]
- 4.O'Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am. 2001;83(9):1358–1369. doi: 10.2106/00004623-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Arrigoni P, Kamineni S. Uncovered posterolateral rotatory elbow instability with cubitus varus deformity correction. Orthopedics. 2009;32(2):130. [PubMed] [Google Scholar]
- 6.Osada D, Kameda M, Tamai K. Persistent posterolateral rotatory subluxation of the elbow in cubitus varus: a case report. Hand Surg. 2007;12(2):101–105. doi: 10.1142/S021881040700350X. [DOI] [PubMed] [Google Scholar]
- 7.Heo YM, Yi JW, Lee JB, Lee DH, Park WK, Kim SJ. Unstable simple elbow dislocation treated with the repair of lateral collateral ligament complex. Clin Orthop Surg. 2015;7(2):241–247. doi: 10.4055/cios.2015.7.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rhyou IH, Kim YS. New mechanism of the posterior elbow dislocation. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2535–2541. doi: 10.1007/s00167-011-1872-7. [DOI] [PubMed] [Google Scholar]
- 9.Cho CH, Kim BS, Rhyou IH, et al. Posteromedial elbow dislocations without relevant osseous lesions: clinical characteristics, soft-tissue injury patterns, treatments, and outcomes. J Bone Joint Surg Am. 2018;100(23):2066–2072. doi: 10.2106/JBJS.18.00051. [DOI] [PubMed] [Google Scholar]