Abstract
Backgroud
Femoral neck stress fractures (FNSFs) are rare but potentially disabling injuries if the diagnosis is missed or delayed and proper treatment is not provided. The aim of this study was to investigate and describe the characteristics and clinical course of FNSFs in South Korean male military recruits.
Methods
Between May 2015 and October 2019, 16 fractures in 12 young male military recruits were reviewed. The characteristics of the fractures were ascertained by detailed analysis of the history and clinical course, as well as radiographs, bone scintigrams, and magnetic resonance images.
Results
The median duration between endurance training and the development of hip pain was 5 weeks, while the median duration of pain before the patient sought medical attention was 3 weeks. Four patients (33.3%) exhibited bilateral fractures, and concomitant lesions involving the proximal tibia were found in 3 patients (25%). Fourteen of the 16 fractures (87.5%) were compression-type fractures, and surgery was performed for 7 hips. Complete union without malunion or osteonecrosis was achieved in all cases, and all cadets returned to their full activity levels in an average of 10 weeks.
Conclusions
We observed excellent prognosis of FNSFs. Our report highlights the importance of early reporting, detection, and treatment regarding the challenging management of FNSFs. When a military recruit reports hip pain, a FNSF should be considered; furthermore, the bilaterality of the fracture and the presence of concomitant lesions should also be investigated.
Keywords: Femoral neck, Stress fracture, Internal fixation
Femoral neck stress fractures (FNSFs) are rare, representing 5% of all stress fractures, and they are most prevalent among runners and military recruits.1,2) Despite the rarity, they have the potential to be one of the most serious injuries; if left untreated, subsequent fracture propagation and displacement increase the risk of avascular necrosis of the femoral head, nonunion, and osteoarthritis.3,4,5) To avoid misdiagnosis or delayed diagnosis, strong clinical suspicion and awareness of these injuries are of paramount importance.4,6)
FNSFs may occur along the medial or lateral margin of the neck, and their management is guided by the location and extent of the fracture.7,8) Stress fractures restricted to the superior surface of the femoral neck are termed tension-type fractures, while those restricted to the inferior surface are termed compression-type fractures. Tension-type fractures are potentially unstable and liable to displace without surgical fixation. Compression-type fractures, on the other hand, are mechanically stable and generally treated conservatively with non-weight-bearing and frequent radiographic follow-ups.5,9)
In South Korea, at the age of 18 years, all men become liable for compulsory military service for 22 months. They receive basic training during the initial 2 months of their service, during which high fitness levels are required. Individuals with poor physical conditioning or undiag nosed preexisting injuries exhibit worsening of their condition due to training and comprise the at-risk population for FNSFs.9,10,11) There are only a few studies on FNSFs, and most of these are case reports. To our knowledge, there is no case series involving South Korean military recruits.12,13)
Accordingly, the aim of this study was to investigate and describe the clinical presentation (fracture pattern, bilaterality, and other concomitant lesions), clinical course, and prognosis of FNSFs in South Korean male military recruits.
METHODS
Study Population and Diagnosis
The design and protocol of this retrospective study were approved by the Institutional Review Board (IRB No. AFCH-20-IRB-013), and the need to obtain informed consent was waived. In total, 12 young, South Korean male military recruits who underwent treatment for FNSFs between May 2015 and October 2019 at The Armed Forces Capital Hospital, South Korea, were included (Table 1). All patients were interviewed in order to collect pertinent data, including their physical activity levels, onset and duration of symptoms, trauma history, predisposing factors, and previous treatments. In all patients, bone scintigraphy was performed to identify any other stress fracture. Bilateral 3.0-T magnetic resonance imaging (MRI) of the hips was performed, and FNSFs were considered when marrow edema involving the femoral neck was observed on MRI in cases with negative findings in plain radiography.14) All prospectively collected images were retrospectively reviewed in consensus by 2 orthopedic surgeons with 15 (BHY) or 40 years of experience (HKY), in the diagnosis and treatment of femoral neck fractures.
Table 1. Demographic Characteristics of South Korean Military Recruits Treated for Femoral Neck Stress Fractures.
| No. | Sex/age (yr) | BMI (kg/m2) | Follow-up duration (mo) | Site | Fracture type | Fullerton & Snowdy | Duration from admission to pain development | Time from pain development to clinic visit | Initial radiographic result | Concomitant stress fracture | Surgical treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male/19 | 22.5 | 13 | Right | Compression/incomplete | Type 2 | Unknown | 2 wk | Negative | Both proximal tibia | IF using MCS |
| 2 | Male /20 | 24.5 | 6 | Left | Tension/incomplete | Type 4 | 2 wk | 6 wk | Negative | None | None |
| 3 | Male/21 | 22.2 | 12 | Right | Compression/incomplete | Type 2 | 4 wk | 1 day | Negative | None | IF using MCS |
| 4 | Male /20 | 21.7 | 9 | Left | Compression/complete | Type 2 | 5 wk | 1 wk | Positive | None | None |
| 5 | Male /20 | 23.9 | 6 | Right | Compression/incomplete | Type 2 | 6 wk | 1 wk | Negative | None | None |
| 6 | Male /20 | 19.9 | 16 | Left | Compression/complete | Type 2 | 2 wk | 3 wk | Positive | None | IF using MCS |
| 7 | Male /19 | 24.9 | 13 | Right | Compression/complete | Type 2 | 4 wk | 4 wk | Positive | None | IF using MCS |
| 8 | Male /20 | 26.1 | 6 | Right | Compression/incomplete | Type 2 | 6 mo | 8 wk | Negative | Left proximal tibia | None |
| Left | Compression/incomplete | Type 2 | Negative | None | |||||||
| 9 | Male /19 | 28.7 | 14 | Right | Compression/incomplete | Type 2 | Unknown | 8 wk | Negative | Left proximal tibia and fibula | None |
| Left | Compression/complete | Type 2 | Negative | IF using MCS | |||||||
| 10 | Male /20 | 29.3 | 7 | Right | Compression/incomplete | Type 2 | 1 wk | 3 day | Negative | None | IF using DHS |
| Left | Compression/displaced | Type 3 | Positive | IF using DHS | |||||||
| 11 | Male /18 | 20.2 | 6 | Right | Compression/incomplete | Type 2 | 3 wk | 8 wk | Positive | None | None |
| Left | Compression/complete | Type 2 | Positive | IF using MCS | |||||||
| 12 | Male /20 | 23.7 | 6 | Left | Tension/incomplete | Type 4 | 8 wk | 12 wk | Negative | None | None |
BMI: body mass index, IF: internal fixation, MCS: multiple cannulated screws, DHS: dynamic hip screw.
Classification and Treatment Plan
We categorized patients into 4 groups according to the Fullerton & Snowdy classification:15) type I, fracture on the tension side of the femoral neck; type II, fracture on the compression side of the femoral neck; type III, displaced fracture; and type IV, atypical, superiorly based, incomplete tension-type fracture. Fractures in the 4th category, added by Provencher, are routinely absent on plain radiographs and present on MRI.16)
The treatment of FNSFs was planned according to the location and extent of the fracture. According to previous reports, conservative treatment was planned for type II (incomplete compression < 50% of the femoral neck width) and type IV fractures, while surgery was planned for type I (tension-type fractures), type II (incomplete compression > 50% of the femoral neck width), and type III fractures. All internal fixations were performed using multiple cannulated screws or dynamic hip screws (DHSs) with a standard basic technique.17) After DHS fixation, an additional cannulated screw was inserted to prevent rotation.18)
For conservatively managed cases, restricted weight-bearing with crutches was allowed until the pain completely resolved; this normally takes between 6 and 8 weeks. Subsequently, weight-bearing on the injured side was gradually increased from non-weight-bearing to toe-touch weight-bearing to partial weight-bearing, depending on the degree of pain. For operated cases, non-weight-bearing or toe-touch weight-bearing with crutches was maintained for 4 weeks, followed by partial weight-bearing with crutches for further 6 weeks. In all cases, regular follow-up radiographs were obtained for determination of union and any other changes. As a guide, radiographs should be obtained weekly for the first 4 weeks, every 2 weeks for the next 4 weeks, and every 4 weeks for the next 8 weeks.
Outcomes and Statistical Analysis
We identified the anthropometric characteristics and configurations of the fractures as well as other concomitant stress fractures. The clinical course was ascertained by assessment of the duration between enlistment and fracture diagnosis, duration of pain before the patient visited the clinic, and union time and rate. Descriptive statistics are reported as median and range for continuous variables and total number and percentage for discrete variables by using Excel version 2016 (Microsoft, Redmond, WA, USA).
RESULTS
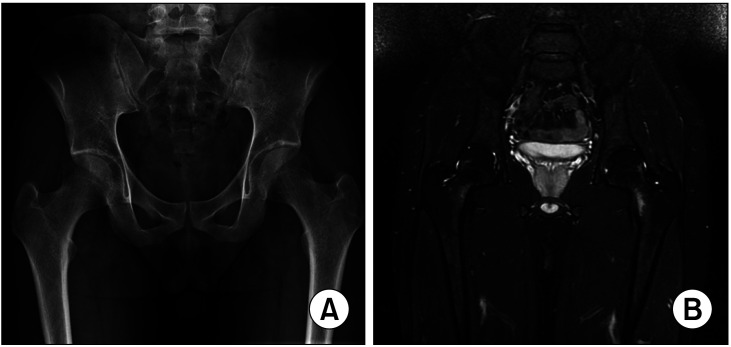
All patients were healthy military recruits with no remarkable history of disease or treatment with medication. Four patients (33.3%) exhibited bilateral fractures; thus, 16 hips of 12 patients were analyzed. All 4 patients diagnosed with bilateral fractures complained of unilateral hip pain and were later found to have an asymptomatic FNSF in the contralateral hip. Only 6 of the 16 (37.5%) hips were diagnosed on initial X-rays, and all FNFSs were confirmed by MRI (Fig. 1). The median age of the patients at the first hip fracture was 20 years (range, 18–22 years), and the median body mass index was 23.9 kg/m2 (range, 19.9–29.3 kg/m2).
Fig. 1. Imaging findings of a bilateral femoral neck stress fracture, which was treated by conservative treatment in a South Korean male military recruit. (A) An anteroposterior pelvis radiograph showing the femoral necks of both sides without specific findings. (B) A T2-weighted image showing hyperintensity around the inferior aspect of the femoral necks of both sides, and the extents of incomplete compression-type stress fractures were identified as < 50%. Complete union was achieved with conservative treatment.
The median duration between endurance training and the development of hip pain was 5 weeks (range, 1 week–6 months). The median duration of pain before the patient sought medical attention was 3 weeks (range, 1 day–3 months). Three of the 12 (25%) patients were subsequently diagnosed with stress fractures involving the proximal tibia by bone scanning.
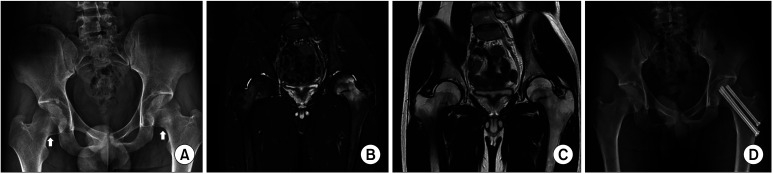
Compression-type fracture was the main fracture type (14 hips; 8 incomplete, 5 complete, and 1 displaced), followed by incomplete tension-type fracture (2 hips). Surgery was performed for 8 hips, and complete union was achieved without malunion or osteonecrosis in all cases (Fig. 2). All cadets returned to their full activity levels in an average of 10 weeks.
Fig. 2. Imaging findings of a bilateral femoral neck stress fracture, which was treated by operative treatment in a South Korean male military recruit. (A) An anteroposterior view of the pelvis showing sclerotic changes in the subcapital inferomedial areas (arrows) of both femoral necks. (B) A T2-weighted image showing hyperintensity around both subcapital fracture lines. (C) The extents of incomplete compression-type stress fractures in the right and left hips were identified as < 50% and > 50% of the femoral neck width, respectively, on a T1-weighted image. (D) A radiograph obtained at 6 months after surgery showing complete union of the fractures.
DISCUSSION
Although stress fractures are extremely rare in the general population, 4%–5% of all military trainees experience a stress fracture.1) One of the most significant stress fractures is FNSF, and it has been reported that FNSFs account for approximately 2% of all stress fractures in military recruits.1,2) To the best of our knowledge, the present study included the largest number of treated FNSFs in South Korean male military recruits.
An increasingly overweight and less fit civilian population is transformed into military units through a modern military training program.19,20) The initial military training course is an intensive residential program that is uniform for all recruits. However, recruits with poor physical conditioning have to be trained at the highest fitness levels ever experienced in their lives.3,21) One underlying physiological effect of insufficient preservice physical activity is inadequate adaptation of bones and other connective tissues to high-impact activities such as running, cutting, and jumping.10,22,23) Arguably, FNSFs are the most devastating bone stress injury.8) Loss of the shockabsorbing effects of the gluteus medius and minimus muscles, which are significant stabilizers of tensile forces at the superior aspect of the femoral neck, results in FNSFs when the muscles become fatigued under repetitive high stress.7,8)
In the present study, the median duration of endurance training before the development of hip pain was 5 weeks (range, 1 week to 6 months), which was comparable to that in previous reports.10,24) Thus, a high index of suspicion for FNSFs and prompt referral for bone scanning or MRI at the main military hospital are important for conscripts complaining of groin or proximal thigh pain.4) MRI should be performed even if plain radiographs show some sclerotic changes at the femoral neck, because this can aid in confirming bilateral FNSFs.11,25) MRI is also useful for diagnosing conditions other than FNSFs, such as osteonecrosis.3)
Concomitant stress fractures were found in 3 patients (25%) in our study, and all lesions involved the proximal tibia. An epidemiology study from the United States reported that 30% of all stress fractures involved multiple lower extremity bones,9) with the metatarsals and proximal tibia being the most common sites in American military cadets. Moreover, over 50% of all stress fractures occurred within 3 months of matriculation. Although MRI is the single best technique for the assessment of patients with stress fractures, bone scintigraphy is valuable for the exclusion of other stress fractures in cases where MRI findings are inconclusive.26)
In the present study, all cadets achieved bone union within a period consistent with that in previous reports (6 to 12 weeks after surgery).10,14,23) The majority of FNSFs are caused by compressive-type forces, which occur at the inferior aspect of the neck. Otherwise, tension-type FNSFs are not common but more vertical and unstable in nature, so there is a high delayed union and nonunion rate in the bone healing process.27) The incidence of compressive-type fractures in the present study was 87.5% (14/16), similar to the values in previous studies.3) Displaced fractures are reportedly associated with many complications; however, there was only 1 case in the present study. We believe that early reporting to the hospital and treatment allowed for early detection and led to excellent outcomes. It should be noted that the findings of physical examination in earlier reports were nonspecific and that the duration of symptoms or pain could not be used to differentiate FNSFs from other diagnoses.7,22,28)
This study has 2 major limitations. First, it was retrospective and involved a small number of patients. This limitation was unavoidable because FNSFs are rare. Second, we did not investigate or consider possible risk factors such as decreased mineral density in the femoral bone, severe exercise, poor baseline physical fitness levels, and other anatomical factors.
In conclusion, to our knowledge, this is the first study to describe FNSFs in South Korean military recruits. Stress fractures are best managed through early detection so the excellent prognosis observed in our study might have resulted from early reporting and treatment. When an individual subjected to repetitive loading of the femoral neck, such as a military recruit, reports hip or groin pain, an FNSF should be considered. Furthermore, the bilaterality of the fracture and the presence of concomitant lesions should also be investigated. For prevention of stress fractures, future studies should investigate causes and risk factors (insufficient preservice physical activity), which can be modified before basic combat training.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Takkar P, Prabhakar R. Stress fractures in military recruits: a prospective study for evaluation of incidence, patterns of injury and invalidments out of service. Med J Armed Forces India. 2019;75(3):330–334. doi: 10.1016/j.mjafi.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waterman BR, Gun B, Bader JO, Orr JD, Belmont PJ., Jr Epidemiology of lower extremity stress fractures in the United States Military. Mil Med. 2016;181(10):1308–1313. doi: 10.7205/MILMED-D-15-00571. [DOI] [PubMed] [Google Scholar]
- 3.Robertson GA, Wood AM. Femoral neck stress fractures in sport: a current concepts review. Sports Med Int Open. 2017;1(2):E58–E68. doi: 10.1055/s-0043-103946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatnagar A, Kumar M, Shivanna D, Bahubali A, Manjunath D. High incidence of stress fractures in military cadets during training: a point of concern. J Clin Diagn Res. 2015;9(8):RC01–RC03. doi: 10.7860/JCDR/2015/12535.6282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sjolin SU, Eriksen C. Stress fracture of the femoral neck in military recruits. Injury. 1989;20(5):304–305. doi: 10.1016/0020-1383(89)90178-2. [DOI] [PubMed] [Google Scholar]
- 6.Clough TM. Femoral neck stress fracture: the importance of clinical suspicion and early review. Br J Sports Med. 2002;36(4):308–309. doi: 10.1136/bjsm.36.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konetsky M, Miller J, Tripp C. Femoral neck stress fracture. J Orthop Sports Phys Ther. 2013;43(4):275. doi: 10.2519/jospt.2013.0407. [DOI] [PubMed] [Google Scholar]
- 8.Egol KA, Koval KJ, Kummer F, Frankel VH. Stress fractures of the femoral neck. Clin Orthop Relat Res. 1998;(348):72–78. [PubMed] [Google Scholar]
- 9.Cosman F, Ruffing J, Zion M, et al. Determinants of stress fracture risk in United States Military Academy cadets. Bone. 2013;55(2):359–366. doi: 10.1016/j.bone.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Kupferer KR, Bush DM, Cornell JE, et al. Femoral neck stress fracture in Air Force basic trainees. Mil Med. 2014;179(1):56–61. doi: 10.7205/MILMED-D-13-00154. [DOI] [PubMed] [Google Scholar]
- 11.Thomas R, Wood AM, Watson J, Arthur CH, Nicol AM. Delay in diagnosis of neck of femur stress fracture in a female military recruit. J R Nav Med Serv. 2012;98(2):27–29. [PubMed] [Google Scholar]
- 12.Yoon BH, Kwon MS. Atraumatic bilateral fracture of the femoral neck in young male patient with suspected osteomalacia. J Bone Metab. 2017;24(3):197–200. doi: 10.11005/jbm.2017.24.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santoso A, Joo SD, Lee DH, Seol YJ, Park KS, Yoon TR. Bilateral femoral neck stress fracture presented with unilateral symptoms in a shipman laborer: a case report. Hip Pelvis. 2017;29(1):77–80. doi: 10.5371/hp.2017.29.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rohena-Quinquilla IR, Rohena-Quinquilla FJ, Scully WF, Evanson JR. Femoral neck stress injuries: analysis of 156 cases in a U.S. Military Population and Proposal of a New MRI Classification System. AJR Am J Roentgenol. 2018;210(3):601–607. doi: 10.2214/AJR.17.18639. [DOI] [PubMed] [Google Scholar]
- 15.Fullerton LR, Jr, Snowdy HA. Femoral neck stress fractures. Am J Sports Med. 1988;16(4):365–377. doi: 10.1177/036354658801600411. [DOI] [PubMed] [Google Scholar]
- 16.Provencher MT, Baldwin AJ, Gorman JD, Gould MT, Shin AY. Atypical tensile-sided femoral neck stress fractures: the value of magnetic resonance imaging. Am J Sports Med. 2004;32(6):1528–1534. doi: 10.1177/0363546503262195. [DOI] [PubMed] [Google Scholar]
- 17.Lee YK, Moon KH, Kim JW, Ha YC, Lee MH, Koo KH. Learning curve of internal fixation for nondisplaced femoral neck fractures: a cumulative sum analysis. Clin Orthop Surg. 2018;10(1):9–13. doi: 10.4055/cios.2018.10.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siavashi B, Aalirezaei A, Moosavi M, Golbakhsh MR, Savadkoohi D, Zehtab MJ. A comparative study between multiple cannulated screws and dynamic hip screw for fixation of femoral neck fracture in adults. Int Orthop. 2015;39(10):2069–2071. doi: 10.1007/s00264-015-2881-9. [DOI] [PubMed] [Google Scholar]
- 19.Knapik JJ, Darakjy S, Hauret KG, et al. Increasing the physical fitness of low-fit recruits before basic combat training: an evaluation of fitness, injuries, and training outcomes. Mil Med. 2006;171(1):45–54. doi: 10.7205/milmed.171.1.45. [DOI] [PubMed] [Google Scholar]
- 20.Knapik JJ, Sharp MA, Steelman RA. Secular trends in the physical fitness of United States Army Recruits on Entry to Service, 1975-2013. J Strength Cond Res. 2017;31(7):2030–2052. doi: 10.1519/JSC.0000000000001928. [DOI] [PubMed] [Google Scholar]
- 21.Yang S, Luo Y, Yang L, et al. Comparison of femoral strength and fracture risk index derived from DXA-based finite element analysis for stratifying hip fracture risk: a cross-sectional study. Bone. 2018;110:386–391. doi: 10.1016/j.bone.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Petrin Z, Sinha A, Gupta S, Patel MK. Young man with sudden severe hip pain secondary to femoral neck stress fracture. BMJ Case Rep. 2016;2016:bcr2016216820. doi: 10.1136/bcr-2016-216820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duquette TL, Watson DJ. Femoral neck stress fracture in a military trainee. J Orthop Sports Phys Ther. 2010;40(12):834. doi: 10.2519/jospt.2010.0421. [DOI] [PubMed] [Google Scholar]
- 24.Lee CH, Huang GS, Chao KH, Jean JL, Wu SS. Surgical treatment of displaced stress fractures of the femoral neck in military recruits: a report of 42 cases. Arch Orthop Trauma Surg. 2003;123(10):527–533. doi: 10.1007/s00402-003-0579-8. [DOI] [PubMed] [Google Scholar]
- 25.Raval P, Mayne AI, Yeap PM, Oliver TB, Jariwala A, Sripada S. Outcomes of magnetic resonance imaging detected occult neck of femur fractures: do they represent a less severe injury with improved outcomes? Hip Pelvis. 2019;31(1):18–22. doi: 10.5371/hp.2019.31.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beck BR, Bergman AG, Miner M, et al. Tibial stress injury: relationship of radiographic, nuclear medicine bone scanning, MR imaging, and CT Severity grades to clinical severity and time to healing. Radiology. 2012;263(3):811–818. doi: 10.1148/radiol.12102426. [DOI] [PubMed] [Google Scholar]
- 27.Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29(1):100–111. doi: 10.1177/03635465010290010201. [DOI] [PubMed] [Google Scholar]
- 28.Ejnisman L, Wajnsztejn A, Queiroz RD, Ejnisman B. Unusual presentation of a femoral stress fracture. BMJ Case Rep. 2013;2013:bcr2012007828. doi: 10.1136/bcr-2012-007828. [DOI] [PMC free article] [PubMed] [Google Scholar]