Abstract
In 2020, the novel COVID-19 pandemic replaced TB as the world’s top cause of death from an infectious disease. The October 21, 2020 the UN Secretary-General report on progress towards implementation of the UNHLM political declaration on TB stresses that although high-level commitments and targets had galvanized global and national progress towards ending TB, urgent and more ambitious investments and actions were required, especially in lieu of the COVID-19 pandemic where associated public health measures and travel restrictions, have disrupted health services universally. The report sets out 10 priority recommendations to get the world on track to reach agreed targets by 2022. Political commitment is more critical than ever. COVID-19 diagnostic and vaccination health services need to be aligned to TB services with active early case finding in communities, engaging the private sector care providers and mitigation of fear and stigma. Healthcare staff and community workers and leaders need to be provided with COVID-19 vaccination and personal protective equipment. The UNHLM declaration committed to mobilize 15 billion USD per annum for TB, of which 13 billion USD is for TB care and 2 billion USD per annum for TB R&D. The Global Fund needs to increase funding for TB. Learning from the unprecedented speed of COVID-19 vaccine development, fastracking development and evaluation of TB vaccines is essential. World leaders need to urgently address and reverse the socio-economic consequences of the COVID-19 pandemic and these will determine to what extent they will impact on achieving TB targets.
Keywords: Tuberculosis, TB, United Nations General assembly, End TB targets, Control, COVID-19
Introduction
The ongoing COVID-19 pandemic has disrupted lives and livelihoods and created unprecedented challenges for health systems across the world. In 2020, COVID-19 replaced Tuberculosis (TB) as the top infectious disease of death at the global level, but not in low- and middle-income countries (WHO, 2020). As of February 14th 2021, there have been more than 108 million confirmed cases of COVID-19, including over 2.3 million deaths, reported to WHO (WHO Covid-19 dashboard).
Prior to the onset of the COVID-19 pandemic the global fight against TB received a much-needed boost with the 2018 United Nations High Level Meeting (UNHLM) which resulted in a political declaration with bold commitments and targets for TB to be achieved by the end of 2022 (United Nations, 2018, Stop TB Partnership, 2019). The 2018 UN General Assembly (UNGA) Political Declaration on Tuberculosis was truly a pivotal turning point in global efforts to end the TB epidemic. Ambitious targets were set for diagnosing and treating an additional 40 million people with TB by 2022, mobilizing US$13 billion annually for TB care and prevention and $2 billion per year for research and development.
Progress towards UNGA TB Targets: 2018-2019
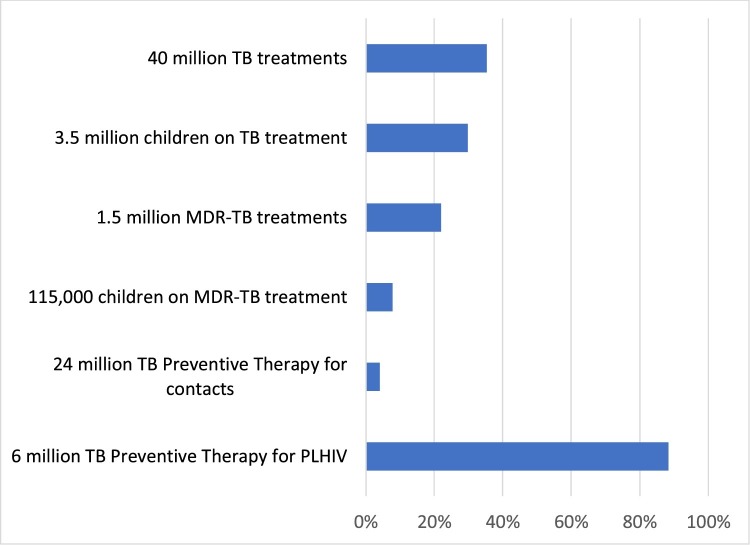
In 2018 and 2019 some progress was made against most of the targets (Figure 1 ) (WHO, 2020; Sahu et al., 2020). The world treated more people with TB and drug-resistant TB than ever before, reducing the number of people missing from care from 4 million to less than 3 million a year. TB preventive therapy was prioritized by high TB burden countries for the first time. Despite good progress, the world was not yet on track to reach the UNHLM TB prevention and care targets for 2022.
Figure 1.
Progress in 2018-2019 against UNHLM global cumulative treatment targets for period 2018-2022.
On October 21, 2020 the United Nations Secretary-General António Guterres, issued a report highlighting progress being made towards the achievement of UNGA global TB targets and implementation of the UNHLM political declaration on TB (United Nations, 2020). The report stressed that although high-level commitments and targets had galvanized global and national progress towards ending TB, urgent and more ambitious investments and actions were required, especially in the context of the COVID-19 pandemic. It noted that high-level commitments and targets have galvanized global and national progress towards ending tuberculosis but called for urgent and more ambitious investments and actions. The report emphasized that despite recent achievements in reducing TB incidence and deaths, and closing gaps in access to prevention and care, the gains remained fragile. The report lists 10 priority recommendations to get the world on track to reach agreed targets by 2022.
Setback and impact due to the COVID-19 pandemic
In 2020, as the COVID-19 pandemic spread across high TB burden countries, their TB health services were disrupted (Fei et al., 2020, Alene et al., 2020). Recognizing that both TB and COVID-19 were airborne respiratory infections several countries used their TB programmes as a launch pad for mounting a response against COVID-19, diverting some cadres of staff, certain specialized health facilities and laboratories from TB to COVID-19. While this was good for addressing COVID-19 it adversely impacted TB prevention and care delivery. At the same time people faced barriers in accessing TB care and diagnostic services due to restrictions in mobility, fear and stigma. The biggest impact was on TB diagnosis and enrolment on treatment which plummeted down in most high TB burden countries. Impacts were also seen on other areas of TB prevention and care and also on TB research and development. A study done by civil society highlighted the array of disruptions in the global fight against TB (Multiple Partners, 2020). A modelling study (Stop TB Partnership, 2020, Cilloni et al., 2020) shows that due to the COVID-19 pandemic-related lockdowns and restrictions, between 2020 to 2025 the global TB incidence could increase by 6.3 million and mortality up by 1.5 million. This would mean a setback of 5-8 years in the global response to TB.
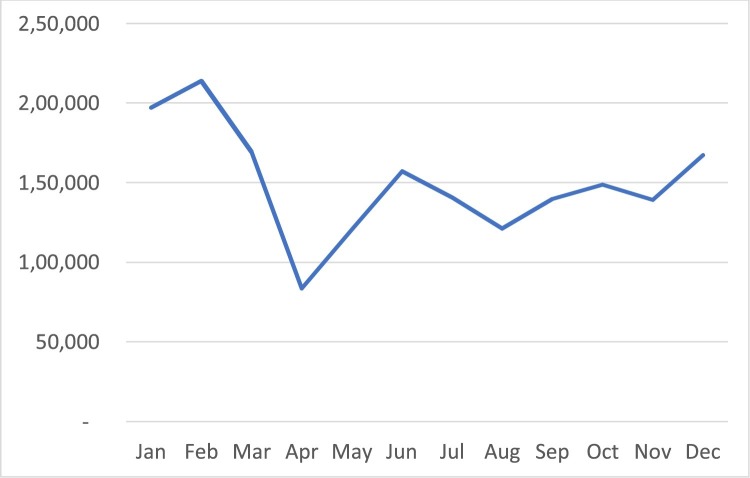
Unlike COVID-19, TB notification data of most countries are not available publicly on a real-time daily basis, but on annual and quarterly frequency. India is an exception, with real-time TB notification system which is publicly available (Govt. of India and Nikshay, 2020). This real-time TB data was extremely useful in India to rapidly detect the problem in 2020, take corrective measures and monitor progress. Figure 2 shows how TB notification in India fell dramatically immediately after announcement of the lockdown on 23rd March 2020. Recovery from this dramatic drop did not happen by default, but because of a massive effort by the TB programme in India which included active TB screening and testing in the community, expansion of rapid molecular testing sites in the country, bidirectional COVID-19 and TB testing, vulnerability mapping of communities, restarting of private clinics and launch of a people’s movement against TB called “Jan Andolan”. These efforts were possible because of existing high level of political commitment by the Prime Minister and the Health Minister of India, and funding made available to the TB programme. TB diagnosis and enrolment increased in the later part of 2020 but overall annual TB notification in 2020 fell short by 25% when compared to 2019. Since the ‘clock is ticking’ more efforts will be required for achieving UNGA TB targets. Sharp declines in TB notification rates were also seen in other high TB burden countries in 2020 (WHO, 2020; The Union, 2020). In general, countries in Asia had a higher decline in TB notification when compared to Africa and other parts of the world. TB patients coinfected with SARS-CoV-2 appear to have three times the mortality of patients who have TB alone (Kumar et al., 2021). The extent of overlap between TB and COVID-19 and impact on mortality and long-term functional recovery, needs to be further researched.
Figure 2.
Monthly TB notification in 2020 in India.
The socio-economic consequences of the COVID-19 pandemic are unfolding. The COVID-19 pandemic increased some of the important risk factors for TB such as malnutrition, poverty and social inequities. WHO had estimated that 22% of the global TB burden in 2019 could be attributed to undernutrition (WHO, 2020). TB thrives in impoverished and socio-economically marginalized settings. How quickly world leaders can address and reverse these socio-economic consequences of the COVID-19 pandemic will determine to what extent they will impact incidence and mortality due to TB.
The widespread use of masking and social distancing is anticipated to reduce transmission of TB, particularly transmission occurring outside the household. South Africa’s national COVID-19 response has generated unprecedented mobilization of resources and has focused the political agenda on health and underlying social determinants that increase vulnerability and mortality. The resulting political and public participation for COVID-19 must also now include HIV and tuberculosis (Keene et al., 2020). Further operational and socio-economic research is needed in this area.
Priority actions needed to overcome the impact of COVID-19 pandemic and achieve the UNHLM targets
Considering the huge setback of the global TB response in 2020 due to the COVID-19 pandemic we recommend three key priority actions in 2021 for high TB burden countries and stakeholders: Recovery; increased financing; and building back better TB responses. For these three actions to happen high-level political commitment is critical.
First, all high TB burden countries need to urgently develop recovery plans and implement them. Such plans should focus on TB diagnosis, by scaling up screening and testing for TB using rapid molecular tests, contact investigations, TB testing for COVID-19 patients, active TB case finding in communities, engaging with private sector care providers and address fear and stigma. Health and community workers need to be provided with COVID-19 vaccination and personal protective equipment, and people needing care should be reached in their communities and homes. The approaches for early detection of people with TB need to be tailored to the local setting. Recovery needs to happen in a campaign mode with urgency and at scale. This could be in the form of a hundred-day, or six-months, massive surge in TB screening and testing of all contacts and vulnerable people in the community, and TB testing of symptomatic people undergoing COVID-19 testing.
Increased financing for TB is critical. The UNHLM political declaration had committed to mobilize 15 billion USD per annum for TB, 13 billion USD for TB care and prevention and 2 billion USD per annum for TB research and development. Currently only half of this funding is available (WHO, 2020; Treatment Action Group (TAG) and Stop TB Partnership, 2020). A report by communities identifies such gaps as a “deadly divide” between commitments and realities and calls for urgent action to close the gap (Stop TB Partnership delegations, 2020). TB responses in low- and middle-income countries are funded by domestic budgets and external funds. The proportion of domestic funding is large in several middle-income countries, but most low-income countries depend heavily on external funding. During the COVID-19 pandemic it is important to maintain and further increase the domestic funding commitments for TB. The main sources of external funding for TB are the Global Fund to Fight AIDS, Tuberculosis and Malaria and the USAID, but the Global Fund allocates only 18% of its resources to TB. Considering that TB kills more people than HIV and Malaria put together, the Global Fund needs to increase funding for TB. The Global Fund has disseminated guidance for countries to develop plans to mitigate the impact of COVID-19 on TB services (The Global Fund, 2020), but it is important that additional funding for such plans must be made available and countries should have systems in place for absorbing the funds and delivering results. The World Bank and Regional Development Banks need to step up with concessional loans, grants and blended financing made available to high TB burden countries. Innovative financing and private sector financing could also play a role.
While recovering it is important to build back better TB responses. Learnings from the response to COVID-19 pandemic needs to be incorporated in TB prevention and care as well as in TB research and development, in order to accelerate the fight against TB and make it resilient to the COVID-19 pandemic.
There are several lessons from the COVID-19 pandemic for TB services. New diagnostic tests for COVID-19 were developed and rapidly adopted in national guidelines after regulatory approvals, and these were procured and scaled-up dramatically to over 1 billion COVID-19 tests worldwide in 2020. This was 60 times more than the number of rapid molecular tests for TB performed in a year. This demonstrates how for an extraordinary health crisis national leaderships and ministries of health can prioritize and scale up testing and how the scientific fraternity and private sector industry can collaborate and respond effectively. Rapid molecular testing platforms for TB such as the Xpert MTB/RIF and Truenat have not been applied at large scale in most high TB burden countries (Medecins Sans Frontieres and Stop TB Partnership, 2020). It is time now to scale up TB diagnostics and undertake massive screening and testing for TB.
Contact tracing is an important component of the response to the COVID-19 pandemic, with public health authorities systematically identifying, isolating and monitoring contacts, using community health workers and human resources beyond those available in the health sector. Call centres and mobile phone applications have facilitated contact tracing. In contrast, contact investigation has been a strategy recommended for TB for last several years, but is sub-optimally implemented in most TB programmes. There are several examples of successful TB contact investigation projects implemented (Blok et al., 2015), but scaling such programmes has remained a low priority in the past. It is time now to build systems for better contact investigation in TB.
The COVID-19 pandemic has made people to accelerate the shift to the digital world. Several digital tools such as telemedicine, digital treatment adherence tools and artificial intelligence tools flourished. While building back it is important to use these systems and tools to ensure efficiency and people centred delivery of TB prevention and care. TB screening tools should now include ultraportable digital X-ray with artificial intelligence-based reading which is especially important for screening for asymptomatic TB (Qin et al., 2019). Treatment support should shift to digital adherence tools such as smart pill boxes, medication sleeves and video observed therapy. TB notification systems and laboratory information systems should become real time with publicly available dashboards for monitoring and agility, and TB affected communities need to be empowered with digital tools to monitor TB responses.
TB programmes need to take the opportunity of the prevailing demand and acceptability of masking, social distancing, and airborne infection control measures to rapidly scale these up in health facilities and congregate settings, something that has been planned in the past but not implemented at scale due to low priority. These interventions should now be prioritized, funded and scaled up.
In the area of research and development there are important learnings from the speed with which science and industry responded with new COVID-19 tests and vaccines. Such fast track research and development is needed for TB. More and better tests for TB are needed especially those that can be deployed at the point of care. Tests are needed that can diagnose both TB and COVID-19 from the same specimen. There are currently 14 candidate TB vaccines in different stages of clinical research, but the timeline for their development is in years and decades. Learning from the COVID-19 vaccine research and development, TB needs urgently new science, new approach to fast-track clinical trials and front-loaded investment on candidate vaccines. Financing for research and development needs to be increased and front-loaded.
The World TB Day is observed every year on 24th March and the theme for 2021 is “the clock is ticking” highlighting the urgency to act, to recover, build back better and accelerate further to reach the UNHLM targets set for 2022. For all this to happen high level political commitment at the level of heads of governments is critical. Taking the ten recommendations made in the UN Secretary General's Progress report, we group them into these action themes (Table 1 ).
Table 1.
Ten priority recommendations of the UN Secretary General’s 2020 Progress report on TB for Actions Needed to Accelerate Progress Towards Global TB Targets, reorganized under the headings of recovery and building back better, increased financing and high-level political commitment.
| Recovery and building back better |
|
|
|
|
|
|
| Increased financing |
|
|
| High-level political commitment |
|
|
Transparency declaration
This article is part of a supplement entitled Commemorating World Tuberculosis Day March 24th, 2021: “The Clock is Ticking” published with support from an unrestricted educational grant from QIAGEN Sciences Inc.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
All authors are members of STOP TB PARTNERSHIP and have a specialist interest in all aspects of Global TB control.
Ethical approval
No ethical approval was required.
Acknowledgements
Sir Zumla is co-Principal Investigator of the Pan-African Network on Emerging and Re-Emerging Infections (PANDORA-ID-NET – https://www.pandora-id.net/) funded by the European and Developing Countries Clinical Trials Partnership the EU Horizon 2020 Framework Programme. Sir Zumla is in receipt of a National Institutes of Health Research senior investigator award and is a Mahathir Science Award Laurette.
References
- Alene K.A., Wandi K., Clements A.C.A. Impact of the COVID-19 Pandemic on Tuberculosis Control: An Overview. Trop Med Infect Dis. 2020;5(3):123. doi: 10.3390/tropicalmed5030123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blok L., Sahu S., Creswell J., Alba S., Stevens R., Bakker M. Comparative Meta-Analysis of Tuberculosis Contact Investigation Interventions in Eleven High Burden Countries. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0119822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cilloni L., Fu H., Vesga J.F., Dowdy D., Pretorius C., Ahmedov S., et al. The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine. 2020;28:100603. doi: 10.1016/j.eclinm.2020.100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fei H., Yinyin X., Hui C., Ni W., Xin D., Wei C., et al. The impact of the COVID-19 epidemic on tuberculosis control in China. Lancet Reg Health Western Pacific. 2020;3:100032. doi: 10.1016/j.lanwpc.2020.100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govt. of India, Nikshay . 2020. TB notification system.https://reports.nikshay.in/ [Accessed 28 January 2021] [Google Scholar]
- Keene C., Mohr-Holland E., Cassidy T., Scott V., Nelson A., Furin J., et al. How COVID-19 could benefit tuberculosis and HIV services in South Africa. Lancet Respir Med. 2020;8(9):844–846. doi: 10.1016/S2213-2600(20)30311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M.S., Surendran D., Manu M.S., Rakesh P.S., Balakrishnan S. Mortality of TB-COVID-19 coinfection in India. Int J TB Lung Dis. 2021 doi: 10.5588/ijtld.20.0947. https://theunion.org/sites/default/files/2021-01/Letter%20Rakesh%200947%20FINAL.pdf [Preprint]; Article submitted 26 December 2020 and final version accepted 9 January 2021. Available from. [DOI] [PubMed] [Google Scholar]
- Medecins Sans Frontieres, Stop TB Partnership . 2020. Step Up for TB 2020: Tuberculosis Policies in 37 Countries.http://www.stoptb.org/suft/Step%20Up%20for%20TB%20Report%20Final.pdf [Google Scholar]
- Multiple Partners . 2020. The impact of COVID-19 on the TB epidemic: A community perspective.http://stoptb.org/assets/documents/resources/publications/acsm/Civil%20Society%20Report%20on%20TB%20and%20COVID.pdf [Google Scholar]
- Qin Z.Z., Sander M.S., Rai B., Titahong C.N., Sudrungrot S., Laah S.N., et al. Using artificial intelligence to read chest radiographs for tuberculosis detection: A multi-site evaluation of the diagnostic accuracy of three deep learning systems. Sci Rep. 2019;9(2019):15000. doi: 10.1038/s41598-019-51503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu S., Ditiu D., Lawson L., Ntoumi F., Arakaki D., Zumla A. UN General Assembly tuberculosis targets: are we on track? Lancet. 2020;395(10228):928–930. doi: 10.1016/S0140-6736(20)30565-1. [DOI] [PubMed] [Google Scholar]
- Stop TB Partnership . 2019. The Paradigm Shift: Global Plan to End TB: 2018-2022.http://www.stoptb.org/assets/documents/global/plan/GPR_2018-2022_Digital.pdf [Google Scholar]
- Stop TB Partnership . 2020. The potential impact of the COVID-19 pandemic on tuberculosis in high burden countries: A modelling analysis.http://stoptb.org/assets/documents/covid/TB%20and%20COVID19_Modelling%20Study_5%20May%202020.pdf [Google Scholar]
- Stop TB Partnership Delegations . 2020. A Deadly Divide: TB Commitments vs TB Realities: A Communities Report on Progress Towards the UN Political Declaration on the Fight Against TB and a Call to Action to Close the Gaps in TB Targets.http://www.stoptb.org/assets/documents/communities/The%20Deadly%20Divide_TB%20Commitments%20vs%20TB%20Realities%20FINAL%20HLM%20Report.pdf November. [Google Scholar]
- The Global Fund . 2020. COVID-19 Information Note: “Catch-up” Plans to Mitigate the Impact of COVID-19 on Tuberculosis Services.https://www.theglobalfund.org/media/10232/covid19_tuberculosisservicesimpact_guidancenote_en.pdf October. [Google Scholar]
- The Union . 2020. Mid-term report on impact of COVID-19 on TB and HIV in Africa.https://theunion.org/sites/default/files/2020-10/Mid-term-Report%20COVID-TBHIV_0.pdf October. [Google Scholar]
- Treatment Action Group (TAG) and Stop TB Partnership . 2020. Tuberculosis Research Funding Trends, 2005–2019.https://www.treatmentactiongroup.org/wp-content/uploads/2020/12/tbrd_2020_final_web.pdf [Google Scholar]
- United Nations General Assembly Resolution A/RES/73/3; October 2018. Political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis. https://www.undocs.org/en/A/RES/73/3.
- United Nations General Assembly 75th session September 2020. Progress towards the achievement of global tuberculosis targets and implementation of the political declaration of the high-level meeting of the General Assembly on the fight against tuberculosis: Report of the Secretary-General https://undocs.org/en/A/75/236.
- World Health Organization . 2020. Global Tuberculosis Report.https://apps.who.int/iris/bitstream/handle/10665/336069/9789240013131-eng.pdf [Google Scholar]
- World Health Organization, COVID-19 Dashboard, https://covid19.who.int/ [Accessed 14 February 2021].