Abstract
Background
The coronavirus disease (COVID-19) pandemic has affected healthcare workers (HCWs) in their clinical practice. HCWs were challenged with new guidelines and practices to protect themselves from occupational risks.
Aim
To determine whether hand hygiene behaviour by real-time measurement was related to the dynamic of the epidemic, and the type of patient being cared for in France.
Methods
This study used an automated hand hygiene recording system to measure HCW hand hygiene on entry to and exit from patient rooms throughout the COVID-19 pandemic. The correlation between hand hygiene compliance and COVID-19 epidemiological data was analysed. Analysis of variance was performed to compare compliance rate during the different periods of the epidemic.
Findings
HCW hand hygiene rate on room entry decreased over time; on room exit, it increased by 13.73% during the first wave of COVID-19, decreased by 9.87% during the post-lockdown period, then rebounded by 2.82% during the second wave of the epidemic. Hand hygiene during patient care and hand hygiene on room exit had a positive relationship with the local COVID-19 epidemic; conversely, hand hygiene on room entry did not depend on the trend of the epidemic, nor on nursing of COVID-19 patients, and it decreased over time.
Conclusion
HCWs modified their behaviours to face the risk propensity of the pandemic. However, to improve the poor compliance at room entry, reducing confusion between the hand hygiene recommendation and glove recommendation may be necessary; disinfection of gloving hands might solve this issue.
Keywords: COVID-19, Real-time measurement, Compliance, Automated hand-hygiene monitoring, Cross-transmission, Infection control
Introduction
Since the 2000s, coronaviruses (CoVs) have been associated with significant disease outbreaks in East Asia (SARS-CoV-1) and the Middle East (MERS-CoV). The spread of the novel coronavirus (SARS-CoV-2), initially identified in the Hubei province of China in December 2019 was declared by the World Health Organization (WHO) as the pandemic of coronavirus disease (COVID-19) in March 2020 [1]. At the time of writing there had been 91,938,218 cases and 1,967,655 deaths globally, including 2,806,590 cases and 68,802 deaths in France [2]. Healthcare workers (HCWs) worldwide – who have been regularly trained to avoid hospital-acquired infection by following guidelines, particularly hand hygiene – are currently facing another objective in order to reduce cross-transmission and protect their patients: to protect themselves from SARS-CoV-2 infection using prevention protocols to which they are less commonly accustomed (self-protection) [3]. These new sanitary guidelines directed toward HCW protection rather than toward patient protection constitute a new challenge for this community. With personal protective equipment (PPE), hand hygiene has been shown to be the cornerstone of protection from respiratory viruses, and hand hygiene remains a major way to limit cross-transmission, as recommended by WHO [4,5].
Since 2012, we have developed an automated hand hygiene monitoring system and used it as a part of the management of healthcare-associated infections at the Institut Hospitalo-Universitaire Méditerranée Infection (IHU-MI) [[6], [7], [8], [9]]. The changing paradigm of hand hygiene practice imposed by this new ongoing epidemic seemed interesting to monitor with our system, to evaluate whether HCWs had easily adjusted to this new approach of infection prevention and changed their behaviour. Since two epidemic waves have been observed, the intention was to monitor HCWs in between the two waves to determine whether their hand hygiene behaviour correlated with the outbreak amplitude and with the type of patient being cared for.
This study aimed to observe whether hand hygiene practices on entry and exit of the patient's room and during patient care were correlated with the dynamic of the epidemic, and with the type of patient being cared for (COVID-19 cases or not) throughout the two waves of the COVID-19 pandemic.
Methods
Automated hand hygiene recording systems
Since the end of 2017, an automatic hand hygiene monitoring device (MediHandTrace®) has been in place in the infectious diseases unit, which contains 25 single bedrooms. This system measures HCW utilization of alcohol-based hand rub (AHR) on entry and exit from patient rooms (hand hygiene opportunity). Thanks to voluntary HCWs who gave their consent, a unique ID tag is inserted in their shoes, and, when entering or exiting the bedroom of each patient's room, this ID tag, a door sensor, and a sensor on the hand sanitizer communicate through a server and allow identification of who entered or exited the room, and whether AHR was performed on entry and exit, with a very good accuracy in experimental settings [[7], [8], [9], [10]]. However, in the real-life environment, the system does not tend to perform as well, especially when several HCWs enter the room at the same time. Indeed, sensor events such as ‘the door is opening’ and ‘the door is closing’ are not associated with an ID tag, and therefore cannot be directly linked to an individual HCW, leaving issues such as whether or not the person whose behaviour is being evaluated truly exited the room.
To optimize the accuracy of interpretation of HCW activities, an algorithm was developed, written in C++ programming language, that identified each activity by analysis of short sequences of consecutive events from raw sensor data. Sensor events were grouped in sequences defined as a serial of signals traducing an event (the door is opening, an identified HCW puts his/her shoes on the carpet, he/she uses hydroalcoholic solution, etc.) associated with its corresponding time of occurrence.
Such event grouping enabled us to accurately pair entry and exit events with unique ID tags in the single bedroom/multiple HCW scenario. It was thus possible to follow the nursing staff's activities in a bedroom on an individual basis – for instance, for each HCW – to determine whether they washed their hands when they entered and when they left the room. To assess the accuracy of the optimization algorithm, we compared its interpretation to a human-based video analysis from cameras set up in patients' rooms. Level of correspondence was excellent.
Piloting of the automated system
In order to assess accuracy of data capture, we examined 33 randomly selected HCW events occurring between November 26th and 29th, 2019 and compared video and interpretations from the algorithm. Eighteen room entries were correctly interpreted as such by the algorithm; for room exits, 13 were interpreted correctly but two interpretations were erroneous due to several HCWs exiting at the same time. Therefore 93.9% of entries and exits were interpreted correctly by the algorithm and the kappa coefficient between the videos and interpretations from the algorithm was 0.88 (Supplementary Appendix).
Infection control procedures
During the COVID-19 pandemic, HCWs were trained and encouraged to adhere to the principles of WHO evidence-based guidelines for PPE use and hand hygiene practice [11,12]. HCWs were asked to wear PPE (gown, FFP2 mask, and gloves) before entering patient rooms. Hand sanitizers containing alcohol (75–85% v/v) effectively reduce the infectivity of corona-viruses in vitro [13]. Disinfection of gloved hands has been demonstrated as efficient and feasible during patient care for multiple activities, and a recent study shows that alcohol-based solution did not affect elongation at breakage of the nitrile gloves [[14], [15], [16]]. Thus, we promoted the use of gloved AHR upon entry to the room, upon exit of the room, and as often as necessary during patient care.
Definitions
Daily hand hygiene compliance rate on room entry and exit was computed by the daily number of AHR utilizations on entry and exit, divided by the total daily number of entries and exits. AHRs during care were computed by the number of AHRs recorded by our system after 18 s (grace delay period) from entering divided by the total daily number of room entries. AHR consumption was computed by the total volume (one application of AHR: 3 mL) of AHR by each HCW each day.
The epidemiological COVID-19 data of our hospital was based on the monthly number of patients screened and the number of patients diagnosed positive for SARS-CoV-2, obtained from the hospital information system. To calculate nursing care of the COVID-19 patient, the bed-day total was calculated as the daily number of beds occupied by either a COVID-19 or a non-COVID-19 patient admitted as an inpatient each month. The study was then separated into four periods: (i) pre-COVID-19, from September 2019 to the end of February 2020; (ii) the first wave of COVID-19, from March 2020 to the end of May 2020; (iii) post lockdown, from June 2020 to the end of August; (iv) the second wave of COVID-19, from September 2020 to the end of November 2020.
Statistical analysis
Data analysis included descriptive analyses. The assumption of normality was assessed by analysis of skewness and kurtosis. First, to evaluate the association between the local COVID-19 epidemic and hand hygiene behaviours, the Pearson correlation coefficient was calculated for the compliance with AHR (on entry and exit), the number of patients screened, the number of patients diagnosed as positive for SARS-CoV-2, and the total bed-days of care of each COVID-19 patient. Second, comparing any differences in compliance with AHR between the four COVID-19 periods, analysis of variance was used to compare the mean of compliance with AHR (on entry, during care and on exit) and AHR consumption between these periods. Time-series analysis using the autoregressive integrated moving average model was performed to analyse the trend of hand hygiene compliance over time. P < 0.05 was considered statistically significant. All the collected data were entered into an Excel file and the statistical tests were performed with SPSS 25.
Ethics
The study protocol was approved by the Review Board of our institution and available under No. 2016–018; all participating HCWs were informed about the automatic monitoring procedure and the guarantee of anonymity and confidentiality. Video was recorded and visualized for accuracy evaluation of the algorithm by two researchers not involved in patient care (M.A. and F.H.). When the content had been analysed and anonymized, the recording video was destroyed. All HCWs are protected by the French National Commission on Informatics and Liberty.
Results
Evolution of compliance with hand hygiene
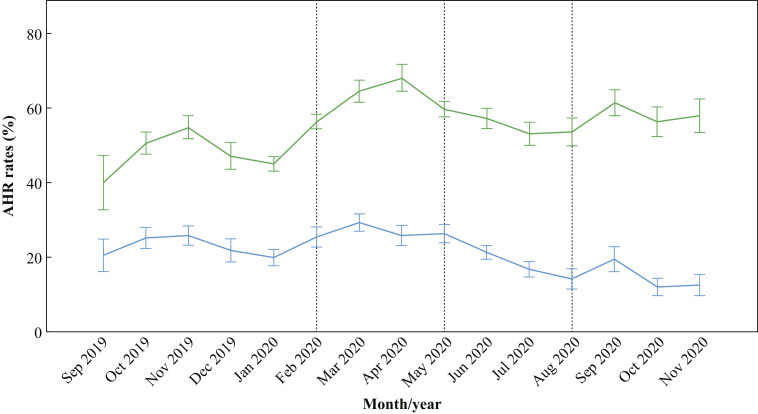
From September 2019 to November 2020 (over 15 months of real-time observation), a total of 162,334 entries and exits were recorded by the automatic monitoring system. The mean of compliance with AHR use on entry to a patient's room within this period of observation was 21.02% (SD: 8.91) and on exit from a patient's room was 55.03% (SD: 11.9). During care, mean incidence of AHR use by HCWs was 4.32% (SD: 2.34). Mean AHR consumption was 61.63 (SD: 22.45) mL/HCW/day. Figure 1 shows the evolution of compliance with AHR use on room entry, during patient care and on room exit.
Figure 1.
Evolution of the compliance to alcohol-based hand rub (AHR) use on room entry, during patient care, and on room exit; 95% confidence interval. Green line: AHR rates of use on room exit; blue line: AHR rates of use on room entry; vertical dashed lines: different periods of the epidemic.
Epidemiological data
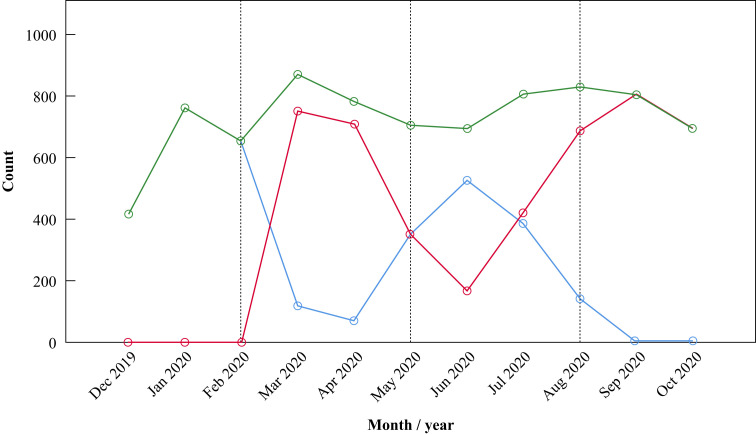
From December 2019 to November 2020, a total of 253,547 new patients were screened at IHU-MI and 21,938 patients were diagnosed as SARS-CoV-2 positive. A total of 1319 patients were admitted to the unit including 834 COVID-19 patients. Each month, the average number of patients screened was 16,903 (SD: 18654) and the average number of COVID-19 patients was 1466 (SD: 2058) (Supplementary Appendix). The average number of bed-days was 730 (SD:123) per month, including 313 (SD: 265) bed-days for non-COVID-19 patients and 417 (SD: 330) bed-days for COVID-19 patients (Figure 2 ).
Figure 2.
Evolution of bed-days of care. Green line: total number of bed-days of care; red line: bed-days of care of COVID-19 patients; blue line: bed-days of care of non-COVID-19 patients; vertical dashed lines: different periods of the epidemic.
Compliance with AHR use on room exit had a positive correlation with the number of patients screened (r = 0.66, P = 0.004), the number of patients diagnosed (r = 0.53, P = 0.021), and the total number of bed-days of COVID-19 patients (r = 0.68, P = 0.011). Use of AHR during care had a strong positive correlation with the number of patients screened (r = 0.84, P < 0.001), the number of patients diagnosed (r = 0.77, P < 0.001), the number of bed-days of COVID-19 patients (r = 0.88, P < 0.001), and the moderately positive correlation with total number of bed-days of care (r = 0.57, P = 0.033). AHR consumption had a positive correlation with the number of bed-days of COVID-19 patients (r = 0.63, P = 0.019) and total bed-days of care (r = 0.61, P = 0.023). Compliance with AHR use on room exit and AHR use during patient care increased as the epidemic of COVID-19 increased or the nursing of COVID-19 in the unit increased, and vice versa. AHR consumption increased when the total number of bed-days or the nursing of COVID-19 patients increased. However, compliance with AHR use on room entry was not associated with the COVID-19 epidemic or the nursing of COVID-19 in the unit (Table I ).
Table I.
Correlations between monthly data for alcohol-based hand rub (AHR) use and patient variables
| Variable | Statistic | AHR on entry | AHR on exit | AHR during care | AHR consumption | Patients screened | Patients diagnosed | COVID patients |
|---|---|---|---|---|---|---|---|---|
| AHR on exit | Pearson r | 0.211 | 1 | |||||
| P | 0.226 | |||||||
| N | 15 | 15 | ||||||
| AHR during care | Pearson r | –0.307 | 0.782 | 1 | ||||
| P | 0.133 | 0.000 | ||||||
| N | 15 | 15 | 15 | |||||
| AHR consumption | Pearson r | 0.203 | 0.561 | 0.298 | 1 | |||
| P | 0.234 | 0.015 | 0.140 | |||||
| N | 15 | 15 | 15 | 15 | ||||
| Patients screened | Pearson r | –0.310 | 0.656 | 0.842 | 0.290 | 1 | ||
| P | 0.131 | 0.004 | 0.000 | 0.147 | ||||
| N | 15 | 15 | 15 | 15 | 15 | |||
| Patients diagnosed | Pearson r | –0.360 | 0.529 | 0.769 | 0.329 | 0.915 | 1 | |
| P | 0.093 | 0.021 | 0.000 | 0.116 | 0.000 | |||
| N | 15 | 15 | 15 | 15 | 15 | 15 | ||
| COVID patients | Pearson r | –0.165 | 0.676 | 0.882 | 0.628 | 0.932 | 0.848 | 1 |
| P | 0.314 | 0.011 | 0.000 | 0.019 | 0.000 | 0.000 | ||
| N | 11 | 11 | 11 | 11 | 11 | 11 | 11 | |
| Bed-days of care | Pearson r | –0.022 | 0.465 | 0.573 | 0.612 | 0.493 | 0.393 | 0.659 |
| P | 0.475 | 0.075 | 0.033 | 0.023 | 0.062 | 0.116 | 0.014 | |
| N | 11 | 11 | 11 | 11 | 11 | 11 | 11 |
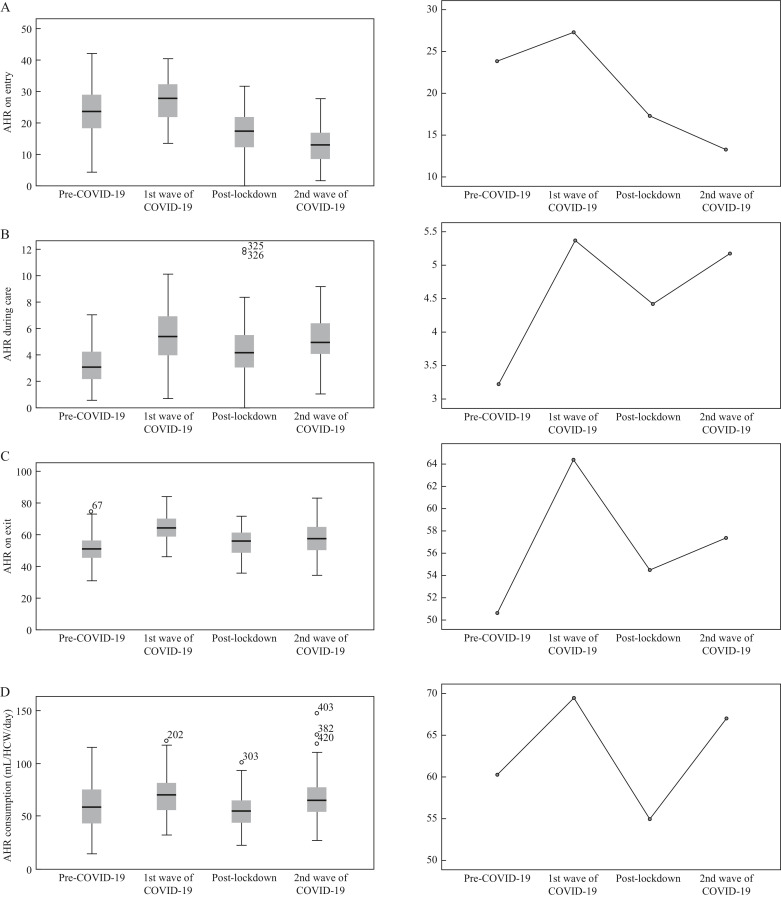
The mean of compliance with AHR use on room entry was 23.88% (SD: 7.56) during the pre-COVID-19 period. For the first wave of COVID-19 this was 27.31% (SD: 6.45), for the post-lockdown period 17.3% (SD: 6.77), and for the second wave was 13.3% (SD: 6.27) (F(3,435) = 77.93, P < 0.001). This low compliance rate on room entry could be explained by the fact that HCWs were gloved before entering the room and staff were not used to disinfecting gloved hands. The mean rate of AHR use during patient care was 3.21% (SD: 1.43) at the pre-COVID-19 period; for the first wave of COVID-19 this was 5.37% (SD: 2.11), for the post-lockdown period 4.41% (SD: 2.15), and for the second wave 5.17% (SD: 1.83) (F(3, 435) = 37.36, P < 0.001). The mean of compliance with AHR use on room exit was 50.63% (SD: 8.28) for the pre-COVID-19 period; for the first wave of COVID-19 this was 64.37% (SD: 8.27), for the post-lockdown period 54.5% (SD: 8.52), and for the second wave 57.32% (SD: 9.93) (F(3, 435) = 51.57, P < 0.001). Mean AHR consumption was 60.28 (SD: 22.75) mL/HCW/day for the pre-COVID-19 period; for the first wave of COVID-19 this was 69.42 (SD: 18.74) mL/HCW/day, for the post-lockdown period 54.94 (SD: 15.97) mL/HCW/day, and for the second wave was 66.98 (SD: 21.83) mL/HCW/day (F(3, 435) = 9.578, P < 0.001) (Figure 3 ).
Figure 3.
Box plots and mean plots. (A) Alcohol-based hand rub (AHR) use on room entry (%); (B) AHR use during patient care (%); (C) AHR use on room exit (%); (D) AHR consumption (mL/HCW/day) during four periods of the COVID-19 epidemic. HCW, healthcare worker.
Mean rate of AHR use on room entry increased by 3.43% during the first wave of COVID-19 but became lower over time. Mean rate of AHR use during patient care increased by 2.15% during the first wave of COVID-19, decreased by 0.95% during the post-lockdown period, and then rebounded by 0.76% during the second wave of the epidemic. Mean rate of AHR use on room exit increased by 13.73% during the first wave of COVID-19, decreased by 9.87% during the post-lockdown period, then rebounded by 2.82% during the second wave of the epidemic. AHR consumption increased by 9.14 mL/HCW/day during the first wave of COVID-19, decreased by 14.48 mL/HCW/day post lockdown, and then rebounded by 12.05 mL/HCW/day during the second wave of the epidemic. Time-series analysis confirmed that there was a decrease in compliance with AHR use on room entry over time (P < 0.001) and an increase in compliance with AHR use on room exit over time (P = 0.013).
Discussion
This long-term hand-hygiene observation using data from an automated monitoring system shows that HCW use of AHR during patient care and on room exit were positively correlated with the dynamics of the local COVID-19 epidemic and the nursing of COVID-19 patients. Total AHR consumption appeared to be related to the nursing of COVID-19 patients and the total number of bed-days of care. Conversely, AHR use on room entry did not depend on the trend of the epidemic nor on the nursing of COVID-19 patients. Consequently, rates of AHR use on room entry and on room exit increased during the first wave of the epidemic and decreased during the post-lockdown period, while AHR use on room exit and during care tended to follow the trend of the epidemic; AHR use on room entry decreased over time.
Four recent studies found that HCW hand hygiene compliance improved during the early pandemic (first quarter of 2020); however, three of these studies were observed by audit without comparing with any remarkable events in national COVID-19 control [[17], [18], [19], [20]]. One study that was based on an automated monitoring system obtained a result similar to ours. The authors found decreased hand hygiene performance after school closures, and concluded that even during the global crisis it seemed difficult to maintain improved hand hygiene performance [20].
Automated monitoring does afford some advantages during the pandemic, such as reducing the human cost for audit, continued measurement and reducing the Hawthorne effect [21]. Our finding shows the different evolution of four hand hygiene indicators: compliance with AHR use on room entry, AHR use during patient care, AHR use on room exit and total AHR consumption. AHR use on room entry and during patient care are mainly related to patient protection whereas AHR use on room exit is related to self-protection of HCWs. At the beginning of the epidemic, the improvement of self-protection and of patient-protection measures could be explained by HCW fear of the crisis, to avoid transmitting the virus to their family, to themselves or to their patients. A recent psychology study showed that fear of pandemic encouraged recommended public health behaviours due to the negative emotions that reduce motivation for risky behaviours [22]. It could also be explained by reference to the protocol. Among all required PPE within the COVID-19 protocol, our observations show a correlation between AHR use and the hospitalization of COVID-19 patients in the unit, with hand hygiene being performed frequently as recommended by WHO [23].
The second observation was the different evolution of compliance with AHR use at room entry and room exit. It seems that the COVID-19 outbreak had more impact on compliance with AHR use on room exit and during care, and on total AHR consumption. HCWs were asked to wear PPE before entering a patient's room and then to remove gloves and apply AHR before leaving a patient's room; this protocol was respected. Thus, even with the fall in compliance during the post-lockdown period, the AHR use on room exit and during patient care remained higher during the second wave of the epidemic than during the pre-COVID-19 period.
Under those circumstances, it seems that gloving hands causes the reduction of compliance at entry. After the first wave of the epidemic, HCWs disinfected their hands less and less on room entry. The low compliance rates on entry could be explained by the gloved hands, which have been reported to reduce hand hygiene rates [24]. Moreover, one may imagine that HCWs better perceived the risk of being exposed to the virus themselves rather than the risk to the patients. However, several recent studies showed the benefit of disinfection of gloved hands [[25], [26], [27]]; alcohol-based disinfectants may slightly affect the breaking load of nitrile gloves, but it does not affect its extensibility [15]. It seems that our HCWs were not aware of such evidence on room entry. As noticed by Allegranzi et al., hand hygiene appears neglected when the emergent virus seems to disappear with compliance rates becoming lower, which ties in with our observations. The studies of Maltezou et al. show that there are gaps in infection control in non-COVID-19 referral hospitals; it is possible that adherence to recommendations could be even lower in non-COVID-19 hospitals [28].
In conclusion, HCWs respected the protocol and modified their behaviours during the outbreak; however, improvements in compliance with AHR on room entry and on exit were not sustained throughout the epidemic, especially for entry. This pandemic has led HCWs to adapt their hand hygiene behaviour to the visible risk (the epidemic's curve) to protect themselves; according to our findings, we emphasize the importance of hand hygiene monitoring even during the pandemic, especially before patient contact. To reduce potential confusion between the hand hygiene recommendation and the glove recommendation, disinfection of gloving hands might improve poor compliance at entry.
Acknowledgements
We thank the nurses and all the medical team at the Institut Hospitalo-Universitaire Méditerranée Infection for their willingness to participate and cooperate in this research. We thank D. Braustein for the epidemiological data. We thank Dr A. McGonigal for English language editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhin.2021.03.004.
Conflict of interest statement
P. Brouqui was a former advisor of the MediHandTrace Company.
Funding sources
This study was funded by ANR-15-CE36-0004-01 and by ANR ‘Investissements d’avenir’, Méditerranée Infection 10-IAHU-03, and in part by SHARP-JA, Grant Agreement EC no. 848096.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO. Weekly epidemiological update on COVID-19 – 16 March 2021. n.d. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20210316_Weekly_Epi_Update_31.pdf [last accessed March 2021].
- 2.Coronavirus Update (Live): 124,338,690 Cases and 2,736,721 Deaths from COVID-19 Virus Pandemic – Worldometer n.d. https://www.worldometers.info/coronavirus/ [last accessed March 2021].
- 3.Lotfinejad N., Peters A., Pittet D. Hand hygiene and the novel coronavirus pandemic: the role of healthcare workers. J Hosp Infect. 2020;105:776–777. doi: 10.1016/j.jhin.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hirose R., Ikegaya H., Naito Y., Watanabe N., Yoshida T., Bandou R. Survival of SARS-CoV-2 and influenza virus on the human skin: importance of hand hygiene in COVID-19. Clin Infect Dis. 2020 Oct 3 doi: 10.1093/cid/ciaa1517. ciaa1517 [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. n.d. Available at: https://www.who.int/publications/i/item/10665-331495 [last accessed March 2021].
- 6.Brouqui P., Boudjema S., Soto Aladro A., Chabrière E., Florea O., Nguyen H. New approaches to prevent healthcare-associated infection. Clin Infect Dis. 2017;65:S50–S54. doi: 10.1093/cid/cix433. [DOI] [PubMed] [Google Scholar]
- 7.Dufour J.-C., Reynier P., Boudjema S., Soto Aladro A., Giorgi R., Brouqui P. Evaluation of hand hygiene compliance and associated factors with a radio-frequency-identification-based real-time continuous automated monitoring system. J Hosp Infect. 2017;95:344–351. doi: 10.1016/j.jhin.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Kerbaj J., Toure Y., Soto Aladro A., Boudjema S., Giorgi R., Dufour J.C. Smartphone text message service to foster hand hygiene compliance in health care workers. Am J Infect Control. 2017;45:234–239. doi: 10.1016/j.ajic.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 9.Boudjema S., Dufour J.C., Aladro A.S., Desquerres I., Brouqui P. MediHandTrace®: a tool for measuring and understanding hand hygiene adherence. Clin Microbiol Infect. 2014;20:22–28. doi: 10.1111/1469-0691.12471. [DOI] [PubMed] [Google Scholar]
- 10.Charles Dufour J. Input of innovative technology for surveillance and improvement of hand hygiene: the MediHandTrace contribution to hand disinfection monitoring and intervention. Clin Microbiol Open Access. 2015;4 doi: 10.4172/2327-5073.1000216. [DOI] [Google Scholar]
- 11.World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. n.d. https://apps.who.int/iris/bitstream/handle/10665/338033/WHO-2019-nCoV-IPC_PPE_use-2020.4-eng.pdf [last accessed March 2021].
- 12.World Health Organization . WHO; Geneva: 2009. WHO guidelines on hand hygiene in health care. [DOI] [PubMed] [Google Scholar]
- 13.Kratzel A., Todt D., V’kovski P., Steiner S., Gultom M., Thao T.T.N. Inactivation of severe acute respiratory syndrome coronavirus 2 by WHO-recommended hand rub formulations and alcohols. Emerg Infect Dis. 2020;26:1592–1595. doi: 10.3201/eid2607.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kampf G., Lemmen S. Disinfection of gloved hands for multiple activities with indicated glove use on the same patient. J Hosp Infect. 2017;97:3–10. doi: 10.1016/j.jhin.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 15.Garrido-Molina J.M., Márquez-Hernández V.V., Alcayde-García A., Ferreras-Morales C.A., García-Viola A., Aguilera-Manrique G. Disinfection of gloved hands during the COVID-19 pandemic. J Hosp Infect. 2021;107:5–11. doi: 10.1016/j.jhin.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assadian O., Humphreys P.N., Ousey K.J. Disinfection of artificially contaminated gloved hands reduces transmission of Staphylococcus epidermidis to catheter valves. J Hosp Infect. 2018;100:e57–e59. doi: 10.1016/j.jhin.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Israel S., Harpaz K., Radvogin E., Schwartz C., Gross I., Mazeh H. Dramatically improved hand hygiene performance rates at time of coronavirus pandemic. Clin Microbiol Infect. 2020;26:1566–1568. doi: 10.1016/j.cmi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Derksen C., Keller F.M., Lippke S. Obstetric healthcare workers’ adherence to hand hygiene recommendations during the COVID-19 pandemic: observations and social-cognitive determinants. Appl Psychol Health Well-Being. 2020 doi: 10.1111/aphw.12240. aphw.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong S.-C., AuYeung C.H.-Y., Lam G.K.-M., Leung E.Y.-L., Chan V.W.-M., Yuen K.-Y. Is it possible to achieve 100 percent hand hygiene compliance during the coronavirus disease 2019 (COVID-19) pandemic? J Hosp Infect. 2020;105:779–781. doi: 10.1016/j.jhin.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore L.D., Robbins G., Quinn J., Arbogast J.W. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am J Infect Control. 2021;49:30–33. doi: 10.1016/j.ajic.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagel S., Reischke J., Kesselmeier M., Winning J., Gastmeier P., Brunkhorst F.M. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol. 2015;36(8):957–962. doi: 10.1017/ice.2015.93. [DOI] [PubMed] [Google Scholar]
- 22.Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020:1–14. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cavanagh G., Wambier C.G. Rational hand hygiene during the coronavirus 2019 (COVID-19) pandemic. J Am Acad Dermatol. 2020;82:e211. doi: 10.1016/j.jaad.2020.03.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fuller C., Savage J., Besser S., Hayward A., Cookson B., Cooper B. “The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32:1194–1199. doi: 10.1086/662619. [DOI] [PubMed] [Google Scholar]
- 25.Baloh J., Thom K.A., Perencevich E., Rock C., Robinson G., Ward M. Hand hygiene before donning nonsterile gloves: healthcare workers’ beliefs and practices. Am J Infect Control. 2019;47:492–497. doi: 10.1016/j.ajic.2018.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jain S., Clezy K., McLaws M.-L. Modified glove use for contact precautions: health care workers’ perceptions and acceptance. Am J Infect Control. 2019;47:938–944. doi: 10.1016/j.ajic.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Acquarulo B.A., Sullivan L., Gentile A.L., Boyce J.M., Martinello R.A. Mixed-methods analysis of glove use as a barrier to hand hygiene. Infect Control Hosp Epidemiol. 2019;40:103–105. doi: 10.1017/ice.2018.293. [DOI] [PubMed] [Google Scholar]
- 28.Maltezou H.C., Dedoukou X., Tsonou P., Tseroni M., Raftopoulos V., Pavli A. Hospital factors associated with SARS-CoV-2 infection among healthcare personnel in Greece. J Hosp Infect. 2021;109:40–43. doi: 10.1016/j.jhin.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.