Abstract
Compression therapy is the mainstay of treatment for patients with venous leg ulcers. Current gold standard is 4 layer bandaging, which has a significant impact on patients comfort, ability to wear their own shoes, and quality of life, as well as taking significant time to apply, and losing compression over time. This systematic review aims to evaluate the use of Velcro wrap devices for the treatment of venous ulceration. Preferred reporting items for systematic reviews and meta‐analyses (PRISMA) guidelines were used to identify articles reporting the use of Velcro wrap devices in patients with venous ulceration. Sixteen articles were identified (14 case series, 1 randomised trial, and 1 audit) reporting on 192 patients. There were reports of improved time to healing, reduced cost by >50%, reduced number and duration of nursing appointments, and improved quality of life in patients in Velcro wrap devices. Although the evidence remains poor, Velcro devices have potential to improve outcomes for patients with venous ulceration and further good quality studies should be undertaken to evaluate these further.
Keywords: compression, venous ulcer, velcro wrap, juxtacures
Key Messages.
this systematic review highlights the use of Velcro Wrap devices for venous ulceration, giving an overview of the different devices available
velcro devices have the potential to reduce cost, reduce nursing time and appointments, and improve ulcer healing
1. INTRODUCTION
Chronic venous ulceration affects approximately 0.6% of the adult population (278 000 persons in the UK),1 is more common in the elderly, and is often associated with a prolonged period of healing and a high recurrence rate.2 As such, venous ulceration significantly affects patient quality of life, and represents a major drain on NHS and social services resources, totalling approximately £662 million per year.3 First line treatment for the management of uncomplicated venous ulceration in the UK is multilayered compression bandaging.4 This serves to increase venous return and reduce venous hypertension, as well as reduce oedema and improve lymphatic circulation, which is often poor in patient with venous leg ulcers.5 There is a wide variety of compression bandaging techniques, with several trials comparing these. The VenUS I trial identified 4 layer bandaging to be more clinically effective and cost effective than short‐stretch bandaging.6 The VenUS IV trial7 found no difference between 4 layer bandaging and two layer hosiery. There is evidence that compression reduces pain, increases healing rates, and improves both quality of life and functional status, when compared with using simple wound dressings alone.8, 9 However, all of these techniques have a significant impact on patient lifestyle, and nursing time.
Despite evidence regarding the benefits of superficial venous surgery in patients with venous leg ulcers,10, 11 this therapy is used in addition to compression, therefore, optimising compression treatment is the primary aim to heal ulcers.
Despite its importance and widespread use, it has been predicted that up to 51% of patients do not comply with their multilayered bandaging.12 There are many potential reasons for this, including: skin irritation, bandage slippage, pain, malodour, inability to maintain hygiene, and discomfort and inability to wear normal footwear. It is also thought that the effect of the compression is compromised by differing leg shapes and skin consistencies.13
Over recent years, there has been development of several Velcro‐based wrap devices for use as alternative compression bandaging for venous ulcer management, using either interlacing or overlapping techniques of wrapping. These can consist of various components to cover the foot up to the thigh. The key differences are outlined in Table 1. Prior descriptive systematic reviews have been undertaken for Velcro wrap devices, including their use in chronic oedema, lipoedema, and lymphoedema, as well as venous ulceration.14, 15 These studies identified a reduction in limb volume and more consistent sub‐bandage pressure in Velcro wrap devices compared with bandaging. In addition, one of the major advantages identified was the relative ease to remove and reapply these devices, which can, therefore, encourage self‐care, improve independence and potentially quality of life.
Table 1.
Details of available Velcro wrap devices for venous ulceration
| Company | Device | Components | Posterior spine | Pressure measuring aid | Technique |
|---|---|---|---|---|---|
| L&R Medical UK | Readywrap | Foot | Yes | No | Overlapping |
| Calf | |||||
| Knee | |||||
| Thigh | |||||
| MediUK | JuxtaCURES | Anklet | No | Yes | Interlacing |
| Calf | |||||
| Sigvaris | Compreflex | Boot | No | No | Interlacing |
| Calf | |||||
| Knee | |||||
| Comprefit | Yes | ||||
| JOBST | FarrowWrap 4000 | Foot | Yes | No | Interlacing |
| Calf | |||||
| Thigh | |||||
| FarrowWrap Strong | Overlapping | ||||
| FarrowWrap Basic | Overlapping | ||||
| FarrowWrap Classic | Overlapping | ||||
| Juzo | Compression wrap | Foot | No | No | Interlacing |
| Calf | |||||
| Haddenham | EasyWrap | Foot | Yes | No | Overlapping |
| Calf |
Posterior spine—stiffer area at back of the device to provide additional compression to calf, ensure alignment and provide vertical stability.
Interlacing technique—each layer of the bandage applied in the opposite direction.
Overlapping technique—all layers of the bandage applied in the same direction with 50% overlap.
The aim of this study is to review the current literature on Velcro‐based wrap devices for venous ulcer healing, cost, nursing time, and patient satisfaction.
2. METHODS
Standard reporting guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA)16 were used to identify any studies reporting on outcomes for all of the devices. Study titles and abstracts were searched using Medline, Embase, Scopus, CINAHL, Pubmed, and Web of Science in September 2018 and repeated in November 2018 by PS and AH. The search terms (Juzo compression) OR (Juxta Cures) OR (readywrap OR juxtacures OR circaid OR comprefit OR compreflex OR farrowwrap) OR ((wrap[MESH] OR device[Mesh[OR dressing[Mesh] or bandage[Mesh]) AND (Velcro Leg OR hook and loop)) AND ulcer[Mesh] were used. No language restrictions or filters were used to restrict study design. Reference lists were searched for further studies to be included (Figure 1).
Figure 1.
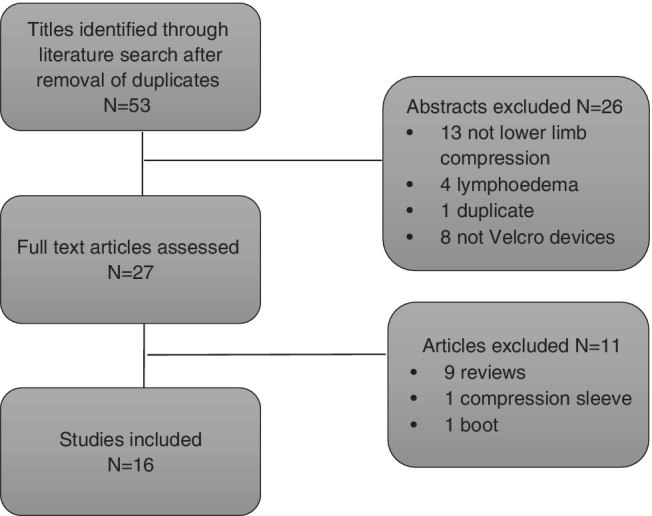
PRISMA diagram
2.1. Study selection and data extraction
Potential studies were screened by PS and AH. For inclusion within the systematic review, the study had to report outcomes for patients using any type of Velcro elastic compression for the treatment of venous ulceration. The outcomes included within this review were ulcer healing, patient satisfaction, cost, and nursing time. All article types were included and although randomised controlled trials were included, randomisation and the use of a comparator were not required. Studies reporting on lymphoedema were excluded.
Data were extracted independently to include the number of participants within the study, type of device used, and outcomes of interest, with any discrepancies discussed between PS and AH. Data included patient satisfaction, cost, nursing time, and ulcer healing.
Study quality was assessed using the Joanna Briggs Institute critical appraisal tool checklists as appropriate.
3. RESULTS
The literature search identified 77 articles. After removal of duplicates, 53 titles and abstracts were reviewed. A total of 26 articles were removed following abstract review, 13 not looking at lower limb compression, 4 regarding lymphoedema, 1 meeting report duplicating another publication, and 8 did not examine Velcro devices. Full text review was undertaken for 27 articles, with a further 11 removed (9 review articles, 1 using a compression sleeve, and 1 using a boot). This resulted in 16 articles to include within the systematic review. For a description of study quality, see Supplemental File.
3.1. Study characteristics
There was one trial comparing both bandaging and JuxtaCures in patients with bilateral ulcers with each limb randomised,17 1 audit,18 and 14 case series19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 ranging from 1 to 35 patients, with 192 patients reported in total. Thirteen studies used the JuxtaCures (or the JuxtaLite or JuxtaFit), 1 study used the JOBST FarrowWrap Strong and Lite,31 1 study used ReadyWrap,18 and 1 study used multiple devices (232) (See Table 2).
Table 2.
Details of studies reporting on Velcro wrap devices for venous ulceration
| Author, year, journal | Type of article | Compression system | Participants | Duration of study | Outcome measures | ||||
|---|---|---|---|---|---|---|---|---|---|
| Healing | Cost | Nursing time | Number of visits | Quality of life | |||||
| Blecken, 2005, J Vasc Surg | Randomised trial | 4 layer bandage v CircAid a | 12 with bilateral ulcers, single leg in each study arm | 12 wk | ✓ | ✓ | |||
| Bradley, 2017, Journal of Community Nursing | Case series | JuxtaCures | 10 patients with previous history of >5 mo compression bandaging | 12 wk | ✓ | ✓ | ✓ | ✓ | |
| Mahoney, 2016, Journal of Community Nursing | Case series | JuxtaLite | 3 patients with recurrent ulcers | ✓ | |||||
| Wicks, 2015, Wound Care | Case series | JuxtaCures and JuxtaFit | 16 patients previously in bandaging | ✓ | ✓ | ✓ | |||
| Brizzio, 2006, Phlebologie | Case series | Stockings (15‐20, 20‐30 or 30‐40 mm Hg), multilayered bandages or CircAid a | 35 patients with no history | ✓ | |||||
| Elvin, 2015, Journal of Community Nursing | Case series | JuxtaCures | 26 patients | 6 mo pre and post change | ✓ | ✓ | ✓ | ||
| Nugent, 2013, Wound Care | Case study | JuxtaCures | 1 patient | 10 wk | ✓ | ✓ | ✓ | ||
| Todhunter, 2017, Journal of Community Nursing | Case series | JOBST FarrowWrap Strong and Lite | 2 patients | ✓ | ✓ | ||||
| Freeman, 2015, Wounds UK | Case series | JuxtaCures | 2 patients in prior bandaging | 3 mo assessment pre and post change | ✓ | ✓ | ✓ | ||
| Ehmann, 2016, Journal of Wound Care | Audit | ReadyWrap | 17 patients in 3 UK and 1 US centre | ✓ | |||||
| Ehmann, 2018, Journal of Wound Care | Case series | A variety of Velcro devices | 9 patients | ✓ | |||||
| Lawrence, 2014, Wounds UK | Case series | JuxtaCures | 3 patients | ✓ | |||||
| Kline, 2008, Vascular | Cohort study | Elastic stocking v Circaid | 30 patients | ✓ | |||||
| Dowsett, 2013, Wounds UK | Case series | JuxtaCures | 2 patients | ✓ | ✓ | ||||
| Williams, 2017, Journal of Community Nursing | Case series | JuxtaCures | 15 patients previously in bandaging | ✓ | ✓ | ✓ | |||
| Freeman, 2016, Journal of Community Nursing | Case series | JuxtaCures | 9 patients previously in bandaging | ✓ | ✓ | ✓ | |||
Circaid changed its name to JuxtaCures; however, this is the same device.
3.2. Ulcer healing
Within the randomised trial, only patients with bilateral venous ulcers were enrolled. The limbs were randomised to one in bandaging and one in JuxtaCures, and ulcer healing was compared between the bandaged and JuxtaCures device limbs in each individual patient. There was significantly faster healing in JuxtaCures (HR 0.56 [0.33‐0.96]; P = 0.0173); however, the total number of patients with a healed ulcer was 4/12 in both cohorts. The ulcer area reduction rate was faster in the JuxtaCures group (2.93 cm2/wk ± 0.60 v 2.30 cm2/wk ± 0.70; P = 0.369).17 Improved healing was also seen in five further case series,19, 20, 24, 25, 31 with Bradley et al19 noting an initial deterioration with increasing exudate up to week 3, then a dramatic improvement. One series by Brizzio et al22 studied 35 patients, placing them into five cohorts including stockings (15‐20, 20‐30, or 30‐40 mm Hg), multilayered bandages, or JuxtaCures. These patients had no history of compression bandaging and were given the most appropriate device clinically, therefore, although those in JuxtaCures did not heal as well as those in stockings, the study reported that those in JuxtaCures had worse ulcers initially.
3.3. Cost
Five articles reported a cost saving using the Velcro devices. Williams29 reported a cost saving in 15 patients from week 4 onwards, and over a 6 month period there was a cost saving in staff time from £30 000 to £11 000, as well as £19 000 saved in bandaging. Bradley19 reported a reduction in wound dressing costs from just over £5000 to just over £1000 over a 12‐week period, and a total cost saving in 10 patients over a 6 month period of £8400. Elvin23 reported a decrease in dressing costs across 26 patients from £9701.12 to £4317.56, and in compression from £20 130.76 to £5580.64. Freeman25 reported 2 separate cases, with a total cost saving over a 3‐month period from £4792.20 to £670.46, and £898.98 to £586.10. Finally, Nugent24 reported a single case involving a cost saving from £3300 over the previous 12 months, down to £732 to almost heal the patient.
3.4. Nursing time
The length of nurse time required for the appointment was reported by Freeman30 and Wicks.31 Both reported a reduction from 40 minutes when applying bandaging, down to 19 and 22 minutes, respectively.
Five studies19, 21, 23, 28, 30 all reported a reduction in the number of nursing appointments required by up to two thirds, or reducing clinic appointments to 1 per week.
Five studies also reported a reduction in total nursing time. Elvin23 reported a time saving across 26 patients over 6 months, from 55 hours 16 to 22 hours 50. Wicks21 noted a time saving across the 16 patients from 31 hours 40 down to 11 hours 22 per week. Bradley19 reported a time saving per week across 10 patients from 7 hours down to 2 hours 50. Freeman 2015 reported on two cases, showing a time reduction of 42 hours down to 3.25 hours, and 10 to 2.5 hours over the total treatment period. Williams29 reported a reduction in nursing time by over 50% per patient.
3.5. Patient satisfaction
Nine articles reported on patient satisfaction; however, none used a validated generic or disease‐specific quality of life score. Blecken17 asked patients to rate their satisfaction from 1 to 3. Higher rates of satisfaction were found in the JuxtaCures limb but this was not statistically significant (2.92 ± 0.08 v 2.58 ± 0.15 P = 0.104). The article by Lawrence26 highlighted the advantages for those wishing to self‐care and wear their own shoes. All other articles reported improved patient compliance,24 empowerment,31 less pain,29 better quality of life,28 and being happier with the device.21 Ehmann32 reported that all patients were pleased with the Velcro device allowing daily hygiene; however, interlacing devices were subjectively harder to apply. In addition, Freeman30 reported that 6 out their 9 participants preferred to continue in JuxtaCures, whereas 1 was unable to care for the device and 2 preferred to return to bandaging.
3.6. Tissue quality
Ehmann18 examined patients limb circumference and tissue density showing a significant reduction in limb circumference, and an improvement in tissue density in those using the Velcro device.
3.7. Pressure
Kline27 monitored sub dressing pressures, and identified that the Velcro device had higher mean compression than those using elastic stockings (47 mm Hg at ankle, 35 mm Hg at knee v 26 mm Hg at ankle, and 23 mm Hg at knee).
4. DISCUSSION
This systematic review has identified potential benefits of using Velcro wraps for treating venous ulceration over traditional compression bandaging, particularly with regard to nursing time, cost, and potentially patient satisfaction. There are also several reports of improvement in ulcer healing times although the evidence for this remains poor.
Evidence suggests that higher pressure compression therapy is favoured for patients with venous ulceration.33 The study by Kline27 identified higher pressure than 4 layer bandaging in the Velcro wrap cohort, and with the adjustable nature of the Velcro devices patients should be able to maintain pressure more accurately between dressing changes. In addition, the study by Ehmann18 identified limb circumference and tissue density improvement in the Velcro device. These may explain in part why several studies identified either faster healing rates, or healing in patients with long‐standing ulceration despite previous compression bandaging, as bandages slipping or losing pressure between dressings could have a major adverse effect on efficacy. A further appropriately powered randomised controlled trial to evaluate the role of Velcro devices in ulcer healing is indicated to evaluate this role further.
A significant advantage of Velcro devices is the reduction in nursing time both in terms of a reduction in appointments, and shorter dressing changes, whilst empowering patients to self‐care. Following an initial phase of high exudate and patient training, dressings can often be changed by a practice nurse once per week for 20 minutes, compared with 2 to 3 times per week for 40 minute or longer appointments, thus saving significant patient and nursing time. However, it should be noted that this was not statistically tested, and a trial is required to investigate this further. In addition, all studies reporting on costs identified a significant saving of at least 50% or greater because of the reduction in dressings, bandaging, and nursing time. A health economic evaluation on a large scale would seem prudent given these reports.
Venous ulceration significantly impacts patients quality of life, and one factor in this is bandaging. Bandages slip and impact on mobility and wearing shoes,34, 35 which can affect patient compliance and satisfaction. Although this systematic review has identified anecdotal improvements in markers of quality of life using the Velcro device, there remains a lack of true comparator, and no use of either generic or disease‐specific quality of life scores, therefore, this requires further longitudinal study. A single study identified improved patient compliance,24 and there was a significant reduction in nursing visits in those with Velcro devices, which may in part be because of the ability for patients to apply these devices themselves, and undertake their own dressing changes.
Although this systematic review highlights several areas of potential improvement in the care of patients with venous ulceration by using Velcro devices, there is only a single randomised controlled trial17 that is small and of poor quality. All other studies are case series that are likely to be biased in terms of patient selection. There is also very inconsistent reporting of outcomes between the studies highlighting potential reporting bias. It is imperative that a large, adequately powered randomised controlled trial is now undertaken in order to determine whether Velcro wrap devices affect ulcer healing rates and time to healing, as well as patient quality of life, and cost.
5. CONCLUSION
This systematic review highlights that Velcro wrap devices for the treatment of venous ulceration have significant potential benefits for patients and the health care system in terms of cost, nursing time, patient satisfaction, and potentially ulcer healing; however, further good quality evidence is essential to thoroughly evaluate these devices in the setting of a randomised controlled trial.
Stather PW, Petty C, Howard AQ. Review of adjustable velcro wrap devices for venous ulceration. Int Wound J. 2019;16:903–908. 10.1111/iwj.13116
REFERENCES
- 1. Guest JF, Ayoub N, McIlwraith T, et al. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open. 2015;5(12):e009283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lal BK. Venous ulcers of the lower extremity: definition, epidemiology, and economic and social burdens. Semin Vasc Surg. 2015;28(1):3‐5. [DOI] [PubMed] [Google Scholar]
- 3. Guest JF, Ayoub N, McIlwraith T, et al. Health economic burden that different wound types impose on the UK's National Health Service. Int Wound J. 2017;14(2):322‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scottish Intercollegiate Guidelines Network (SIGN) . SIGN Guideline 120: The Care of Patients With Leg Ulcers. 2010. https://www.sign.ac.uk/sign-120-management-of-chronic-venous-leg-ulcers.html. Accessed October 10, 2018.
- 5. Rasmussen JC, Aldrich MB, Tan IC, et al. Lymphatic transport in patients with chronic venous insufficiency and venous leg ulcers following sequential pneumatic compression. J Vasc Surg Lymphat Disord. 2016;4(1):9‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Iglesias C, Nelson EA, Cullum NA, Torgerson DJ. VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers. Health Technol Assess. 2004;8(29):iii 1‐105. [DOI] [PubMed] [Google Scholar]
- 7. Ashby RL, Gabe R, Ali S, et al. VenUS IV (venous leg ulcer study IV)—compression hosiery compared with compression bandaging in the treatment of venous leg ulcers: a randomised controlled trial, mixed‐treatment comparison and decision‐analytic model. Health Technol Assess. 2014;18(57):1‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wong IKY, Andriessen A, Lee DTF, et al. Randomized controlled trial comparing treatment outcome of two compression bandaging systems and standard care without compression in patients with venous leg ulcers. J Vasc Surg. 2012;26(1):102‐110. [DOI] [PubMed] [Google Scholar]
- 9. O'Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012;11:CD000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gohel MS, Barwell JR, Taylor M, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. Br Med J. 2007;335(7610):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gohel MS, Heatley F, Liu X, et al. A randomized Trial of early Endovenous ablation in venous ulceration. N Engl J Med. 2018;378(22):2105‐2114. [DOI] [PubMed] [Google Scholar]
- 12. Miller C, Kapp S, Newall N, et al. Predicting concordance with multi‐layer compression bandaging. J Wound Care. 2011;20(3):101‐102. [DOI] [PubMed] [Google Scholar]
- 13. Moffatt C. Variability of pressure provided by sustained compression. Int Wound J. 2008;5(2):259‐265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Williams A. A review of the evidence for adjustable compression wrap devices. J Wound Care. 2016;25(5):242‐247. [DOI] [PubMed] [Google Scholar]
- 15. Williams A. An updated review of the evidence for adjustable compression wrap devices in the lower limb. Nurse Prescribing. 2018;15(S10):6‐13. [Google Scholar]
- 16. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Blecken SR, Villavicencio JL, Kao TC. Comparison of elastic versus nonelastic compression in bilateral venous ulcers: a randomized trial. J Vasc Surg. 2005;42(6):1150‐1155. [DOI] [PubMed] [Google Scholar]
- 18. Ehmann S, Whitaker JC, Hampton S, Collarte A. Multinational, pilot audit of a Velcro adjustable compression wrap system for venous and lymphatic conditions. J Wound Care. 2016;25(9):513‐520. [DOI] [PubMed] [Google Scholar]
- 19. Bradley M, Nelis L, Reagen M, et al. Using an adjustable compression device to manage venous leg ulcers. J Community Nurs. 2017;31(2):40‐44. [Google Scholar]
- 20. Mahoney K. A simple and effective solution to preventing recurrent venous leg ulcers. J Community Nurs. 2016;30(4):24‐28. [Google Scholar]
- 21. Wicks G. An alternative to compression bandaging in venous leg ulcers. J Community Nurs. 2015;29(4):40‐47. [Google Scholar]
- 22. Brizzio EO, Blättler W, Rossi G, et al. Healing venous ulcers with different modalities of leg compression. Unexpected findings of a pilot study. Phlebologie. 2006;35(5):249‐255. [Google Scholar]
- 23. Elvin S. Cost efficacy of using juxta CURES™ and UCS™ debridement cloths. J Community Nurs. 2015;29(2):62‐65. [Google Scholar]
- 24. Nugent L. Juxta CURES: compression for healing venous leg ulcers. Br J Community Nurs. 2013;18(suppl):S40‐S45. [PubMed] [Google Scholar]
- 25. Freeman N. Enhancing a venous leg ulcer treatment pathway with compression wrap devices. Wounds UK. 2015;11(3):38‐45. [Google Scholar]
- 26. Lawrence G. Juxta CURES: an innovative method of providing compression for leg ulcer management. Wounds UK. 2014;10(1):64‐70. [Google Scholar]
- 27. Kline CN, Macias BR, Kraus E, et al. Inelastic compression legging produces gradient compression and significantly higher skin surface pressures compared with an elastic compression stocking. Vascular. 2008;16(1):25‐30. [DOI] [PubMed] [Google Scholar]
- 28. Dowsett C, Elson D. Meeting the challenges of delivering leg ulcer services. Wounds UK. 2013;9(1):90‐95. [Google Scholar]
- 29. Williams S. Notes on a six‐month evaluation of juxtacures™ by one community nursing team. J Community Nurs. 2017;31(3):38‐42. [Google Scholar]
- 30. Freeman N, Norris R. Using an adjustable compression system to treat community leg ulcers. J Community Nurs. 2016;30(3):47‐52. [Google Scholar]
- 31. Todhunter J. Empowering patients to self‐care with a Velcro wrap compression device. J Community Nurs. 2017;31(4):28‐30. [Google Scholar]
- 32. Ehmann S, Bock K. Case report to demonstrate the need for selection criteria for optimal adjustable Velcro wrap prescription. J Wound Care. 2018;27(suppl 1):S10‐S17. [DOI] [PubMed] [Google Scholar]
- 33. Milic DJ, Zivic SS, Bogdanovic DC, et al. The influence of different sub‐bandage pressure values on venous leg ulcers healing when treated with compression therapy. J Vasc Surg. 2010;51(3):101‐102. [DOI] [PubMed] [Google Scholar]
- 34. Adderley U, Thompson C. A study of the factors influencing how frequently district nurses re‐apply compression bandaging. J Wound Care. 2007;16(5):217‐221. [DOI] [PubMed] [Google Scholar]
- 35. Meyer FJ, McGuinness CL, Lagattolla NRF, Eastham D, Burnand KG. Randomized clinical trial of three‐layer paste and four‐layer bandages for venous leg ulcers. Br J Surg. 2003;90(8):934‐940. [DOI] [PubMed] [Google Scholar]


