Abstract
Peripheral arterial disease (PAD) and its most severe form, critical limb ischaemia (CLI), are very common clinical conditions related to atherosclerosis and represent the major causes of morbidity, mortality, disability, and reduced quality of life (QoL), especially for the onset of ischaemic chronic leg ulcers (ICLUs) and the subsequent need of amputation in affected patients. Early identification of patients at risk of developing ICLUs may represent the best form of prevention and appropriate management. In this study, we used a Prediction System for Chronic Leg Ulcers (PredyCLU) based on fuzzy logic applied to patients with PAD. The patient population consisted of 80 patients with PAD, of which 40 patients (30 males [75%] and 10 females [25%]; mean age 66.18 years; median age 67.50 years) had ICLUs and represented the case group. Forty patients (100%) (27 males [67.50%] and 13 females [32.50%]; mean age 66.43 years; median age 66.50 years) did not have ICLUs and represented the control group. In patients of the case group, the higher was the risk calculated with the PredyCLU the more severe were the clinical manifestations recorded. In this study, the PredyCLU algorithm was retrospectively applied on a multicentre population of 80 patients with PAD. The PredyCLU algorithm provided a reliable risk score for the risk of ICLUs in patients with PAD.
Keywords: amputation, chronic leg ulcer, critical limb ischaemia, fuzzy logic, peripheral arterial disease
1. INTRODUCTION
Peripheral arterial disease (PAD) is one of the most common disease related to atherosclerosis and represents a major cause of chronic illness, associated with cardiovascular morbidity, mortality, disability, and reduced quality of life (QoL). More than 27 million people in the Western world (equals to 16% of people aged over 55 years) are affected by PAD.1, 2
Generally, about 20% of patients with PAD are found to deteriorate significantly over a 5‐year period and one‐third of these patients will progress to Critical limb Ischaemia (CLI) that represents the more severe form of PAD. CLI includes persistent rest pain, and, in the more advanced stages, patients develop ulceration and gangrene that may lead to minor or major amputations of lower limbs. It is estimated that about 30% of these patients have the possibility to have an amputation, and only 45% of these will be alive with both legs intact.3, 4, 5, 6
The risk factors for progression of PAD to the advanced forms of CLI and to the need for amputation are not yet fully investigated and established. 7
Fuzzy logic is a flexible mathematical system built on the experience of experts, which can model nonlinear function of arbitrary complexity, and it was used in a previous experience in order to calculate the risk of chronic venous ulcers. It was then created a Prediction System for Chronic Leg Ulcers (PredyCLU) applied to venous ulcers. 8
The aim of this study was to validate the PredyCLU algorithm in patients with PAD in order to describe the possibility to develop ischaemic chronic leg ulcers (ICLUs), and the subsequent need of amputation.
2. MATERIALS AND METHODS
The study was a multicentre retrospective evaluation performed in the Department of Medical and Surgical Sciences of University “Magna Graecia” of Catanzaro; the Department of Public Health, University of Naples “Federico II”; and the Department of Morphology, Surgery and Experimental Medicine, University of Ferrara. This study was approved by the Institutional Review Board in accordance with the Declaration of Helsinki and the Guideline for Good Clinical Practice.
2.1. Selection criteria and patients
We designed a retrospective case‐control study comparing patients with PAD with ICLUs, (Grade III, categories 5 and 6 of Rutherford Classification of PAD) 9 (cases), with a control group of patients with PAD without ICLUSs (grades 1‐4, categories 1‐4 of Rutherford Classification of PAD). 9
Moreover, information regarding factors indicated in Table 1 must have been available for all patients to be included. Exclusion criteria were the presence of leg ulcers other than the ischaemic type, any history of leg ulcer in the control group, impossibility to have a complete clinical history according to the factors listed in Table 1.
TABLE 1.
Items investigated
| Age |
| Gender male |
| Diabetes duration (years) |
| Diabetes treatment |
| Limb ischaemic pain |
| Renal insufficiency |
| CRP > 3 mg/L |
| Dyslipidaemia (LDL/HDL/triglycerides/total cholesterol) |
| Urinary albumin: creatinine (mg/mmol) |
| Peripheral sensory neuropathy |
| Smoking |
| At least a previous cardiovascular event |
| At least a previous coronary event |
| Antihypertensive treatment |
| Arterial pressure (min/max) |
| Angina |
| Previous MI |
| Coronary revascularisation |
| At least a previous cerebrovascular event |
| Stroke |
| Carotid surgery |
Abbreviations: CRP, C‐reactive protein; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; MI, myocardial infarction.
2.2. The application of PredyCLU for the risk of ischaemic ulcers onset and the evaluation phase
In this study, we used the PredyCLU algorithm as described in a previous study.ss In the evaluation phase, patients' clinical data were retrieved from anonymous forms that were made available and assigned to two investigators who were also blinded to the clinical information concerning the presence of ICLUs.
3. RESULTS
The patient population consisted of 80 subjects with PAD (Table 2), of which 40 patients (100%) (30 males [75%] and 10 females [25%]; mean age 66.18 years; median age 67.50 years) had ICLUs and represented the case group.The other 40 patients (100%) (27 males [67.50%] and 13 females [32.50%]; mean age 66.43 years; median age 66.50 years) did not have ICLUs and represented the control group.
TABLE 2.
Patient characteristics
| Characteristics | Group A (40 pts) | Group B (40 pts) | P |
|---|---|---|---|
| Male | 30 (75%) | 27 (67.50%) | Not significant |
| Female | 10 (25%) | 13(32.50%) | Not significant |
| Age | 66.18 | 66.43 | .88 |
| Diabetes duration (years) | 39 (97.50) | 38 (95.00) | <.0001 |
| Diabetes treatment | 39 (97.50%) | 38 (95.00) | <.0001 |
| Limb ischaemic pain | 39 (97.50%) | 35(87.50%) | <.0001 |
| Renal insufficiency | 24 (60.00%) | 21 (52.50%) | .0191 |
| CRP > 3 mg/L | 28 (70.00%) | 20 (50.00%) | .0038 |
| Dyslipidaemia (LDL/HDL/triglycerides/total cholesterol) | 20 (50.00%) | 20 (50.00%) | .8628 |
| Urinary albumin: creatinine (mg/mmol) | 26 (65.00%) | 22 (55.00%) | .8307 |
| Peripheral sensory neuropathy | 38 (95.00%) | 24 (60.00%) | <.0001 |
| Smoking | 34 (85.00%) | 30 (75.00%) | .0734 |
| at least a previous cardiovascular event | 17 (42,50%) | 10 (25.00%) | .1003 |
| at least a previous coronary event | 16 (40.00%) | 21 (52.50%) | .3842 |
| Antihypertensive treatment | 28 (70.00%) | 29 (72.50%) | .5630 |
| Arterial pressure (min/max) | 37 (92.50%) | 36 (90.00%) | .0044 |
| Angina | 32 (80.00%) | 6 (15.00%) | <.0001 |
| Previous MI | 26 (65.00%) | 1 (2.50%) | <.0001 |
| Coronary revascularisation | 22 (55.00%) | 3 (7.50%) | <.0001 |
| At least a previous cerebrovascular event | 21 (52.50%) | 3 (7.50%) | .0023 |
| Stroke | 6 (15.00%) | 22 (55.00%) | .0987 |
| Carotid surgery | 14 (35.00%) | 13 (32.50%) | .9262 |
Abbreviations: CRP, C‐reactive protein; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; MI, myocardial infarction.
Full patients' demographics and clinical characteristics are shown in Table 2, and P values have been calculated between groups (P value of ≤.05 was used to denote statistical significance).
Suggestively, after PredyCLU evaluation and splitting of the results per group, all patients of the case group (with ICLUs) and all patients of control group (without ICLUs) were allocated in two distinct zones of the graphic elaborated by PredyCLU (Fig 1).
FIGURE 1.
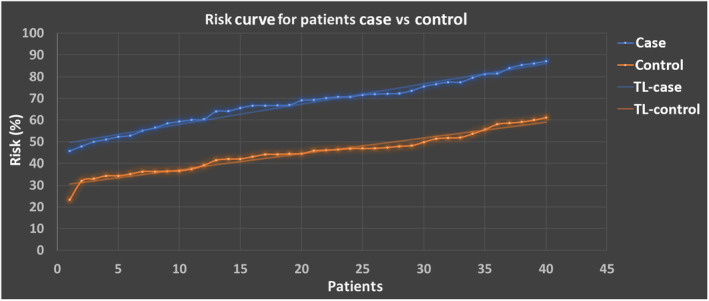
Risk curve for the patients of case group versus control group. In blue are shown the cases and in orange are shown the controls. The image also shows the TL for both cases. TL, trend line
In Figure 1, the risk curves for assessed patients are shown: in blue (top), the level of the risk for patients with ulcer. The bottom curve, in orange, denotes the level of the risk for patients without ulcer. The dotted line on the curve represents the average risk. We found a good separability, on the sample considered, between patients with ulcer compared with patients without ulcer.
In fact, the data processing had produced the risk stratification as shown in Figure 2. A risk score up to 47.84 (±8.69)% identified a low risk area for patients. All control group cohort was allocated in this area. A score more than 48% represented the possibility to develop ICLUs and a score over 67.87 (±11.10)% identified the high‐risk area. All case group cohort was allocated in the aforementioned intervals.
FIGURE 2.
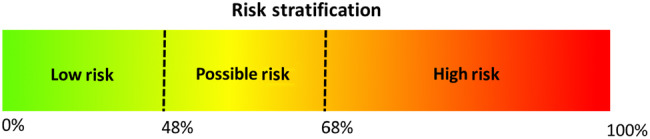
Stratification of the risk. A risk score between 0% and 48% identifies a low‐risk area for patients. A score between 48% and 68% represents the possibility to develop ICLUs and over 68% starts the high‐risk area. ICLUs, ischaemic chronic leg ulcers
Furthermore, in patients of case group, the higher was the risk calculated with the PredyCLU, the more severe were the clinical manifestations recorded (data not shown).
4. DISCUSSION
PAD affects a significant number of people and represents an important cause of disability, especially for its complications such as ICLUs and limb loss.1, 2, 3, 4, 5, 6 As patients progress to CLI, not only do they have a significant increase in risk of limb loss, but they also have an increase in mortality. Therefore, an effective classification of patients with PAD is important to help determine their prognosis. 10 We have also limited data to predict which patients with CLI will progress to ICLUs and eventually to amputation.7, 10
A more tailored risk prediction is fundamental to improve clinical decision making about which patients will benefit from specific interventions and to evaluate and improve risk‐adjusted outcomes and the use of health care resources. 11
As shown in a previous study, 8 in the past few years, an increasing number of medical publications use fuzzy logic to process data due to its capabilities to emulate the process of human reasoning. In the present study, 8 a similar approach was used in order to calculate the overall risk of ICLUs for the patients in both groups. We customised the PredyCLU algorithm with the factors listed in Table 1 and then processed the data collected for each patient. Figure 1 shows the data sorted by the risk level. A good distinction is also evident in the sample considered, between patients with ICLUs and patients without ICLUs, and it is shown in Figure 2.
In our study, the main factors that increase the risk of progression of CLI towards limb ulceration are the presence of diabetes, limb ischaemic pain, peripheral sensory neuropathy, angina, previous myocardial infarction (MI), and coronary revascularisation. Although the first four aforementioned risk factors are quite obvious, the latter three factors concern heart‐related conditions and procedures, and should be further investigated and they represent a novel finding in our study.
Overall considered, our study showed that the PredyCLU algorithm could be effectively used in patients with PAD in order to give a reliable risk stratification tool towards the risk of ischaemic ulcer onset.
Commonly, in medical practice, the diagnosis of the disease uses imprecise and vague linguistic terms. In addition, a large number of symptoms must be related to each other. 8
The fuzzy logic technique is a powerful artificial intelligence approach, which was developed based on the Fuzzy Set Theory. L. A. Zadeh first introduced the Fuzzy Set Theory in 1965 12 and, similar to fuzzy logic, medicine works in the field of uncertainty. 13 As reported in previous papers, fuzzy logic has been used in many areas of medicine and has proven to be suitable for supporting medical decisions.8, 13
Thanks to its characteristics, fuzzy logic tries to model the typical way of human reasoning that leads to reasonable decisions in practical situations where there are good doses of uncertainty and inaccuracy. 12
There are two main limits in our study: we evaluated all the risk factors listed in the patient history in one unique frame time, as if they were present simultaneously and not succeeding each other, and secondly, the cohort population was quite small.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Serra R, Bracale UM, Barbetta A, et al. PredyCLU: A prediction system for chronic leg ulcers based on fuzzy logic; part II—Exploring the arterial side. Int Wound J. 2020;17:987–991. 10.1111/iwj.13360
REFERENCES
- 1. Stehouwer CD, Clement D, Davidson C, et al. Peripheral arterial disease: a growing problem for the internist. Eur J Intern Med. 2009;20(2):132‐138. [DOI] [PubMed] [Google Scholar]
- 2. Brevetti G, Oliva G, Silvestro A, Scopacasa F, Chiariello M, Peripheral Arteriopathy and Cardiovascular Events (PACE) Study Group . Prevalence, risk factors and cardiovascular comorbidity of symptomatic peripheral arterial disease in Italy. Atherosclerosis. 2004;175(1):131‐138. [DOI] [PubMed] [Google Scholar]
- 3. Aboyans V, Criqui MH, Denenberg JO, Knoke JD, Ridker PM, Fronek A. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. 2006;113(22):2623‐2629. [DOI] [PubMed] [Google Scholar]
- 4. Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter‐Society Consensus (TASC). J Vasc Surg. 2000;31(1 Pt 2):S1‐S296. [PubMed] [Google Scholar]
- 5. Hirsch AT, Haskal ZJ, Hertzer NR. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary. A collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter‐Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239‐1312. [DOI] [PubMed] [Google Scholar]
- 6. Fowkes FG, Aboyans V, Fowkes FJ, McDermott MM, Sampson UK, Criqui MH. Peripheral artery disease: epidemiology and global perspectives. Nat Rev Cardiol. 2017;14(3):156‐170. [DOI] [PubMed] [Google Scholar]
- 7. Nehler MR, Duval S, Diao L, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg. 2014;60(3):686.e2‐695.e2. [DOI] [PubMed] [Google Scholar]
- 8. de Franciscis S, Fregola S, Gallo A, et al. PredyCLU: a prediction system for chronic leg ulcers based on fuzzy logic; part I ‐ exploring the venous side. Int Wound J. 2016;13(6):1349‐1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517‐538. [DOI] [PubMed] [Google Scholar]
- 10. Vallabhaneni R, Kalbaugh CA, Kouri A, Farber MA, Marston WA. Current accepted hemodynamic criteria for critical limb ischemia do not accurately stratify patients at high risk for limb loss. J Vasc Surg. 2016;63(1):105‐112. [DOI] [PubMed] [Google Scholar]
- 11. Chung J, Modrall JG, Valentine RJ. The need for improved risk stratification in chronic critical limb ischemia. J Vasc Surg. 2014;60(6):1677‐1685. [DOI] [PubMed] [Google Scholar]
- 12. Kosko B. Fuzzy Thinking: the New Science of Fuzzy Logic. New York, NY: Hyperion Press; 1993. [Google Scholar]
- 13. Torres A, Nieto JJ. Fuzzy logic in medicine and bioinformatics. J Biomed Biotechnol. 2006;2006:91908‐91907. 10.1155/JBB/2006/91908. [DOI] [PMC free article] [PubMed] [Google Scholar]


