Abstract
Pressure ulcers lead to discomfort for patients and may have an important impact on a patient's quality of life. Measure the incidence and prevalence of pressure ulcers in a Hospice environment; evaluate the risk factors associated with pressure ulcers; and calculate the incidence of Kennedy Terminal Pressure Ulcers. This multicentre prospective cohort study enrolled 440 cancer patients in advanced phase, consecutively admitted to five hospices of the AUSL della Romagna (Italy), during a period of 1 year. Five hundred more patients were excluded from the study because of inability to sign the consent form or refusal to participate. All patients were adults above 18 years of age. The National Pressure Advisory Panel Classification System was used to evaluate the pressure ulcers. Potential risk predictors were evaluated through the Braden Scale, the Numerical Scale, and the Pain Assessment in Advanced Dementia Scale. Starting in September 2016, 214 (48.6%) females and 226 (51.4%) males were analysed. The incidence of pressure ulcers in the total population was 17.3%. The risk factors that influence the development of pressure ulcers were age, proximity to death, and duration of stay in Hospice. The incidence of Kennedy Terminal Pressure Ulcers was 2.7%. This study demonstrates that 17.3% of all patients admitted to a hospice setting developed a pressure ulcer. The longer the patients stay in hospice and the clinical condition deteriorates, the higher the risk of developing a pressure ulcer.
Keywords: cancer patients in advanced phase, hospice setting, incidence, Kennedy terminal ulcer, pressure ulcer
1. INTRODUCTION
Palliative care (PC) is an approach that aims to improve the quality of life physically, psychologically, socially, and spiritually in patients affected by illnesses with an unfavourable prognosis. PC focuses on the patient and their families, respecting the patients' will and wishes. According to The World Health Organisation (WHO), about 40 million people around the world need PC each year, and the number will continue to increase.1, 2
Literature demonstrates that very few studies have been evaluating the incidence, prevalence, and risk factors of pressure ulcers (PUs) in the hospice setting. In Italy, the prevalence of PUs in hospital settings varies from 4.7% to 32%. The prevalence of PUs in nursing homes is 22%, but when it comes to the hospice setting, no exact incidence and prevalence are mentioned. In an overview from 2012, Langemo concludes that the incidence and prevalence in the USA in hospice settings are partially unknown. It is estimated that around one third of patients admitted to hospices will develop ulcers during their stay, and about 50% of these are PUs. According to National Pressure Ulcer Advisory Panel (NPUAP), the prevalence is about 10% to 11%, but it is probably underestimated. In an Italian prospective study, 414 patients were examined. The prevalence was 22.9% and the incidence 6.7%; 15 patients (3.6%) developed a PU during the last 6 days of life. From a review of PU prevalence and incidence across Scandinavia, Iceland, and Ireland emerges an incidence of 20.4% in hospice settings.3, 4, 5, 6, 7, 8
The lack of studies conducted in the hospice setting has created a profound need to calculate incidence and prevalence of PUs and to comprehend more thoroughly which risk factors may have an impact on the development of PUs; this has led us to organize this study.
We have also chosen to include a little known phenomenon in our study: the Kennedy Terminal Ulcers (KTU). These ulcers are characterised by a fast tissue deterioration, named ‘Skin Failure’. They differ from normal PUs because they are able to pass from category 1 to category 4 in only a few hours. Usually, they appear in the final 48 to 72 hours of life and are frequently localised on the sacrum. In literature, they are often described with a precise form as pear, horseshoe, or butterfly shaped. Furthermore, they are described with specific colours as yellow, black, and purple. The exact origin has not been found yet, but it is thought that the phenomenon may be attributed to a lack of blood perfusion in the tissues or a deterioration process of the internal organs reflecting on the skin what is going on inside the body.9, 10, 11, 12
2. METHOD
A multicentre observational prospective cohort study has been conducted on cancer patients in an advanced phase, consecutively admitted to five hospices of the ‘AUSL della Romagna’ (Italy) during a period of 12 months. The hospice of Savignano started the data collection in September 2016, the other hospices followed, and in November 2017, the data collection was concluded.
The study predicted the enrolment of competent patients and the study was conducted following the procedures in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2013. Before the enrolment, the patients received complete information about the purpose of the study and they signed an informed consent thereby accepting the participation in the study.
All patients were adults above 18 years of age, capable of expressing their consent.
At the moment of admission to hospice, all general data were sampled in Case Report Form 1 (CRF) within 48 hours by a nurse. Among the general data reported in CRF 1, we evaluated in the analysis: age, sex, sensorial perception, state of consciousness, cachexia, mobilisation, pain, issues related to moisture, dyspnoea, pharmacological sedation, pathological fractures, and forced position caused by pathology. The presence of PUs, at the moment of admission to the hospice was registered and described according to the NPUAP Classification system.13 Variables related to care, such as mattresses, friction and shear, postures, incontinence pads, and lotion were also analysed. Every single patient counts only once in this study.
In the daily care activities and during the whole conduction of the study, the nurses were responsible for daily skin inspections and the description of skin changes. In case of a new PU occurrence, the CRF 2 was filled out. This procedure was repeated every time a new PU developed in a patient. The collection of data stopped when the patient was either discharged or died.
3. STATISTICS
Statistical analysis was performed on all recorded variables using the value calculations of mean, standard deviation, median, percentiles and tables of absolute and percentage frequencies. Univariate analysis was applied to the relationship between the single variables and the outcome, ‘appearance of a new lesion’, through the use of Student test T, the Mann‐Whitney non‐parametric test, and the Chi Squared test. In all tests, the statistical significance threshold was set at 0.05. Statistical significant variables from the univariate analysis were inserted in a multivariate logistical regression model to verify the existence of possible confounding factors and to obtain adjusted Odds ratio for each factor in equivalence to the other conditions considered in this model. All statistical analysis was conducted using the software Stat Intercooled.
4. ETHICS
This protocol has been approved by the Ethics Comity of Romagna (Comitato Etico di IRST e di Area Vasta Romagna), and all patients enrolled have been informed about the subject and the purpose of the study and have signed an informed consent. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2013.
5. RESULTS
Starting September 2016, in five hospices (Forlimpopoli, Savignano sul Rubicone, Lugo, Faenza e Dovadola), 440 consecutively admitted competent advanced phase cancer patients, 214 (48.6%) females and 226 (51.4%) males were enrolled and analysed. Five hundred patients were excluded from the study because of inability to sign the consent form or refusal to participate. Therefore, 440/940 (47%) of the entire population has participated in the study and has been analysed.
The mean age of the population studied was 73.7 years, the minimum age was 37 and the maximum age was 98. The length of stay in hospice was on average 18.1 days (DS 14.35; range 1‐94 days); 300 patients (68.6%) out of 437 died in Hospice and the remaining 137 (31.4%) were discharged either to their homes, to another hospital facility or to rest homes. In the three cases, this was not mentioned (Table 1).
Table 1.
Descriptive analysis of the characteristics of the population
| Total patients N (n = 440) | |
|---|---|
| ‐ | Media (ds) |
| Age | 73.7 (12.6) |
| Age distribution/centre | |
| Dovadola | 79.6 (10.5) |
| Lugo | 77 (10.8) |
| Faenza | 76.2 (12) |
| Savignano sul Rubicone | 71.6 (12.5) |
| Forlimpopoli | 69.9 (13.2) |
| ‐ | Median (IIQ) |
| Braden Scale | 15 (13‐18) |
| Pain valuated with numeric rating scale (NRS) | 0 (0‐2) |
| Pain assessment in advanced dementia scale (PAINAD) | 0 (0‐2.5) |
| ‐ | n (%) |
| Male patients | 226 (51.4%) |
| Female patients | 214 (48.6%) |
| Primary tumour | |
| Pulmonary | 108 (24.7%) |
| Gastrointestinal | 82 (18.8%) |
| Genitourinary | 82 (18.8%) |
| Hepatic‐bile‐pancreatic | 62 (14.1%) |
| Haematological | 30 (6.9%) |
| Breast | 29 (6.6%) |
| Head and neck | 20 (4.6%) |
| Brain and nervous system | 11 (2.5%) |
| Skin (Melanoma) | 7 (1.6%) |
| Other | 6 (1.4%) |
| Number of patients with pain at the moment of entrance evaluated with the Scales NRS and PAINAD (not related to a presence of PU) | 131/430 (30.5%) |
| Cachexia | |
| BMI 18.5‐24.9 | 252 (57.8%) |
| weight loss >/< 20% | 139 (31.9%) |
| weight loss >/< 30% | 45 (10.3%) |
| State of consciousness | |
| Patients awake at the entrance | 422 (95.91%) |
| Drowsiness | 18 (4.1%) |
| Dyspnoea at the moment of entrance | 130 (29.6%) |
| Pathological fractures at the entrance | 18 (5%) |
| Obligatory position at the entrance | 80 (18.2%) |
| Incontinence pads | 253 (57.6%) |
| Skin lotions | 149 (33.9%) |
| Mattresses | |
| Polyurethane foam mattresses | 241 (55.3%) |
| Dynamic air pressure‐relieving mattresses | 159 (36.5%) |
| Other types of mattresses | 36 (8.2%) |
6. PRESSURE ULCER POINT PREVALENCE AT THE MOMENT OF ADMISSION
Out of 440 enrolled patients, 439 patients were evaluated. In one case, these data are missing. Of 439 patients, 112 (25.5%) presented one or more PUs at the moment of admission. A total of 140 PUs were observed. Twenty (19.1%) of the 112 patients complained pain in relation to the PU at the moment of admission (Table 2).
Table 2.
Characteristics of pressure ulcers (PUs)
| n (%) | |
|---|---|
| Population with PU distribution/centres at the moment of admission | |
| Hospice Lugo | 28 (25%) |
| Forlimpoli | 25 (22%) |
| Savignano Sul Rubicone | 23 (21%) |
| Faenza | 19 (17%) |
| Dovadola | 17 (15%) |
| Total | 112 (100%) |
| Location of PUs | |
| Sacrum | 87 (62.2%) |
| Heels | 24 (17.1% |
| Gluteus | 7 (5%) |
| Trochanter | 6 (4.3%) |
| Other parts of the body | 16 (11.4%) |
| NPUAP classification system. Categories of PUs | |
| Cat 1 | 62 (44.6%) |
| Cat 2 | 55 (39.6%) |
| Cat 3 | 11 (7.9%) |
| Cat 4 | 4 (2.9%) |
| Unstageable; depth unknown | 3 (2.1%) |
| Suspected deep tissue injury: depth unknown | 4 (2.9%) |
| 112 patients with PU at the moment of admission complained pain in relation to the PU | 20 (19.1%) |
7. INCIDENCE OF PRESSURE ULCERS
Seventy‐six (17.3%) patients out of the 440 patients enrolled developed a PU during their stay in Hospice. Out of the 76 patients who developed a PU, 61 (80%) patients did not have a PU at the moment of the entrance in hospice. Only 15/112 (13.4%) patients that presented one or more PUs at the moment of admission, developed a new PU. This means that patients who already had a PU at the entrance were more likely not to develop a PU during their stay. The reason for this could be found in a greater attention on behalf of the personnel during the daily care activities. In 10/76 (13.1%) cases, the patient complained pain in relation to the developed PU. In addition, the mean score of the NRS scale was 1.3 with a range 2 to 10 (DS 2.4).
The distribution of the incidence of PUs for each hospice is evidenced in Table 3; in Figures 1 and 2, the location and category of the PUs are described. The PUs were evaluated and described through the NPUAP classification system. The highest concentration of PUs, 34/76 (44.7%) were localised on the sacrum followed by 19/76 (25%) situated on the heels. Out of 76 PUs, 43 (56.6%) were a first category, and 16 (21%) were a second category. A total of 14.5% were a suspected deep tissue injury where the depth was unknown (Figures 1 and 2).
Table 3.
Incidence pressure ulcer (PU)/centre
| PU developed (n = 76) | PU non‐developed (=364) | ||
|---|---|---|---|
| Centre | n (%) | P (Test chi2) | |
| Savignano Sul Rubicone | 21 (27.6%) | 71 (19.5%) | |
| Forlimpopoli | 20 (26.3%) | 128 (35.2%) | |
| Lugo | 14 (18.4%) | 70 (19.2%) | .306 |
| Dovadola | 13 (17.2%) | 46 (12.6%) | |
| Faeenza | 8 (10.5%) | 49 (13.5%) | |
| Total | 76 (100%) | 364 (100%) | |
| ‐ | n (%) | ||
| Pain in relation to PUs developed in hospice (Score range on the numeric rating scale [NRS] scale min 2 and max 10). Score range Painad scale (0‐1) | 10/76 (13.1%) | 66/76 (85.5%) | |
Figure 1.
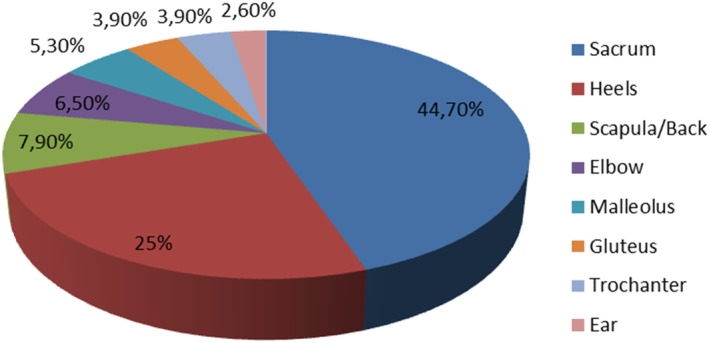
Location of pressure ulcers developed during the stay
Figure 2.
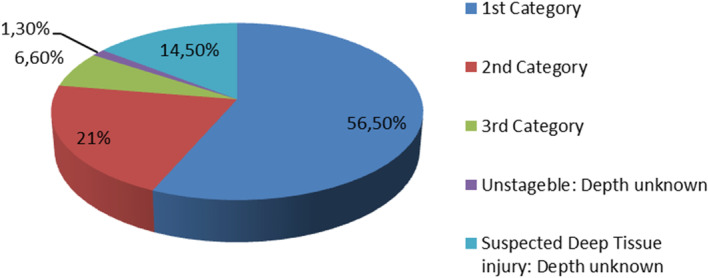
Categories of pressure ulcers developed during the stay
8. PERIOD PREVALENCE
Of 439 patients, 112 (25%) presented a PU at the moment of the entrance (Point Prevalence) and 76/440 (17.3%) patients developed a PU during their stay (Incidence). The Periodic Prevalence was: 188/440 (42.8%).
9. TIME ADMISSION – DEVELOPMENT PU
From the moment of admission to the hospice setting until the development of a PU the mean was 15.93 days (DS 12.3). The range was minimum 2 and maximum 53 days. From the first PU to the second PU the average was 16.89 days (DS 12.7). The range was minimum 10 and maximum 40 days.
10. TIME DEVELOPMENT PU – DEATH
From the moment of the development of a PU until the moment of death the mean was 10 days (DS 9.7). The range was 1 to 44 days. From the development of the second PU until the moment of death the mean was 10.5 days (DS 10.1) with a range of 6 to 37 days.
11. RISK FACTORS THAT DID NOT INFLUENCE THE PRIMARY OUTCOME
As described in Table 4, no significant differences between males and females were found (P = .993). The different diagnosis did not have an impact on the incidence of PU during the stay in hospice (P = .898). The Braden Scale Score in the patients who developed a new PU was not different from the score on the general population in hospice (P = .7996); the dynamic pressure – relieving mattresses did not have a preventive effect in developing PUs. The patients on dynamic air pressure‐relieving mattresses and the patients on polyurethane mattresses were both likely to develop PUs (P = .503). The presence of pain, valuated with NRS o PAINAD score, did not occur more frequently in patients who developed a PU as compared with those who did not develop one. Patients who already had a PU were more likely not to develop a new PU: as said before the cause of this could be a more accurate attention on behalf of the personnel when it comes to daily skin inspections in patients with PUs (Table 5).
Table 4.
Variables that did not influence the onset of new pressure ulcer (PU) (univariate analysis)
| PU developed (n = 76) | No PU developed (n = 364) | ||
|---|---|---|---|
| Mediana (IIQ) | Mann‐Whitney U test | ||
| The Braden scale | 15 (15.5) | 16 (15.5) | 16.6 |
| ‐ | n (%) | P (Test chi2) | |
| NRS | 43 (22.9) | 261 (30.8) | .031 |
| Sex | .0001 | ||
| Female | 37 (17.3) | 177 (82.7) | |
| Male | 39 (17.3) | 187 (82.7) | |
| Diagnosis primary tumour | |||
| Brain and nervous system | 2 (18.2) | 9 (81.8) | 4.193 |
| Haematological | 6 (20) | 24 (80) | |
| Hepatic‐bile‐pancreatic | 14 (22.6) | 48 (77.4) | |
| Gastrointestinal | 15 (18.3) | 67 (81.7) | |
| Genitourinary | 11 (13.4) | 71 (86.6) | |
| Breast | 3 (10.5) | 26 (89.5) | |
| Skin (melanoma) | 1 (14.3) | 6 (85.7) | |
| Pulmonary | 20 (18.5) | 88 (81.5) | |
| Head and neck | 2 (10) | 18 (90) | |
| Other | 1 (16.7) | 5 (83.3) | |
| Sedation | 0 (0) | 3 (100) | .630 |
| Fractures | 2 (11.1) | 16 (88.9) | .498 |
| Obligatory position | 12 (15) | 68 (85) | .365 |
| State of consciousness | 2 (11.1) | 16 (88.9) | .486 |
| Cachexia | |||
| BMI 18.5‐24.9 | 45 (17.9) | 207 (82.1) | 2.697 |
| Weight loss >/< 20% | 27 (19.4) | 112 (80.6) | |
| Weight loss >/< 30% | 4 (8.9) | 41 (91.1) | |
| Dyspnoea | 18 (13.9) | 112 (86.1) | 1.516 |
| Lotion | 23 (15.4) | 126 (84.6) | .554 |
| Mattresses | |||
| Polyurethane foam mattresses | 46 (19.9) | 195 (80.1) |
1.374 |
| Dynamic air pressure‐relieving mattresses | 24 (15.1) | 135 (84.9) | |
| Other types of mattresses | 5 (13.9) | 31 (86.1) | |
Table 5.
Patients with/without pressure ulcers (PUs) at the moment of admission
| PU developed | No PU developed | ||
|---|---|---|---|
| n (%) | P (Test chi2) | ||
| Patients without PUs at the moment of admission who developed a PU during stay | 61/327 (18.6%) | 266/ 327 (81.4%) | .204 |
| Patients with PUs at the moment of admission who developed a PU during stay | 15/112 (13.4%) | 97/112 (86.7%) | |
12. RISK FACTORS THAT INFLUENCE THE PRIMARY OUTCOME
In the analysis (Table 6), we have noticed that the age was significantly higher in the group that developed a PU during the stay in hospice. The mean age was 76.4 years in the group that developed a PU and was 73.1 years in the group that did not develop a PU (P = .039).
Table 6.
Variables that influence the onset of new pressure ulcer (PU) (univariate analysis)
| PU developed (=76) | No PU developed (=364) | ||
|---|---|---|---|
| ‐ | Media (ds) | P (t‐test) | |
| Age | 76.4 (10.5) | 73.2 (12.9) | .002 |
| Days of recovery | 21.5 (16.7) | 13 (13.6) | .000 |
| ‐ | n (%) | P (Test chi2) | |
| Discharged because of death | 63 (21) | 237 (79) | 8.7 |
| Incontinence pad | 34 (13.4) | 219 (86.6) | 6.26 |
The study has evidenced that patients who ended up dying in hospice were more likely to develop a PU, 63 patients (21%) out of the 300 patients who died during their stay, developed a PU, where only 13 (9.5%) out of 137 patients who were discharged, developed a PU (P = .003). The reason could be found in the advanced illness of the patient. The proximity of death leads to physical deterioration, and in this phase, the patients often desire to be left undisturbed, not to be mobilised or they have specific needs to be mobilised in one specific position which makes the prevention of PUs difficult.
The length of stay in Hospice influences the incidence of PUs in a negative way: the longer the patient stays in Hospice the higher the risk of contracting a PU. The mean stay in the patients who developed a PU was 25.6 days with the range of 1 to 94. As a matter of fact this group had in media a 7.5 days longer stay in hospice than the patients who did not develop a PU (P = .0001). Presumably clinical deterioration facilitates the development of PUs.
Another risk factor that could influence the occurrence of PUs is the use of Incontinence pads. The incontinence pads seems to have a protective function when it comes to prevent the development of PUs. This could be caused by a more accurate attention when it comes to changing the pads frequently; therefore, this group of patients is more carefully observed during the daily care activities. However, it would be necessary to know if the patient has a urinary catheter and an incontinence pad or only the incontinence pad. In case the patient only has a urinary catheter, the incontinence pad remains dry, and where the patient has only the incontinence pad, one must assume that the incontinence pad frequently is moisture (Tables 6 and 7).
Table 7.
Multivariated logistic analysis
| Odds ratio (OR) | Confidence interval (CI) 95% | P | |
|---|---|---|---|
| Age | 1.04 | 1‐1.07 | .002 |
| Days in hospice | 1.04 | 1‐1.06 | 0 |
| Death (terminal phase) | 2.7 | 1‐5.06 | .003 |
| Incontinence pads | 0.3 | 0.2‐0.7 | .001 |
We are aware that the lack of this information could be evaluated as a confounding factor that could alter the result. It would have been relevant to collect this data. The moisture variable is collected through the Braden Scale but is not accurate and precise enough.
13. INCIDENCE AND CHARACTERISTICS OF KENNEDY TERMINAL ULCERS
Of 440 patients, 12 (2.7%) developed a Kennedy Terminal Ulcer (KTU). The KTU's developed on average 2, 25 (DS 1.2) days before the moment of death.
Seventy‐five percentage of the KTU's were situated on the sacrum, 17% on the heels, and 8% on the trochanter. Fifty percentage of the KTU's were pear shaped, 33.3% were horseshoe shaped, and 16.7% were butterfly shaped. A total of 33.3% of the Kennedy Terminal Ulcers were red, 33.3% were black, and 33.3% were purple.
14. DISCUSSION/CONCLUSION
The occurrence of PUs in the population admitted to hospices is often, according to literature, combined with pain, odour, and important discomfort, and they have a considerable impact on the patient's quality of life. The PUs are quality indicators of the care provided and have high economic costs for the health system. To prevent PUs and to maintain a stable condition of the PUs already developed, represent an important challenge in the PC setting because of the certain clinical deterioration in cancer patients in the advanced phase.4, 7, 10, 13, 14, 15
This study measured the incidence and the prevalence of PUs in patients with a cancer diagnosis in an advanced phase of illness in five hospices in Italy. Furthermore, the risk factors that could have an effect on the development of PUs were studied. In closing, the incidence of Kennedy Terminal Ulcers was measured.
The initial estimated size of population was around 800 patients, but the procedure of a prospective observational study requests an informed consent signed by the patient. This led to exclude non‐competent patients. This means that 500 patients of the entire population were not enrolled. Possibly this group was more at risk than the patients who were capable of signing the informed consent. Further research is needed in this area, including retrospective observational studies or prospective observational studies where acceptance of informed consent from family members or a person with a trustee mandate is allowed.
The study demonstrates that the point prevalence of PUs at the time of enrolment was 112/439 (25.5%). The incidence of pressure ulcers was 76/440 (17.3%). In addition, the Periodic Prevalence was 188/440 (42.8%).
In this study the classical risk factors (pain, cachexia, state of consciousness, dyspnoea at the moment of entrance, pathological fractures at the entrance and moisture, mobilisation, friction and shear, activity, nutrition as described in the Braden Scale) and means of prevention (incontinence pads, skin lotions, mattresses) seems to have less bearing than expected (Table 4).
Quite surprisingly the alternating pressure mattresses versus the polyurethane mattresses (anti pressure ulcer mattresses) did not demonstrate significant differences. Patients using both types of mattresses were likely to develop PUs.
The Braden Scale, that normally indicates the risk of contracting a pressure ulcer, resulted to be a non‐significant variable. The Braden Scale score was the same (mediana 15.5) in patients who developed a new PU and in patients who did not develop a new PU (mediana 15.5).
Pain resulted as a non‐significant variable. The mean score on the NRS Scale in the patients who developed a PU was 1.25 (SD 2.4) with a range from 0 to 10 and the mean score for the patients who did not develop a PU was 1.22 (SD 2.2). Only one patient scored 1 with the Painad score (range 0‐1).
On the other hand we found that age, type of discharge (death), length of stay were risk factors that had a negative influence on the risk of contracting a PU.
The mean age in the group that developed a new PU was 76.4 years so it was significantly higher in this group compared with the group that did not develop a new PU where the age was 73.1 years.
The patients who developed a PU in hospice had a mean stay of 25.6 days with a range from 1 to 94 days which was significantly higher compared with the group that did not develop a new PU where the mean was 16.5 days. The length of stay influenced the incidence of PUs in a negative way which means that the longer the patient stayed in hospice the higher was the risk of contracting a PU, and patients who ended up dying in hospice were even more likely to develop a PU. The reason for this could probably be found in the clinical deterioration that the patients undergo through the last days/weeks of life (Tables 6 and 7).
As said before the incidence in this study was 76/440 (17.3%). We cannot modify the risk factors; age, proximity to death (type of discharge) and length of stay to prevent PUs in this setting but it is interesting that only 15/76 (13.4%) patients who already had a PU at the moment of admission developed a new PU versus 61/76 (18.7%) who did not. A mayor attention in the daily care activities to the patients that did not have a PU at the moment of admission may be relevant in this setting.
The foundation of PC is to respect the patient's will and wishes, find solutions together with the patients that benefits. When it comes to prevention, the choices that are made are not necessarily always according to the recommendations of the guidelines. Could a more specific set of guidelines for this setting be relevant?
15. KENNEDY TERMINAL ULCER
Furthermore, we wanted to measure the incidence of the Kennedy Terminal Ulcer. Twelve patients (2.7%) in this study developed a KTU in the end of the life phase (2.25 days before death). It is an interesting phenomenon because it could be used as a prognostic indicator of how close the patients are to the moment of death. However, the incidence of KTUs in the study was low. Further studies are recommended as it is discussed insufficiently in literature because of the lack of data.
CONFLICTS OF INTEREST
The author/s declare/s that there is no conflict of interest. No competing financial interests exist.
ACKNOWLEDGEMENTS
The authors thank the following investigators who participated in this study: to the staff of Hospice of Savignano Sul Rubicone (FC), Hospice of Forlimpopoli (FC), Hospice of Dovadola (FC), Hospice of Faenza (RA), and Hospice of Lugo (RA), Ufficio Ricerca Clinica e Organizzativa Staff Direzione Sanitaria Rimini Ausl della Romagna and Unità Biostatistica e Sperimentazioni Cliniche of Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori (I.R.S.T.) S.r.l. Sede legale: 47014 Meldola (FC) Via Piero Maroncelli, 40.
Jakobsen Tina Bull Tafteberg, Pittureri C, Seganti P, et al. Incidence and prevalence of pressure ulcers in cancer patients admitted to hospice: A multicentre prospective cohort study. Int Wound J. 2020;17:641–649. 10.1111/iwj.13317
This protocol ‘LESHOSPICE’ with the reference n. 3778/2016 has been approved by the Ethics Comity of Romagna (Comitato Etico Unico IRST e di Area Vasta Romagna)Via Piero Maroncelli, 40, 47014 Meldola (FC), Italy, on the June 20, 2016 and the protocol ‘LESHOSPICE’ n. 1645 has obtained the authorisation to conduct the study on the July 13, 2016 by the Azienda USL della Romagna, Piazza Leonardo Sciascia, 111, 47521 Cesena (FC), Italy. All participants in this study have signed consent form. All authors have signed a consent form.
REFERENCES
- 1. Alvarez OM, Kalinski C, Nusbaum J, et al. Incorporating wound healing strategies to improve palliation (symptom management) in patients with chronic wounds. J Palliat Med. 2007. Oct;10(5):1161‐1189. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO) . www.who.int/cancer/palliative/definition/en/. Accessed February 14, 2019.
- 3. Cartabelotta A, Peghetti A. Linea guida per la prevenzione e trattamento delle lesioni da pressione nelle cure primarie e in ospedale. Evidence open access journal published by the GIMBE Foundation. Giugnio. 2014;6(5):p1‐p5. [Google Scholar]
- 4. Langemo DK, Black J. The National Pressure Ulcer Advisory Panel. Pressure ulcers in individuals receiving palliative care: a National Pressure Advisory Panel White Paper. Adv Skin Wound Care. 2010;23(2):59‐70. [DOI] [PubMed] [Google Scholar]
- 5. Langemo DK. General principles and approaches to wound prevention and care at end of life: an overview. Ostomy Wound Manage. 2012;58(5):24 ‐6, 28, 30. [PubMed] [Google Scholar]
- 6. Reifsnyder J. Development of pressure ulcers in patients receiving home hospice care. Wounds J. 2005;17(4):74‐79. [Google Scholar]
- 7. Hendrichova I, Castelli M, Mastroianni C, et al. Pressure ulcers in cancer palliative care patients. J Palliat Med. 2010;24(7):669‐673. [DOI] [PubMed] [Google Scholar]
- 8. Moore Z, Johanssen E, Van Etten M. A review of PU prevalence and incidence across Scandinavia, Iceland and Ireland (part 1). J Wound Care. 2013;22(7):361‐368. [DOI] [PubMed] [Google Scholar]
- 9. Miner KJ. Discharge to hospice: a Kennedy terminal ulcer case report. J Am Col Certif Wound Spec. 2009;1(3):84‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joyce M, Black JM, Edsberg L, Baharestani MM, Langemo DK, Goldberg M, McNichol L, Cuddingan J, The NPUAP Panel . Pressure ulcers: avoidable or unavoidable? Results of the National Pressure Ulcer Advisory Panel Consensus Conference; February 2011; 57(2): 1‐7. [PubMed]
- 11. Kennedy KL. LLC. Welcome to Kennedy Terminal Ulcer.com Available at www.kennedyterminalulcer.com. Accessed February 21, 2019.
- 12. Vera R. Literature review of Kennedy terminal ulcers: identification, diagnosis. Nursing Goals, and Interventions. 2014; Honors thesis. 24; 5‐17. [Google Scholar]
- 13. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel . Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Washington, DC: National Pressure Advisory Panel; 2009. http://www.npuap.org/now-available-new-2014-international-pressure-ulcer-guidelines/2014. Accessed February 21, 2019. [Google Scholar]
- 14. Galvin J. An audit of pressure ulcer incidence in a palliative care setting. Int JPalliat Nurs. 2002;8(5):214‐221. [DOI] [PubMed] [Google Scholar]
- 15. Maida V, Corbo M, Dolzhykov M, Ennis M, Irani S, Trozzolo L. Wounds in advanced illness: a prevalence and incidence study based on a prospective case series. Int Wound J. 2008;5(2):305‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]


