Abstract
Brochures are a useful supplement to patient education. There is increasing evidence that they are an effective medium to support patient satisfaction, adherence, and empowerment. This study aims to produce reliable data on how much patients with venous leg ulcer (VLU) may profit from a brochure that focuses on VLU and on measures and aims of the related compression therapy. The evaluation took part from October 2018 until March 2019 and included 136 patients with VLU and related compression therapy. They were randomly sorted into a case group and a control group of 68 patients each. The case group received a brochure about venous disease and compression therapy and filled in a questionnaire after reading. The questions ranged from basic knowledge about VLU and compression therapy to aspects of self‐care. The control group answered the same questions without previous reading of the brochure. The results show that in almost every aspect, the patients in the case group were better informed about their diseases, the compression therapy, and how they may support the measures adequately. This study suggests that patients with VLU may profit from a brochure that explains their disease and the related compression therapy. Better knowledge and understanding may strengthen their empowerment and adherence.
Keywords: adherence, compression therapy, empowerment, patient education, venous leg ulcer
1. INTRODUCTION
Besides surgical and invasive interventions, compression therapy is a cornerstone in the therapy of patients with venous insufficiency and its consequences such as oedema and venous leg ulcer (VLU).1 Well‐managed compression therapy with adequate and correctly used materials lowers pressure and volume overload in the venous system, reduces pain, and supports wound healing.2 There are several options for the treatment of VLU with compression therapy. Their usage is oriented on to the different phases of therapy. These consecutive phases are called decongestion phase, maintenance phase, and prevention.2 In the initial decongestion phase, the VLU is treated with high‐compression bandaging.2, 3, 4 The most common options are short‐stretch bandages, padding materials, multicomponent systems, and adaptive compression bandages, also known as wrap or velcro compression devices.2, 5, 6 When oedema is widely reduced or gone and the VLU is healing continuously, the maintenance phase starts. Therefore, the treatment switches to ulcer‐stocking systems or medical compression stockings.6, 7, 8 When the VLU is healed, the patients receive medical compression stockings, which often have to be worn for a lifetime to prevent recurrence of VLU.6
In addition, there are two important keys to a successful therapy of VLU. One is adequate handling of compression materials by the professional users based on their up‐to‐date knowledge and experience.9 The second is patient's adherence to therapy and the acceptance of necessary treatment options and interventions.10 The latter includes the correct usage and care of needed compression materials. For hygienic reasons, short‐stretch bandages, as well as adaptive compression bandages and medical compression stockings, should be changed and cleaned daily by using mild or special detergents according to manufacturer's recommendations. The compression materials should dry lying on a laundry rack. Heater or direct sunlight may damage the compression material. Also important is the patient's ability and willingness to use adequate skincare products. The chronic venous insufficiency, as well as friction of the compression materials, may cause skin irritations and pruritus.11 A daily skin care is therefore necessary. Suitable skincare products should be based on water‐in‐oil (W/O) emulsion, which consists of moisturising factors, such as urea or glycerine, and should be mostly free from emulsifiers, perfume additives, and preservatives.11, 12 Compression stockings do not glide well on recently creamed skin. Therefore, skincare products should be evaporated before donning or should be applied in the evening. Additionally, compression therapy develops its main effect only after regular activation of the calf muscle pump through movement.13 Therefore, venous leg sport activities, for example, walking and foot exercises, support the effect of compression therapy.14, 15
To develop an understanding of one's own illness, its developmental mechanisms, and its associated measures, an indication‐specific education is necessary.16, 17 The content should always be based on the individual needs of the patient.18, 19, 20, 21 Patient brochures are a useful supplement to patient education.19, 20, 21 They have been proven to be an effective medium to increase patients' satisfaction and adherence and may contribute to their empowerment.22, 23, 24, 25, 26, 27 There is an agreement that an informed patient can participate constructively as an equal partner to the treatment process.28 Therefore, there is a high demand for brochures addressing patients and their relatives.16 Internationally, several instruments for patient information, mainly leaflets, were examined in studies. Most of them showed to be useful to improve patients' knowledge.22, 23, 24, 25, 26, 29, 30 So far, we have not found any research on brochures on VLU and related compression therapy.
The brochure “Compression therapy—easy and well‐fitting” addresses patients with VLU and related compression therapy.31 The brochure informs about risk factors that may promote venous insufficiency, about options and materials of compression therapy, about why and when compression therapy should be worn, and what the patient may contribute to the therapy. It also provides information about venous sport exercises and skin care. The brochure was created by a society called “Wundzentrum Hamburg” in Hamburg, Germany (Figure 1). Founded in 2002, this charitable society is dedicated to interdisciplinary and interprofessional cooperation in the fields of diagnostics, therapy, and care of people with chronic wounds. Following a self‐imposed principle that the successful treatment of people with chronic wounds requires appropriate collaboration of all occupational groups involved in care, the members organise themselves into working groups to create therapy and treatment standards as well as patient brochures.
Figure 1.
Brochure “Compression therapy—easy and well‐fitting”
This study will provide data on how much patients with VLU and related compression therapy benefit from using the described brochure on patient education. It focuses on the improvement of theoretical knowledge, practical abilities, and related skills‐subjectively and factually.
2. METHODS
2.1. Study design and procedure
The participating medical care facilities were chosen regarding their specification (ambulatory care and medical practices, hospitals, and specialised clinical wound practices) resulting in a non‐randomised sample. All facilities treat patients with VLU, which are the subjects of interest in this study. The inclusion and exclusion criteria are shown in Figure 2 (CONSORT flow chart). The allocation of patients to the case or control group was conducted alternately and therefore randomly.
Figure 2.
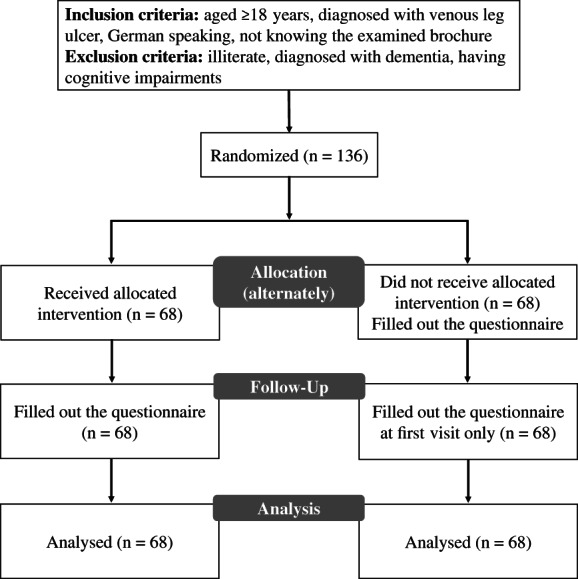
Enrolment
This quasi‐randomised controlled trial was conducted in Germany and Austria between October 2018 and March 2019. All eligible patients attending one of the recruiting centres during the defined period and treatment routine were asked to participate and then divided into two groups: control group and case group. After informed consent was given, the control group received a questionnaire on their theoretical and practical knowledge about VLU and compression therapy as well as related skills. The questionnaire was filled out directly in the facility and handed back to the medical staff. The case group received the brochure “Compression therapy—easy and well‐fitting” after informed consent was given. The patients were asked to read the brochure carefully at home and bring it back with them to their next appointment. They were informed that they would then have to answer a questionnaire, but they did not know that this would be related to the brochure. After returning to the facility, the patients of the case group were asked if and when they had read the brochure. Afterwards, they received the same questionnaire as the control group, completed it immediately, and handed it back to the medical staff. Patients of both groups (control and case group) filled out the standardised questionnaires independently and anonymously. Participation was voluntary and independent of the treatment in the facility. We have chosen the sample size based on methodological aspects as N = 100 (n = 50 in the case group and the control group each), thus allowing for statistical comparisons of the two groups.
All study materials were sent or personally handed out to the study centres. The participating institutions collected the completed questionnaires and sent or handed them back.
2.2. Materials
This survey focused on theoretical knowledge as well as practical knowledge and the related skills of the patients. The data were determined by the patient's self‐assessment and actual knowledge. To check the questionnaire for comprehensibility, in the first step, a pretest with n = 6 participants was performed. In the second step, a cognitive face‐to‐face interview was conducted. Both rounds showed that the developed questionnaire was well understood, so that only a few formulations were adapted. In the third step, the questions were again filled out by two patients independently to assure comprehensibility.
The questionnaire starts with six questions on subjective knowledge of compression therapy, as on theoretical knowledge, practical knowledge, and the abilities concerning compression therapy. These questions were rated on a scale from 1 to 4 (excellent, good, sufficient, and inadequate). The following questions concerned the patients' actual knowledge about compression therapy. The questions were mostly answered by multiple choice. In order to be able to better assess the patients' knowledge, some incorrect options were included. Overall, this part of the questionnaire evaluated the knowledge about the effects of compression therapy, risk factors for venous disease, options of self‐care, skin care, and leg sport activities. Additionally, the patients' usage and care of compression materials and donning devices were examined. The questionnaire ends with the patients' general information on age, gender, and education. Furthermore, the time period of being affected with VLU was queried. Patients of the case group were also asked at which time they had carefully read the brochure.
Besides the brochure and questionnaire, the study material included a letter for the centres with a description of procedure, a patient's information sheet, and an informed consent form with data protection declaration.
2.3. Data protection and ethical guidelines
The requested local ethics committee has decided that no ethics vote is required for this study due to the anonymous, non‐personal data collection.
2.4. Statistical analysis
Analyses were conducted using IBM SPSS Statistics 23 and univariate statistics. Mean, median, and standard deviation are reported for interval scaled items. Frequency distributions and percentages are reported for ordinal and nominal items. Missing data for each item are shown when above 5%, which was not the case for all items. To assess statistical significance of differences between case group and control group, the chi‐square test (Χ 2‐test) and, when more than 20% of the cells had expected counts below five, the Fisher's exact test (FET) were applied (significance level of α = 0.05). For the crosstabs, age (numeric), education (seven answer categories), and wound status (numeric) were categorised (see results). The STROBE and CONSORT guidelines for reporting randomised controlled trials were considered for this publication.
3. RESULTS
Overall, 136 patients (26.5% men, 73.5% women) with a mean age of 71 years (median: 74 years; range: 38–94 years) took part. Half of the patients (n = 68) were in the case group and the other half (n = 68) in the control group. This proportion was also found in the participating medical care facilities. Regarding the age of the patients, there were no significant differences between the two groups (Table 1). A total of 38.2% of the patients were enrolled in specialised clinical wound practice, 36.8% were enrolled in ambulatory care, 20.6% at medical practices, and 4.4% at hospitals (Table 1). Most patients (41.2%) achieved an education that included the 10th grade, of which 41.2% finished school below that grade. A higher education was achieved by 16.9%. There were no significant differences between the case group and control group (Table 1). The duration of VLU was 13.4 months on average (median: 6 months, range: 1–264 months). Case and control groups showed significant (P = .009) differences in VLU duration (case group: mean: 8.5 months; median: 6 months; range: 1–98 months; and control group: mean: 18.3 months; median: 8 months; range: 1–264 months) (Table 1). In the case group, all patients (n = 68) read the brochure “Compression therapy—easy and well‐fitting.” In 85.3% of the cases, the brochure was read in a period of 1 to 13 days and in 14.7% within 3 weeks (14 to 21 days).
Table 1.
Demographics and clinical characteristics of patients with venous leg ulcer
| With brochure, n (%) | Without brochure, n (%) | P | |
|---|---|---|---|
| Age in years: mean/median/SD | 70.9/72.5/12.2 | 71.6/75.0/12.6 | .840 |
| Sex: | |||
| Female | 54 (79.4%) | 46 (67.6%) | .087 |
| Male | 14 (20.6%) | 22 (32.4%) | |
| Graduation: | |||
| Low | 29 (42.6%) | 27 (40.3%) | .848 |
| Middle | 32 (47.1%) | 31 (46.3%) | |
| High | 7(10.3%) | 9 (13.4%) | |
| Treating institution: | |||
| Specialised clinical wound practice | 26 (38.2%) | 26 (38.2%) | 1.000 |
| Outpatient care | 25 (36.8%) | 25 (36.8%) | |
| Hospital | 3 (4.4%) | 3 (4.4%) | |
| Practice (physician) | 14 (20.6%) | 14 (20.6%) | |
| Venous leg ulcer in months of occurrence: | |||
| <7 months | 42 (61.8%) | 27 (39.7%) | .009 |
| 7–12 months | 17 (25.0%) | 18 (26.5%) | |
| >12 months | 9 (13.2%) | 23 (33.8%) | |
| Mean/median/SD | 8.5/6.0/12.5 | 18.3/8.0/36.1 | |
| Total | 68 (100%) | 68 (100%) |
3.1. Estimation of subjective knowledge
The questionnaire started with six questions about venous disease and compression therapy. The patients were asked to estimate their knowledge on a scale from 1 (very good) to 4 (inadequate). The results showed that the subjective knowledge of patients in the control group at least doubled the subjective knowledge of the case group in the value 4 (inadequate) in four of six questions (Table 2). The value 2 (good) was estimated in the case group in any question above the control group (Table 2). The value 1 (very good) was estimated in the control group in five of six items, a little more often than in the case group. In total, the subjective knowledge in the case group was similar or only a bit higher than in the control group. The six questions addressed the function of the veins, the causes of venous diseases, the effects of compression therapy, the products of compression therapy, the cleansing of compression materials, and the awareness about what the patient can contribute to therapy and prevention. Only in the latter case, the difference between the two groups was significant (0.023) (Table 2).
Table 2.
Subjective knowledge of patients with venous leg ulcer about compression therapy
| With brochure, n (%) | Without brochure, n (%) | P | ||
|---|---|---|---|---|
| How well do you estimate your background knowledge about the tasks of veins? | Inadequate | 6 (8.8%) | 13 (19.1%) | .345 |
| Sufficient | 27 (39.7%) | 23 (33.8%) | ||
| Good | 29 (42.6%) | 28 (41.2%) | ||
| Very good | 6 (8.8%) | 4 (5.9%) | ||
| How well are you informed about possible causes of veinal diseases? | Inadequate | 7 (10.3%) | 14 (20.6%) | .357 |
| Sufficient | 27 (39.7%) | 21 (30.9%) | ||
| Good | 28 (41.2%) | 26 (38.2%) | ||
| Very good | 6 (8.8%) | 7 (10.3%) | ||
| How well are you informed about the effects of compression therapy? | Inadequate | 3 (4.4%) | 9 (13.2%) | .106 |
| Sufficient | 18 (26.5%) | 20 (29.4%) | ||
| Good | 36 (52.9%) | 24 (35.3%) | ||
| Very good | 11 (16.2%) | 15 (22.1%) | ||
| How well do you feel informed about the variety of different products for compression therapy? | Inadequate | 6 (8.8%) | 11 (16.2%) | .334 |
| Sufficient | 21 (30.9%) | 20 (29.4%) | ||
| Good | 33 (48.5%) | 25 (36.8%) | ||
| Very good | 8 (11.8%) | 12 (17.6%) | ||
| How would you rate your knowledge about handling of compression materials including material care, for example, cleansing? | Inadequate | 3 (4.4%) | 5 (7.4%) | .471 |
| Sufficient | 19 (27.9%) | 20 (29.4%) | ||
| Good | 36 (52.9%) | 28 (41.2%) | ||
| Very good | 10 (14.7%) | 15 (22.1%) | ||
| How well are you aware about what you can contribute to therapy and prevention? | Inadequate | 1 (1.5%) | 8 (11.8%) | .023 |
| Sufficient | 27 (39.7%) | 17 (25.0%) | ||
| Good | 32 (47.1%) | 29 (42.6%) | ||
| Very good | 8 (11.8%) | 14 (20.6%) | ||
| Total | 68 (100%) | 68 (100%) | ||
3.2. Effects of compression therapy and risks for venous diseases
The patients answered two questions about effects of compression therapy (five items) and risks for venous diseases (six items). Patients in the case group had significantly more knowledge than patients in the control group in most items. For example, with 98.5%, most of them knew that compression therapy improves wound healing, and 56.9% of the control group did not know this (P = .000) (Table 3). An important factor for venous disease is, for example, heredity. This was known by 86.8% in the case group and by 36.8% in the control group (P = .000) (for further answers about the effects of compression therapy and risks for venous diseases, see Table 3).
Table 3.
Effects of compression therapy and the risks for venous diseases
| With brochure, n (%) | Without brochure, n (%) | P | |
|---|---|---|---|
| What are the effects of compression therapy? | |||
| Lean, decongested legs | 68 (100%) | 54 (79.4%) | .000 |
| Pain | 5 (7.4%) | 21 (30.9%) | .000 |
| Restriction of blood circulation | 2 (2.9%) | 4 (5.9%) | .340 |
| Improved wound healing | 67 (98.5%) | 30 (44.1%) | .000 |
| Prevention of reoccurrence of wounds | 55 (80.9%) | 22 (32.4%) | .000 |
| What may increase the risk of developing a venous disease? | |||
| Heredity | 59 (86.8%) | 25 (36.8%) | .000 |
| Sun and warmth | 61 (89.7%) | 33 (48.5%) | .000 |
| Sit often and for long periods | 64 (94.1%) | 46 (67.6%) | .000 |
| Much exercise | 0 (0.0%) | 6 (8.8%) | .014 |
| Underweight | 3 (4.4%) | 5 (7.4%) | .359 |
| Varicose veins | 65 (95.6%) | 42 (61.8%) | .000 |
| Total | 68 (100%) | 68 (100%) |
3.3. Self‐care and vein sport activities
The patients answered two questions about options of self‐care (five items) and vein sport activities (six items). In most items, the patients in the case group had significantly more knowledge than the patients in the control group (Table 4). The case group, for example, knew about the importance of removing cornea of the feet (86.8%) and to shorten the nails regularly (85.3%). These items were rated as not important in the control group (each 83,8%; P = .000) (Table 4). According to the knowledge about vein sport activities, both groups mainly answered correctly. Nevertheless, for each item, a (much) higher percentage of the control group chose the wrong option.
Table 4.
Aspects of self‐care and vein sport activities
| With brochure, n (%) | Without brochure, n (%) | P | ||
|---|---|---|---|---|
| Shower the legs extensively with hot water every day | Yes | 2 (2.9%) | 6 (8.8%) | .215 |
| No | 65 (95.6%) | 62 (91.2%) | ||
| Remove cornea of the feet | Yes | 59 (86.8%) | 11 (16.2%) | .000 |
| No | 8 (11.8%) | 57 (83.8%) | ||
| Rest the legs occasionally above heart level | Yes | 65 (95.6%) | 53 (77.9%) | .002 |
| No | 3 (4.4%) | 15 (22.1%) | ||
| Shorten nails regularly | Yes | 58 (85.3%) | 11 (16.2%) | .000 |
| No | 10 (14.7%) | 57 (83.8%) | ||
| Sit often and rest | Yes | 2 (2.9%) | 21 (30.9%) | .000 |
| No | 66 (97.1%) | 47 (69.1%) | ||
| Climbing stairs | Yes | 61 (89.7%) | 36 (52.9%) | .000 |
| No | 7 (10.3%) | 32 (47.1%) | ||
| Ankle extension and flexion exercises | Yes | 65 (95.6%) | 45 (66.2%) | .000 |
| No | 3 (4.4%) | 23 (33.8%) | ||
| Push‐ups | Yes | 0 (0.0%) | 3 (4.4%) | .133 |
| No | 67 (98.5%) | 65 (95.6%) | ||
| Walking | Yes | 68 (100%) | 46 (67.6%) | .000 |
| No | 0 (0.0%) | 22 (32.4%) | ||
| Tread water | Yes | 55 (80.9%) | 28 (41.2%) | .000 |
| No | 12 (17.6%) | 40 (58.8%) | ||
| Hot baths | Yes | 0 (0.0%) | 1 (1.5%) | .368 |
| No | 67 (98.5%) | 67 (98.5%) | ||
| Total | 68 (100%) | 68 (100%) | ||
3.4. Skin care
The patients answered two questions about their skin care. In the case group, 58.8% preferred correct skincare products based on W/O emulsion with moisturising factors, while the control group chose these products significantly (P = .000) less often (17.6%). Many members of each group specified their choice and/or named their used skincare products. 80% of the case group named urea skin care as the product of their choice, which is recommended. In the control group, 17.1% preferred urea, 22% bag balm, 9.8% baby and olive oil, 9.8% marigold cream, 7.3% Nivea lotion, and 34.1% other products for skin care. The case group performed their skin care, as recommended, in 82.4% of the cases in the evening, while a significantly (P = .000) lower number of 11.8% in the control group chose this point of time. Additionally, 39.7% of patients in the control group used skincare products only when needed (case group 2.9%), while 22.1% used these 1 to 3 times a week (case group 4.4%). The difference between the two groups was significant in any item (P = .000).
3.5. Decongestion phase
In the case and control groups, respectively, 22.1% and 39.7% were treated with short‐stretch bandages (Table 5). When asked how long they would have to wear these, 80% of the case group knew that they need short‐stretch bandages until decongestion. In the control group, a significantly (P = .000) lower part knew this (7.4%), while 51.9% guessed that they would have to wear short‐stretch bandages until their wound healed (for further answers about decongestion phase, see Table 5).
Table 5.
Materials for compression therapy
| With brochure, n (%) | Without brochure, n (%) | P | ||
|---|---|---|---|---|
| What material do you use for your compression therapy? | ||||
| Short‐stretch bandages | Yes | 15 (22.1%) | 27 (39.7%) | .057 |
| No | 52 (76.5%) | 41 (60.3%) | ||
| Multicomponent system | Yes | 14 (20.6%) | 6 (8.8%) | .044 |
| No | 54 (79.4%) | 62 (91.2%) | ||
| Adaptive compression bandage/velcro device | Yes | 4 (5.9%) | 4 (4.4%) | .556 |
| No | 63 (92.6%) | 65 (95.6%) | ||
| Ulcer stocking system | Yes | 17 (25.0%) | 13 (19.1%) | .412 |
| No | 50 (73.5%) | 55 (80.9%) | ||
| Medical compression stocking | Yes | 18 (26.5%) | 19 (27.9%) | .598 |
| No | 49 (72.1%) | 49 (72.1%) | ||
| Do not know | Yes | 0 (0.0%) | 0 (0.0%) | |
| No | 0 (0.0%) | 0 (0.0%) | ||
| Total | 68 (100%) | 68 (100%) | ||
| How long do you have to wear short‐stretch bandages? | ||||
| At least 1 year | 0 (0.0%) | 5 (18.5%) | .000 | |
| For life | 0 (0.0%) | 6 (22.2%) | ||
| Until your leg is decongested | 12 (80.0%) | 2 (7.4%) | ||
| Until your wound is healed | 3 (20.0%) | 14 (51.9%) | ||
| Total | 15 (100%) | 27 (100%) | ||
3.6. Care of compression materials
The cleansing of compression materials showed some significant differences between case and control group. Cleansing was performed daily (recommended) by 41.2% and once a week by 1.5% of the case group, and daily by 11.8% and once a week by 32.4% of the control group (P = .000; Table 6). For cleansing, the compression materials of 50% of the case group used mild detergent (as recommended), 11.8% added fabric softener, and 11.8% used hair shampoo. In contrast, the control group washed their compression materials in 57.4% of cases with mild detergent, 4.4% added fabric softener, and 5.9% used hair shampoo (Table 6). The patients in the case group dried their compression materials as recommended in 57.4% of cases and in the control group in 19.1% of cases by lying it on a laundry rack (P = .000). Furthermore, 30.9% of the control group used the radiator for drying and no patients of the case group did so (for further answers, see Table 6).
Table 6.
Care of compression materials
| With brochure, n (%) | Without brochure, n (%) | P | |
|---|---|---|---|
| How often do you wash your compression materials? | |||
| Not at all | 14 (20.6%) | 6 (8.8%) | .000 |
| Daily | 28 (41.2%) | 8 (11.8%) | |
| Every 2 days | 19 (27.9%) | 12 (17.6%) | |
| Every 3 days | 4 (5.9%) | 16 (23.5%) | |
| Every 4 days | 0 (0.0%) | 3 (4.4%) | |
| Once a week | 1 (1.5%) | 22 (32.4%) | |
| How do you cleanse your compression materials? | |||
| Not at all | 4 (5.9%) | 5 (7.4%) | .755 |
| Washing by hand | 27 (39.7%) | 21 (30.9%) | |
| Machine washing | 26 (38.2%) | 30 (44.1%) | |
| Not applicable | 11 (16.2%) | 12 (17.6%) | |
| With what detergent do you cleanse your compression materials? | |||
| Mild detergent | 34 (50.0%) | 39 (57.4%) | .246 |
| Heavy‐duty detergent | 17 (25.0%) | 12 (17.6%) | .201 |
| Plus fabric softener | 8 (11.8%) | 3 (4.4%) | .104 |
| Hair shampoo | 8 (11.8%) | 4 (5.9%) | .183 |
| Other | 1 (1.5%) | 3 (4.4%) | .310 |
| How do you dry your compression materials? | |||
| Laundry rack, lying | 30 (57.4%) | 13 (19.1%) | .000 |
| Laundry rack, hanging | 14 (20.6%) | 22 (32.4%) | |
| Radiator | 0 (0.0%) | 21 (30.9%) | |
| In the sun | 0 (0.0%) | 6 (8.8%) | |
| Other | 1 (1.5%) | 0 (0.0%) | |
| Not applicable | 14 (20.6%) | 6 (8.8%) | |
| Total | 68 (100%) | 68 (100%) |
3.7. Donning devices
The comparison of the case and control groups showed significant differences (P = .000) in the knowledge about donning devices for the easier usage of medical compression stockings. In the case group, 73.5% knew sliders and 63.2% metal frame devices, while 23.5% of the control group knew sliders and 8.8% metal frame devices.
4. DISCUSSION
Patient brochures are known to be a useful addition to patient education.20 They have proven to be effective in increasing patient's satisfaction and adherence and may contribute to the empowerment of patients.23, 27 The results of our research support these assumptions. All in all, it was found that the majority of respondents in the case group clearly benefited from the brochure “Compression therapy—easy and well‐fitting.” The patients were asked and agreed to participate without knowing if they would enter the case group or the control group. Therefore, there is no bias between the two groups. Generally, it can be assumed that patients, who are interested in and want to receive information, are more willing to participate in a study like this. As the patients in the case group knew that they would have to complete a questionnaire at their next appointment, they may have read the brochure particularly carefully.
In the introductory self‐assessment of the knowledge on therapy and disease, the control group considered to be more often “very good” informed than the case group in five of the six aspects. This may be because the brochure helps to understand that the subject is more complex than previously assumed. In addition, it can be concluded that one's own experiences may be questioned when reading a brochure that is adapted to the disease and therapy. In the examination of the questions about the content of the brochure, significant differences in current knowledge between the case and control groups could be observed in most of the cases. The questions about the effects of compression therapy showed that the control group was less or even misinformed. They thought that compression could cause pain in 30.9% (case group, 7.4%), while 55.9% (case group, 1.5%) did not know that it improves wound healing and 67.6% did not know that it prevents recurrence (case group, 19.1%). These results show that education helps patients to understand how necessary measures, in this case compression therapy, are related to therapy goals. If patients recognise such connections, adherence to the measures may increase as a result.
Correctly performed self‐care measures support the success of the therapy. More patients of the case group knew that it is important to remove cornea of the feet and to shorten their nails regularly. These measures help to protect the stocking material. The German healthcare system reimburses only one pair of medical compression stockings every 6 months. Therefore, it is crucial to keep them intact by correct usage and care. In addition, incorrect care has a damaging effect on the material qualities and may therefore reduce the effectiveness of the stockings.
Regarding the use of the appropriate detergent for compression materials, the knowledge in the control group was surprisingly slightly better. They used a mild detergent more often and chose more seldom wrong options, such as heavy‐duty detergent and hair shampoo. This was the only topic where the control group was better informed than the case group. This information is prominently presented in the brochure though in a somewhat text‐heavy section, which may explain the outcome (see below). The difference is not significant like in most of the other topics. The information about correct drying of the compression materials settled well in the case group. Only 19.1% of the control group mentioned to dry the materials lying on a laundry rack (case group: 57.4%), 30.9% dried them on a radiator (case group: 0%), and 8.8% in the sun (case group: 0%). The wrong drying method may also cause damage to the compression materials. The use of donning devices can also protect the stocking material, ease the handling, and support the self‐management of the patients.15 Nearly all patients in the case group knew about donning devices, while not even half of the control group was informed about them. In this case, the study showed a significant (P = .000) difference between the two groups.
Regular adequate cleansing of compression materials prevents hygienic complications that can cause skin irritations. The control group washed their materials mostly daily or every 2 days, while most of the control group did this every 3 to 7 days. The friction of the compression materials can additionally irritate the skin. Therefore, it has to be cared with adequate skincare products, for example, with urea (case group: 80%). The skin care in the control group was not adjusted appropriately because 83% used the products (eg, baby oil, Nivea lotion/cream, marigold cream, bag balm) with preservatives, perfumes, and emulsifiers, in particular lanolin, that have an increased sensitising potential especially for patients with venous insufficiency.11, 12 Although a large part of the case group performed skin care every evening, 61.8% of the control group did this only 1 to 3 times a week or as needed. Adequate skin care should be a daily routine for patients with venous insufficiency to protect skin irritations and limiting pruritus.
Compression therapy develops its main effects only when the muscle pumps are activated. Therefore, patients are advised to perform regular foot gymnastics and gait training.14 The case group showed significantly more knowledge about vein sport activities.
In both groups, patients were treated with short‐stretch bandages. These have to be worn until successful decongestion of the leg. Compared with short‐stretch bandages, medical compression stockings secure the pressure over a period of several weeks and achieve a better adherence to therapy.32 Therefore, therapy should be changed from short‐stretch bandages to stockings as soon as the decongestion of the leg is completed. In the control group, most of the patients thought that they have to wear short‐stretch bandages until their wound is healed or at least for 1 year. The case group profited obviously from the brochure because most (80%) knew the correct answer.
It would be an interesting topic for further studies for how long the effect from reading the brochure is present and whether it has any effects on the course of disease. Because the VLU should be healed within a period of 3 to 6 months, it would be very difficult to reach a sufficient proportion of the participating patients after this time.
5. LIMITATIONS
In total, the results show that patients may profit from a brochure. The brochure used in this study has been produced according to certain criteria, for example, targeted group and specified aim, personal approach, adequate font size and layout, corresponding line spacing, informative illustrations, information to author references, and understandable language.16, 20 This may be a limiting factor because our results may not be transferable to other brochures. This study was performed in Germany and Austria by using a brochure in the German language. It would be conceivable to apply the brochure in other languages after it has been translated.
As shown in our study, one aspect, the correct usage of detergent, was not known better by the case group. This aspect was explained in a somewhat text‐heavy section of the brochure. Maybe with an additional explaining communication, there would have been a better outcome. This indicates that the sole use of brochures should be viewed critically. Ideally, it is used to support an educational situation with the patient. The patient should have the opportunity to ask questions after reading in order to prevent incomprehension and possible resulting rejection.16 It may also strengthen empowerment and self‐management of the patient. The significant difference in wound duration between case and control groups may be another limiting factor. The patients in the control group had a much longer duration of VLU than the patients in the case group, and 33.8% had their VLU over 12 months (case group: 13.2%). It can be assumed that with a longer presence of the VLU, therapy measures and causes of the illness would have to be known better. This may be false knowledge that can endanger the therapy if not corrected. This astonishing result supports the assumption that reading an adequate brochure leads to more understanding and correct knowledge about these measures. As described earlier, knowledge can support patient's adherence and thus lead to the success of the therapy. Our study aimed to examine the improvement in patient's knowledge and gives no direct insights regarding patient's adherence or even clinical improvements.
5.1. Practical implications
A prerequisite for successful compression therapy is the patient's understanding of an agreement on the associated measures. An informative brochure, adapted to the patient's needs, can help to strengthen adherence, to improve empowerment, and thus to improve healing of VLU. In addition, such brochures can support education by medical and nursing personnel by complementing a personal educational conversation. The use of such a brochure can also lead to time saving with regard to the care process, as the patient independently acquires reliable knowledge.
ACKNOWLEDGEMENTS
The authors thank Sabine Ahrendt and Mario Gehoff who are part of the scientific communication team of the IVDP for copy‐editing.
Protz K, Dissemond J, Seifert M, et al. Education in people with venous leg ulcers based on a brochure about compression therapy: A quasi‐randomised controlled trial. Int Wound J. 2019;16:1252–1262. 10.1111/iwj.13172
REFERENCES
- 1. Partsch H, Mortimer P. Compression for leg wounds. Br J Dermatol. 2015;173(2):359‐369. [DOI] [PubMed] [Google Scholar]
- 2. Dissemond J, Eder S, Läuchli S, Partsch H, Stücker M, Vanscheidt W. Compression therapy of venous leg ulcers in the decongestion phase. Med Klin Intensivmed Notfmed. 2018;113(7):552‐559. [DOI] [PubMed] [Google Scholar]
- 3. Amsler F, Willenberg T, Blättler W. In search of optimal compression therapy for venous leg ulcers: a meta‐analysis of studies comparing divers bandages with specifically designed stockings. J Vasc Surg. 2009;50(3):668‐674. [DOI] [PubMed] [Google Scholar]
- 4. Mosti G. Kompressionstherapie bei Veneninsuffizienz und arteriellen Erkrankungen. Phlebologie. 2014;43(03):127‐133. [Google Scholar]
- 5. Dissemond J, Protz K, Hug J, Reich‐Schupke S, Kröger K. Compression therapy of chronic leg ulcers: practical aspects. Z Gerontol Geriatr. 2018;51(7):797‐804. [DOI] [PubMed] [Google Scholar]
- 6. Dissemond J, Protz K, Reich‐Schupke S, Stücker M, Kröger K. Compression therapy in leg ulcers. Hautarzt. 2016;67(4):311‐323. [DOI] [PubMed] [Google Scholar]
- 7. O'Donnell TF, Passman MA, Marston WA, et al. (2014) management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2014;60(2):3S‐59S. [DOI] [PubMed] [Google Scholar]
- 8. Stücker M, Altmeyer P, Reich‐Schupke S. Therapy of venous leg ulcers. New and established approaches. Hautarzt. 2011;62(7):504‐508. [DOI] [PubMed] [Google Scholar]
- 9. Heyer K, Protz K, Augustin M. Compression therapy—cross‐sectional observational survey about knowledge and practical treatment of specialised and non‐specialised nurses and therapists. Int Wound J. 2017;14(6):1148‐1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weller CD, Buchbinder R, Johnston RV. Interventions for helping people adhere to compression treatments for venous leg ulceration. Cochrane Database Syst Rev. 2016;(3):CD008378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geier J, Erfurt‐Berge C, Mahler V. Hautpflege bei chronisch venöser Insuffizienz. Phlebologie. 2018;4(47):199‐204. [Google Scholar]
- 12. Wohlrab J. Topical preparations and their use in dermatology. J Dtsch Dermatol Ges. 2016;14(11):1061‐1070. [DOI] [PubMed] [Google Scholar]
- 13. Rabe E, Földi E, Gerlach H, et al. Leitlinie: Medizinische Kompressionstherapie der Extremitäten mit Medizinischem Kompressionsstrumpf (MKS), Phlebologischem Kompressionsverband (PKV) und Medizinischen adaptiven Kompressionssystemen (MAK). AWMF‐Registernummer: 037/005. 2018. https://www.awmf.org/uploads/tx_szleitlinien/037‐005l_S3k_Medizinische‐Kompressionstherapie‐MKS‐PKV_2019‐05.pdf
- 14. Klyscz T, Jünger M, Zuder D, et al. Verbesserung der kutanen Mikrozirkulation bei der chronischen Veneninsuffizienz (CVI) durch ein sportmedizinisches Bewegungsprogramm. Akt Dermatol. 1997;23:248‐251. [Google Scholar]
- 15. Protz K, Heyer K, Dissemond J, et al. Compression therapy ‐ current practice of care: level of knowledge in patients with venous leg ulcers. J Dtsch Dermatol Ges. 2016;14(12):1273‐1283. [DOI] [PubMed] [Google Scholar]
- 16. Protz K, Verheyen‐Cronau I, Heyer K. Broschüren zur Unterstützung der Patientenedukation in den Themenbereichen MRSA, Kompression und Wundwissen – Eine Untersuchung anhand der Veröffentlichungen des Wundzentrum Hamburg e. Pflegewissenschaft. 2013;15(12):658‐678. [Google Scholar]
- 17. Moscicka P, Szewczyk MT, Jawien A, Cierzniakowska K, Cwajda‐Białasik J. Subjective and objective assessment of patients' compression therapy skills as a predicator of ulcer recurrence. J Clin Nurs. 2016;25(13–14):1969‐1976. [DOI] [PubMed] [Google Scholar]
- 18. Andriessen A, Apelqvist J, Mosti G, Partsch H, Gonska C, Abel M. Compression therapy for venous leg ulcers: risk factors for adverse events and complications, contraindications – a review of present guidelines. J Eur Acad Dermatol Venereol. 2017;31(9):1562‐1568. [DOI] [PubMed] [Google Scholar]
- 19. Protz K. Richtig schulen. Pflegezeitschrift. 2014;67(6):342‐347. [PubMed] [Google Scholar]
- 20. Zegelin A. Information, Schulung, Beratung und Anleitung. In: Menche N, ed. Pflege heute (7th ed.). München: Urban & Fischer, 2019:1220‐1235. [Google Scholar]
- 21. Hossieny P, Smith RC, Yates P, Carroll G. Efficacy of patient information concerning casts applied post‐fracture. ANZ J Surg. 2012;82:151‐155. [DOI] [PubMed] [Google Scholar]
- 22. Kenny T, Wilson RG, Purves IN, Clark J, Newton DP, Moseley DV. A PIL for every ill? Patient information leaflets (PILs): a review of past, present and future use. Fam Pract. 1998;15:471‐479. [DOI] [PubMed] [Google Scholar]
- 23. Merle V, Marini H, Rongere J. Does an information leaflet about surgical site infection (SSI) improve recollection of information and satisfaction of patients? A randomized trial in patients scheduled for digestive surgery. World J Surg. 2011;35:1202‐1211. [DOI] [PubMed] [Google Scholar]
- 24. Dixon‐Woods M. Writing wrongs? An analysis of published discourses about the use of patient information leaflets. Soc Sci Med. 2001;52:1417‐1432. [DOI] [PubMed] [Google Scholar]
- 25. Akkuzu G, Arslantaş S, Kosker SB, Sen S. Evaluation by patients and caregivers of the effectiveness of a brochure developed to prevent pressure ulcers. J Wound Ostomy Continence Nurs. 2009;36(6):610‐615. [DOI] [PubMed] [Google Scholar]
- 26. Johnson A, Sandfort J, Tyndall J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database Syst Rev. 2003;4:CD003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. National Health and Medical Research Council . How to Present the Evidence of Consumers. Canberra: Preparation of Consumer Publications. Commonwealth of Australia; 2000. [Google Scholar]
- 28. Corbett LQ, Ennis WJ. What do patients want? Patient preference in wound care. Adv Wound Care (New Rochelle). 2014;3(8):537‐543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bobridge A, Sandison S, Paterson J, Puckridge P, Esplin M. A pilot study of the development and implementation of a 'best practice' patient information booklet for patients with chronic venous insufficiency. Phlebology. 2011;26(8):338‐343. [DOI] [PubMed] [Google Scholar]
- 30. Hartigan I, Murphy S, Hickey M. Older adults' knowledge of pressure ulcer prevention: a prospective quasi‐experimental study. Int J Older People Nurs. 2012;7(3):208‐218. [DOI] [PubMed] [Google Scholar]
- 31.Wundzentrum Hamburg. Kompressionstherapie einfach – tragbar. Informationen für Betroffene und Angehörige. 2018. www.wundzentrum‐hamburg.de/uploads/media/Patientenbroschuere_Kompression_2018.pdf.
- 32. Kahle B, Hermanns H‐J, Gallenkemper G. Evidenzbasierte Therapie chronischer Beinulzera. Dtsch Arztebl Int. 2011;108(14):231‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]


