Abstract
The prevalence of chronic wounds in the Helsinki metropolitan area in 2008 was investigated. Thereafter, a specialised wound care team was founded as part of the City of Helsinki Health Services, aiming for early diagnoses of chronic wounds. In the current study, we have repeated the prevalence study to analyse the changes in the prevalence of chronic wounds. A questionnaire on wound patients was sent to all units of social and health care in the Helsinki metropolitan area. We asked about the number of patients with wounds treated during a 24‐hour period, as well the aetiology and location of the wounds. A total of 911 patients had, altogether, 1021 wounds. Thus, prevalence was 0.08%. Pressure and multifactorial ulcers were the most common aetiological groups, whereas wound without defined aetiology had diminished greatly (61%) The prevalence of chronic wound decreased when compared with 2008 (0.08% vs 0.1%). The number of elderly people aged over 65 years had increased 35%, and the age‐adjusted prevalence had decreased. Wounds are treated mostly in primary care units and as outpatients. Therefore, the following conclusion may be reached: diagnostic process and implementation of treatment paths are strengthened within primary care units, yet prevalence of wounds has decreased.
Keywords: aetiology, chronic wounds, leg ulcer, prevalence, primary care, treatment pathways
1. INTRODUCTION
Chronic wounds cause substantial health care costs and decrease the quality of life.1 This is partially because of the fact that there is a lack of a diagnostic process in public wound care. Vowden et al reported that 41% of patients suffering from arterial ulcers and treated in the community did not receive specialist services. Of all the wounds with unknown aetiology, the vast majority (93%) was treated at primary care units.2 When there is a delay in diagnosis, the entire treatment process is delayed, causing additional costs and individual suffering.
According to the Finnish national registry maintained by the National Institute for Health and Welfare, a wound was coded as the patient's diagnosis in 13% of the primary health care outpatient visits (36 100 out of 267 800 nurse's appointments).3 This means roughly 99 visits per day per one million inhabitants. “Wounds” was the third biggest group after “routine health checks” (139/day/1 million inhabitants) and “acute upper respiratory infections” (99/day/1 million inhabitants). It has been estimated that, in the Helsinki metropolitan area, the treatment of wounds costs approximately 7 to 14 million euros per year.4 The estimated wound care costs in the United Kingdom during 2012 to 2013 were 4.5 to 5.1 billion pounds per year, roughly the same as the costs of obesity (5.0 billion pounds per year).5
Systematic studies on the prevalence of chronic wounds at the national or population level are scarce. The epidemiological challenge is the heterogeneity of the studies, which makes them difficult to compare.6
In 2008, the prevalence of chronic wounds was studied in the Helsinki metropolitan area.7 The prevalence of chronic wounds in the region was 0.10%7. Since that study, efforts to strengthen primary care have been made. A wound care team in primary care was established in Helsinki in 2013. The team includes a general practitioner (GP) educated in chronic wounds, three wound care nurses, and a part‐time podiatrist. This unit is part of the City of Helsinki's primary care health centre network, focusing on the early diagnosis of chronic wounds and the provision of specialist consultations to all the primary care units in the Helsinki area: health centres, home care, and nursing homes.
The aim of the current study was to evaluate the change in the prevalence of chronic wounds and their aetiologies for 8 years in the Helsinki metropolitan area.
2. METHODS
The study evaluated the prevalence of chronic wounds for 1 day at the health care units in the Helsinki metropolitan area. A 1‐day prevalence questionnaire was sent to all social and health care units in the region: health centres, home care units, hospital outpatient clinics, and inpatient wards, as well as nursing homes.
The data collection date was November 30 2016, with the exception of the City of Vantaa, where the date was postponed to January 23 2017 because of organisational problems. In order to increase the response rate, the questionnaire was repeated on April 3 2017 in health centres of Helsinki that did not respond at all on original date.
The electronic questionnaire was sent via email to the supervisors of these units, and they were asked to distribute the questionnaire to the personnel, mainly nurses.
The questionnaire included questions regarding the overall number of patients who had visited or stayed on a ward in the health care unit that day and, specifically, the number of wound patients. Furthermore, we enquired about the location and the aetiology of the wounds. The aetiological factors of the wounds were self‐reported by the personnel of the units. The nurses either found the proper diagnosis (ICD‐10‐code) from patient records, or they defined the aetiology of the wound themselves.
3. RESULTS
The questionnaire was sent to a total of 797 units in the Helsinki metropolitan area, 322 (40.4%) of which responded. The best response rate (78%) was achieved in the City of Helsinki units, whereas no response was received from private clinics and private hospitals.
The overall number of patients visiting health care units for any reason was 12 051, 911 (7.6%) of whom presented with a total of 1021 wounds. The population in the Helsinki metropolitan area (Helsinki, Espoo, Vantaa) was 1 112 615 in 2016, and the prevalence of wounds in the capital area was thus 0.08%. In 2008, 1029 patients had a total of 1192 wounds, the prevalence being 0.10% (P < 0.001).
The trends in the aetiological variance of wounds between the previous study in 2008 and the present study are shown in Table 1.
Table 1.
Wound aetiologies for the years 2008 and 2016
| 2008, % (n) | 2016, % (n) | Spectrum of aetiologies below knee level, 2016, % (n) | |
|---|---|---|---|
| Pressure | 22.6 (269) | 26.0 (265) | 14.6 (89) |
| Diabetic | 11.2 (134) | 10.5 (107) | 15.6 (95) |
| Ischaemic | 7.0 (83) | 8.1 (83) | 12.8 (78) |
| Vena insuff/oedemic | 12.7 (151) | 10.9 (111) | 17.2 (105) |
| Postoperative | 8.9 (106) | 10.1 (103) | 6.1 (37) |
| Post‐traumatic | 11.7 (119) | 10.8 (65) | |
| Multifactorial | 21.2 (253) | 16.5 (168) | 17.1 (104) |
| Vasculitis | 1.3 (13) | 1.8 (11) | |
| Unknown | 13.7 (163) | 5.1 (52) | 4.1 (25) |
| Total | 100.0 (1192) | 100.0 (1021) | 100.0 (609) |
The majority (60%) of the chronic wounds were located below the knee level (Table 2).
Table 2.
Locations of the wounds, % (n)
| Foot/ankle | 37.0 (378) |
| Leg | 22.6 (231) |
| Knee/thigh | 6.5 (66) |
| Body | 19.1 (195) |
| Other | 12.2 (125) |
| Unknown | 2.5 (26) |
| Total | 100 (1021) |
Of all wound patients, 53.1% were treated as outpatients, 21.0% were hospitalised, and 25.9% were living in a nursing home (Table 3). Primary care providers reported 73.9% of all wound patients, indicating that the greatest proportion of wound patients are treated within primary care. One third of the wound patients were treated by home care units (31.2%) (Table 4), although the prevalence of wounds in these units was lower (5.8%) than at health centres or hospitals (10.9% and 17.9% respectively).
Table 3.
Division of wound patients for in‐ and outpatients
| Total area | Wound patients | % | Helsinki City Units | Wound patients | % | |
|---|---|---|---|---|---|---|
| Inpatients | 1156 | 191 | 21.0 | 725 | 127 | 21.6 |
| Outpatients | 6664 | 484 | 53.1 | 4304 | 333 | 56.6 |
| Nursing homes | 4275 | 236 | 25.9 | 3138 | 128 | 21.8 |
| Total | 12 051 | 911 | 100.0 | 8167 | 588 | 100.0 |
Inpatients: hospitalised patients.
Outpatients: health centres, home care, foot therapy, and hospital outpatient clinics.
Nursing homes: assisted living units, widely variating the level of aid needed.
Table 4.
Division of wound patients between institutions in the Helsinki metropolitan area
| Helsinki metropolitan area | Total patient visits | Wound patients | Wound patients in these institutions (%) | Division of wound patients between institutions (%) |
|---|---|---|---|---|
| Nursing homes | 4242 | 236 | 5.6 | 25.9 |
| Home care | 4983 | 290 | 5.8 | 31.8 |
| Health centres | 1485 | 162 | 10.9 | 17.8 |
| Hospitals | 1341 | 223 | 16.6 | 24.5 |
| Total | 12 051 | 911 | 100.0 |
Hospital patients: in‐ and outpatients in the Helsinki University Hospital and the City of Helsinki hospitals.
Health centres: primary care outpatients and foot therapy.
4. DISCUSSION
Chronic wounds cause major health care costs and, at the individual level, a decrease in the quality of life. In 2008, we found that the prevalence of wounds among all patients treated during 1 day in the Helsinki metropolitan area was 0.10%. In the current study, we repeated the previous questionnaire to study the 1‐day point prevalence with the same questionnaire formula and the same population area. The prevalence in 2016 was slightly lower compared with the prevalence in the previous 8 years, being 0.08%. Considering the fact that the number of patients aged over 65 years had increased by 35.1% over the 8‐year interval, the age‐adjusted prevalence had decreased rather than increased.
The Finnish population is aging,8 and this reflects the prevalence and incidence of wound patients. Wound healing is reversely associated with age9. Elderly individuals with chronic diseases and multiple comorbidities have a higher risk of developing non‐healing wounds. Age itself increases not only the risk of developing a wound but also the risk of delayed wound healing. From the age of 60 years onwards, the normal wound‐healing process is abnormal, and in the over 70 years age group, the time to wound healing is 25% slower.9
The limitation of our study was that the response rate was very low in the whole study area (40.4%). However, the numbers of wounds reported were quite similar to those reported in 2008. We assume that the units which did treat wound patients mainly responded but that the response rate was lower for those units that had no wound patients, 25% in 2016 compared with 39% in 2008, the non‐responders therefore lowering the response rate for the entire study area. In the City of Helsinki units, the response rate was fairly high at 78% (Tables 4 and 5).
Table 5.
Division of wound patients only in the City of Helsinki Units
| The City of Helsinki Units | Total of patient visits | Wound patients | Wound patients in these units (%) | Division of wound patients between units (%) |
|---|---|---|---|---|
| Nursing home | 3138 | 128 | 4.1 | 21.8 |
| Home care | 3438 | 206 | 6.0 | 35.0 |
| Health centres | 785 | 119 | 15.2 | 20.2 |
| Hospitals | 806 | 135 | 16.7 | 23.0 |
| Total | 8167 | 588 | 100.0 |
Another limitation is that we only had data on the number of patients, wound location, and aetiology but no information on the patients' age and were therefore unable to calculate the age‐adjusted prevalence.
Practically all of the responding professionals were nurses. This leads to a question concerning the diagnostic process and whether the diagnosis was made by a physician. In primary care, there remains a challenge to involve general practitioners in the treatment process from the beginning to ensure that the aetiological investigations are being taken into account properly despite the wound care team that was established within primary care, aiming to bridge the gap in the treatment paths between primary care nurses and specialist care.
The problem of defining an accurate diagnosis has also been acknowledged in previous studies. A variation of diagnostic methods between specialties was observed in a German study by Körber et al. in 2011, where the authors detected the underlying causes of leg ulcers: venous insufficiency in 47.6%, arterial wounds in 14.5%, and a combination of both in 17.6% of the cases.10 The aetiological spectrum varies according to the health care unit in question, as well as patient mobility, the standard of living, and the location of the wound. A different prevalence of aetiologies is found in different health care units.
The finding by Körber et al was analogous to a study in the Skaraborg County, Sweden, that investigated the spectrum of leg ulcer aetiologies in below‐knee‐level ulcers at a vascular clinic during 1988 and 2002. The diagnoses were as follows: venous incompetence in 31%, arterial insufficiency in 4%, combined vascular aetiology in 25%, diabetic foot ulcer in 8%, a pressure ulcer in 4%, and multifactorial cause in 18% of the cases.10 These results obtained at a specialist clinic are quite different from those of population‐based studies.
Based on the City of Helsinki units' response rate and interventions to strengthen the primary care by establishing a wound care team, we analysed the City of Helsinki as a subgroup. In the City of Helsinki units, there was no change in prevalence (0.09% vs 0.10%; Figure 1). This can reflect better wound care as there is generally a tendency towards increased wound prevalence because of aging and the increased prevalence of diabetes. In addition, compared with the situation in 2008, the proportion of wounds with unknown aetiology had decreased significantly (Table 1). This result shows that the understanding of defining the aetiological factor has increased. The largest aetiological groups were pressure and multifactorial wounds (Table 1). Both multifactorial and post‐traumatic wounds (Figure 1) can be discussed if multiple comorbidities are found to delay the healing of these wounds. Unfortunately, this result emphasises the continued lack of proper implementation despite good evidence and guidelines and the existence of the mentioned wound care team.
Figure 1.
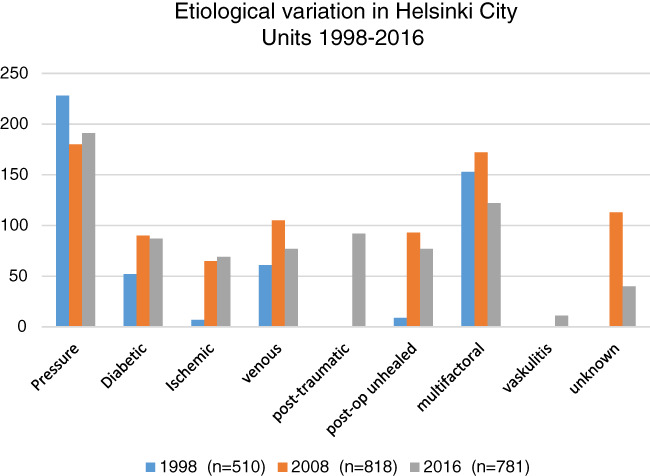
Aetiological variation in Helsinki City Units 1998‐2016
The present study had some similarities with a retrospective study from the United Kingdom5 on wound aetiologies. The data were collected from the The Health Improvement Network database of general practitioners' patient records. The study showed that the annual prevalence of chronic wounds in the United Kingdom was: unspecified leg ulcers 19%, venous leg ulcers 13%, postoperative (over 4 weeks) wounds 11%, diabetic foot ulcers 8%, traumatic wounds 7%, arterial ulcers 1%, and pressure ulcers 7% (only GP's records and no nursing homes included)5
Pressure ulcers are of great significance in the current data. Pressure ulcer was the most common wound aetiology in nursing homes, and the prevalence of pressure ulcers in the present study was high, 26% (n = 1035), which is remarkably higher than in 2008 (23%). This is somewhat surprising as awareness of the importance of decompression has increased. Among hospitalised patients, the rate was 33%, which is again higher than what was found in Finland in 1992 (22%).12
Special attention focuses on nursing homes as pressure ulcers constitute 43% of all chronic ulcers found in the nursing home setting in the present study. A Swedish study13 showed a pressure ulcer prevalence of 16.6% in hospitals and 14.5% in nursing homes in Sweden. It was discussed that, despite the measures taken to combat pressure ulcers, their prevalence rates are high in Europe.13 Although the present study was not performed as recommended by the European Pressure Ulcer Advisory Panel, and therefore, the results are not directly comparable, we can conclude that the prevalence of pressure ulcers in the Helsinki metropolitan area is still too high.
It is notable that the lack of wound registries causes a variety of problems in studies on wound prevalence and incidence. It has been estimated that 60% of chronic ulcers are leg ulcers. In previous studies reviewed, the prevalence of leg ulcers ranged from 0.6% to 3.6% of the population investigated.14 Because of the absence of systematic investigations of wound prevalence, Järbrink et al have introduced a study protocol for a systematic prevalence study on chronic wounds (Järbrink et al).
As wound patients in the Finnish health care system are mainly investigated and treated within primary care, the question is how to implement evidence‐based wound care in primary care by both for GPs and nurses. In the spring of 2018, a wound centre was established at the Helsinki University Hospital. The aim of the wound centre is to develop treatment paths, to create a network of wound specialists in both specialist and primary care, and to offer consultations efficiently. This emphasises the fact that educating primary care personnel and focusing on the implementation of local guidelines improves the diagnostic process of a wound patient.
Ethical consideration: According to Finnish law, there is no need for ethical committee approval with this kind of study protocol. We have obtained approval for a registry study from the Cities in Helsinki metropolitan area and the Helsinki University Hospital.
Ahmajärvi KM, Isoherranen KM, Mäkelä A, Venermo M. A change in the prevalence and the etiological factors of chronic wounds in Helsinki metropolitan area during 2008‐2016. Int Wound J. 2019;16:522–526. 10.1111/iwj.13077
REFERENCES
- 1. Lindholm C, Searle R. Wound management for the 21st century: combining effectiveness and efficiency. Int Wound J. 2016;13(suppl S2:5‐15. 10.1111/iwj.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kathryn R, Vowden P, Vowden K. The prevalence, management and outcome for patients with lower limb ulceration identified in a wound care survey within one English health care district. J Tissue Viability. 2009;18(1):13‐19. [DOI] [PubMed] [Google Scholar]
- 3. Finnish National Registry . National Institute for Health and Welfare Web site. www.thl.fi. Accessed November 30, 2016.
- 4. Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2008. Nov‐Dec;17(6):763‐771. 10.1111/j.1524-475X.2009.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guest JF, Ayoub N, McIlwraith T, et al. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open. 2015;5:e009283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Järbrink K, Ni G, Sönnergren H, et al. Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review. Syst Rev. 2016;5(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mäkelä A, Annanmäki L, Koivunen E, et al. Cross‐sectional survey of the occurrence of chronic wounds within capital region in Finland. EWMA J. 2010;10(1):24‐26. [Google Scholar]
- 8.Statistics Finland Web site. www.stat.fi. Accessed January 30, 2017.
- 9. Wicke C, Bachinger A, Coerper S, Beckert S, Witte MB, Königsrainer A. Aging influences wound healing in patients with chronic lower extremity wounds treated in a specialized Wound Care Center. Wound Repair Regen. 2009;17(1):25‐33. [DOI] [PubMed] [Google Scholar]
- 10. Körber A, Klode J, Al‐Benna A, et al. Etiology of chronic leg ulcers in 31,619 patients in Germany analyzed by an expert survey. J Dtsch Dermatol Ges. 2011. Feb;9(2):116‐121. [DOI] [PubMed] [Google Scholar]
- 11. Forssgren A, Nelzen O. Changes in the aetiological Spectrum of leg‐ulcers after a broad‐scale intervention in a defined geografical population in Sweden. Eur J Vasc Endovasc Surg. 2012;44:498‐503. [DOI] [PubMed] [Google Scholar]
- 12. Pellinen A, Kekki P. Vuodeosastopotilaiden painehaavaumat esiintyvyys ja henkilöstön käsitykset. Suom Lääkäril. 1994;49:3196‐3199. [Google Scholar]
- 13. Gunningberg L, Hommel A, Bååth C, Idvall E. The first national pressure ulcer prevalence in county council and municipality settings in Sweden. J Eval Clin Pract. 2013. Oct;19(5):862‐867. [DOI] [PubMed] [Google Scholar]
- 14. Graham I, Harrison M, Nelson E, Lorimer K, Fisher A. Prevalence of lower‐limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care. 2003;16:305‐316. [DOI] [PubMed] [Google Scholar]


