Abstract
Background
The COVID-19 pandemic placed considerable strain on critical care resources. How US hospitals responded to this crisis is unknown.
Research Question
What actions did US hospitals take to prepare for a potential surge in demand for critical care services in the context of the COVID-19 pandemic?
Study Design and Methods
From September to November 2020, the chief nursing officers of a representative sample of US hospitals were surveyed regarding organizational actions taken to increase or maintain critical care capacity during the COVID-19 pandemic. Weighted proportions of hospitals for each potential action were calculated to create estimates across the entire population of US hospitals, accounting for both the sampling strategy and nonresponse. Also examined was whether the types of actions taken varied according to the cumulative regional incidence of COVID-19 cases.
Results
Responses were received from 169 of 540 surveyed US hospitals (response rate, 31.3%). Almost all hospitals canceled or postponed elective surgeries (96.7%) and nonsurgical procedures (94.8%). Few hospitals created new medical units in areas not typically dedicated to health care (12.9%), and almost none adopted triage protocols (5.6%) or protocols to connect multiple patients to a single ventilator (4.8%). Actions to increase or preserve ICU staff, including use of ICU telemedicine, were highly variable, without any single dominant strategy. Hospitals experiencing a higher incidence of COVID-19 did not consistently take different actions compared with hospitals facing lower incidence.
Interpretation
Responses of hospitals to the mass need for critical care services due to the COVID-19 pandemic were highly variable. Most hospitals canceled procedures to preserve ICU capacity and scaled up ICU capacity using existing clinical space and staffing. Future research linking hospital response to patient outcomes can inform planning for additional surges of this pandemic or other events in the future.
Key Words: COVID-19, critical care, ICU organization, triage
FOR EDITORIAL COMMENT, SEE PAGE 391
COVID-19, the illness caused by the SARS-CoV-2 virus, has rapidly spread around the world in a global pandemic that has strained, and in some regions overwhelmed, the capacity of existing critical care resources. The virus first emerged in November 2019, and as of December 2020, there have been > 15 million cases worldwide, with ongoing spread at a rate of > 200,000 cases per day.1 COVID-19 is associated with high rates of respiratory failure and critical illness. In the early phase of the pandemic, more than one-half of patients with COVID-19 required hospitalization,2 and 15% to 20% of hospitalized patients were admitted to ICUs predominantly for respiratory failure requiring mechanical ventilation and shock requiring vasopressor support.3, 4, 5 Critically ill patients with COVID-19 have prolonged ICU courses, requiring an average of 2 weeks of mechanical ventilation.6,7 Thus, the sheer volume of patients and their extended critical illness combined have created an unprecedented demand for intensive care.
Prior to the current pandemic, several groups developed recommendations for hospitals and ICUs to respond to mass critical care needs in the case of an epidemic, bioterrorism, or other mass casualty event.8,9 These recommendations were broad and far-reaching and were generally organized around the 3 S’s of preparedness: space, staff, and stuff.10,11 They outlined that hospitals should have the ability to expand ICU capacity by extending to other hospital areas, with appropriate beds and monitors for expansion areas; be able to rapidly increase clinical and nonclinical staffing and models of using noncritical care staff to care for ICU patients; and have plans to ensure availability of necessary medical equipment and medications. Recommendations also emphasized the importance of established networks of regional coordination across hospital systems and establishing objective, ethical, and transparent triage systems under the most extreme circumstances.
Despite these recommendations, as the COVID-19 pandemic unfolded, it quickly became obvious that many hospitals and clinicians were ill-prepared to meet the demands of caring for the surges of patients with COVID-19. Clinicians had concerns about inadequate staffing; shortages of supplies, medications, and beds; and overcrowding.12,13 Anecdotal reports from hospitals experiencing surges suggested a patchwork of responses and solutions.14, 15, 16, 17, 18, 19, 20, 21 However, robust data on how hospitals actually responded to the surge in demand for critical care services during this period are lacking. To better understand this issue, we performed a structured survey of a representative sample of US hospitals asking what steps they planned for or undertook during the first phase of the COVID-19 pandemic.
Materials and Methods
Study Design and Population
We performed a cross-sectional survey of US hospitals identified by using the 2018 American Hospital Association Annual Survey Database. We also used the Centers for Medicare & Medicaid Services Healthcare Cost Reporting Information System to obtain hospital characteristics not present in the American Hospital Association Annual Survey, as well as the Pittsburgh Atlas crosswalk to assign hospitals to geographic regions that reflect their acute care catchment areas.22 To estimate the total population by region, projections from the 2010 United States Census (Geolytics) were used. The New York Times COVID-19 case database was used to determine the incidence of COVID-19 according to region and date.23
The survey was limited to general, acute care hospitals with an ICU. Because it was not feasible to survey all eligible hospitals, we created a sample using a combination of random and purposeful sampling. First, all eligible hospitals were stratified based on size, teaching status, health system membership, and cumulative incidence of COVID-19 in the hospital’s geographic region on the date the study was launched (June 29, 2020), randomly selecting up to 10 hospitals in each stratum. Next, we enriched this sample by purposefully selecting all hospitals in the four regions with the greatest cumulative COVID-19 incidence at the time of study launch. This sampling approach ensured adequate representation of a broad range of hospital types, while also ensuring adequate representation of hospitals that dealt with a substantial burden of patients with COVID-19. A detailed description of the sampling strategy is provided in e-Appendix 1.
Survey Development
We drafted the survey instrument based on previous ICU organizational surveys,24, 25, 26, 27, 28 existing frameworks for pandemic preparedness,10,11,29 and published case studies about hospital responses during the early phases of the pandemic.18, 19, 20, 21 We piloted the survey with six ICU nursing leaders at two institutions to obtain their feedback about the content, form, and structure. The final survey included 30 items within five domains: hospital characteristics related to ICU organization and management; actions intended to reduce demand for critical care; actions intended to increase the supply and/or efficiency of critical care; actions related to mechanical ventilation; and actions related to staffing. For each action, respondents could indicate that they either did it, considered doing it but did not actually do it, never considered doing it, or were unsure. The complete survey instrument is provided in e-Appendix 2.
Survey Administration
The survey was administered from September 14, 2020, through November 20, 2020. A mixed methods approach was used whereby respondents were invited by mail and telephone to complete the survey on-line using a commercial electronic survey tool (Qualtrics). All mail correspondence was addressed to the hospital’s Chief Nursing Officer, with instructions to pass the survey on to another individual should they not be the best person to complete the survey. We chose to send the survey invitation to the Chief Nursing Officer because this position exists at all US hospitals, and people in this role are well positioned to be able to answer questions about hospital surge planning. To incentivize participation, the initial invitation letter included a $10 bill and offered a $50 gift card upon completion. Nonrespondents were sent two additional letters at 2-week intervals. We then attempted to contact nonresponders by telephone to encourage them to complete the survey. During the telephone call, a research assistant also offered to complete the questionnaire over the telephone if desired by the participant.
Analyses
To evaluate for the possibility of nonresponse bias, characteristics of responding hospitals and nonresponding hospitals were compared by using Fisher exact test. Characteristics of interest included the stratification variables described earlier, as well as ICU size and the size of the hospital’s metropolitan statistical area. For this analysis, we considered a survey to be a response when it was > 30% complete.
Among respondents, we then calculated the proportion of hospitals that took each potential action. Both unweighted proportions and weighted proportions were calculated. To estimate weighted proportions, we accounted for the sampling strategy by creating inverse probability sampling weights based on the number of hospitals in the respondent’s stratum.30 We also accounted for nonresponse by creating a propensity score for survey response using a logistic regression model in which the independent variables were all hospital characteristics described earlier.31 The final survey weights were the product of the sampling weights and the propensity score.
A bivariate analysis was also performed in which we examined whether hospitals’ actions were associated with the cumulative incidence of COVID-19 cases in their region. To simplify this analysis, the survey responses were dichotomized as either yes, indicating that the hospital completed the action, or no, indicating any other response. The cumulative incidence of COVID-19 in each hospital’s region was also dichotomized as either high (defined as at or above the median) or low (defined as below the median). For this analysis, we used the incidence on the date the respondent took the survey rather than the date the survey was launched. The statistical significance of differences across groups was assessed by using Rao-Scott corrected F tests.32
Statistical analyses were performed with Stata 16.1 (StataCorp). A P value ≤ .05 was considered significant. All aspects of this research were reviewed and approved by the University of Pittsburgh Human Research Protections Office.
Results
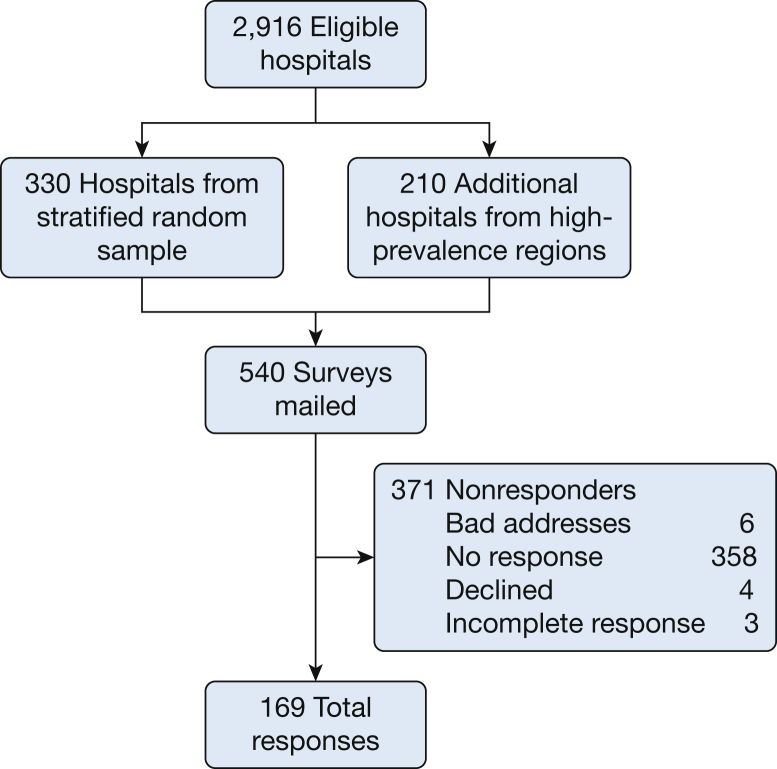
Surveys were sent to Chief Nursing Officers of 540 US hospitals, including 330 hospitals from the stratified random sample and 210 additional hospitals from the high-prevalence regions, and responses were received from 169 (31%) (Fig 1). A total of 148 (87.6%) respondents were Chief Nursing Officers. Other respondent types included hospital leaders of quality, safety, and patient care (n = 7 [4.1%]), ICU leaders (n = 5 [3.0%]), Chief Operating Officers (n = 4 [2.4%]), other nursing administrators (n = 3 [2.3%]), and other hospital administrators (n = 2 [1.2%]). Table 1 summarizes characteristics of surveyed hospitals. Nonresponding hospitals had more ICU beds, were located in larger communities, were more likely to be part of a hospital system, and were more likely to be in regions of higher COVID-19 caseloads.
Figure 1.
Flow diagram for hospital sampling strategy and survey responses.
Table 1.
Characteristics of Responding Hospitals and Nonresponding Hospitals
| Characteristic | Responding Hospitals (n = 169) |
Nonresponding Hospitals (n = 371) |
P Value |
|---|---|---|---|
| Hospital size | .22 | ||
| < 100 beds | 42 (25.0) | 74 (19.9) | |
| 100-250 beds | 67 (39.9) | 138 (37.2) | |
| > 250 beds | 60 (35.5) | 159 (43.0) | |
| ICU size | .02 | ||
| 1-10 beds | 41 (24.3) | 81 (21.8) | |
| 11-30 beds | 67 (39.6) | 110 (29.6) | |
| > 30 beds | 61 (36.1) | 180 (48.5) | |
| Teaching statusa | .85 | ||
| Teaching hospital | 89 (52.7) | 192 (51.8) | |
| Nonteaching hospital | 80 (47.3) | 179 (48.2) | |
| Community sizeb | .001 | ||
| < 100,000 | 45 (26.6) | 55 (14.8) | |
| 100,000 to 1 million | 47 (27.8) | 92 (24.8) | |
| > 1 million | 77 (45.6) | 224 (60.4) | |
| Membership in a hospital system | .001 | ||
| Member | 89 (52.7) | 251 (67.5) | |
| System nonmember | 80 (47.3) | 120 (32.5) | |
| COVID-19 regional case loadc | .02 | ||
| Low | 38 (22.5) | 58 (15.6) | |
| Medium | 42 (24.9) | 72 (19.4) | |
| High | 89 (52.7) | 241 (65.0) |
All values are frequency (percent). Percentages may not add to 100 due to rounding. P values comparing responding hospitals vs nonresponding hospitals are from Fisher’s exact test.
Teaching status determined by a resident full-time equivalents > 0 from the 2018 Centers for Medicare & Medicaid Cost Reports.
Total population of the hospital’s metropolitan statistical area obtained from the 2013 United States Census.
Regional case load as determined from the New York Times COVID-19 database on June 29, 2020. Low = < 2,000; medium = 2,001 to 14,250; and high > 14,250.
Table 2 summarizes the actions and preparations in response to COVID-19-related surge in demand for critical care services, reported as weighted estimates of all US hospitals. The unweighted survey results are presented in e-Table 1. To reduce overall demand for intensive care by non-COVID-19 patients, the vast majority of hospitals canceled or postponed both elective surgeries (96.7%) and nonsurgical procedures (94.8%). Many hospitals were also prepared to cancel medical treatments (53.3%) but did not do so. To increase efficiency/supply of ICUs, a majority of hospitals dedicated specific ICUs for patients with COVID-19 (63.3%). The majority of hospitals were also prepared to transform other clinical units (eg, step-down units, medical wards, even non-ward clinical spaces) into ICUs, but many did not actually do so, and only very few hospitals created new medical units altogether (12.9%).
Table 2.
Weighted National Estimates of Actions Taken to Prepare for and/or Respond to a Surge in Critically Ill Patients Related to COVID-19 Among US Hospitals
| Action | Prepared and Did It | Prepared But Did Not Do It | Did Not Prepare or Unsure |
|---|---|---|---|
| Actions to reduce demand for intensive care | |||
| Canceled/postponed elective surgery | 96.7% | 2.9% | 1.0% |
| Canceled/postponed nonsurgical procedures | 94.8% | 3.6% | 1.6% |
| Adopted a policy to transfer more patients to other acute care hospitals | 36.0% | 47.1% | 17.0% |
| Canceled/postponed medical treatments | 28.8% | 53.3% | 17.9% |
| Adopted a policy to accept fewer transfers from other acute care hospitals | 20.4% | 37.8% | 41.7% |
| Actions to increase efficiency/supply of ICUs | |||
| Dedicated specific ICUs as “COVID-19” ICUs | 63.3% | 21.0% | 15.7% |
| Repurposed existing step-down units as ICUs | 50.8% | 37.6% | 11.6% |
| Repurposed other clinical care space not typically dedicated to inpatient care as an ICU | 32.7% | 58.7% | 8.6% |
| Repurposed existing medical/surgical units as ICUs | 24.0% | 49.6% | 26.4% |
| Created new medical units in areas not typically dedicated to health care | 12.9% | 47.7% | 39.4% |
| Actions to increase or preserve ventilator capacity | |||
| Bought or borrowed additional mechanical ventilators | 70.7% | 27.2% | 2.1% |
| Used noninvasive ventilators, CPAP machines, or anesthesia machines for mechanical ventilation | 29.5% | 63.8% | 6.8% |
| Developed or adopted a protocol for rationing ventilators | 5.6% | 64.4% | 29.9% |
| Developed or adopted a protocol for connecting more than one patient to a single ventilator | 4.8% | 61.3% | 34.0% |
| Actions to increase or preserve ICU staff | |||
| Created specialized teams to perform procedures on COVID-19 patients | 59.5% | 23.0% | 17.5% |
| Asked ICU providers to work longer hours or extra shifts | 61.3% | 30.3% | 8.4% |
| Brought in new ICU providers who do not typically work in the hospital to help out | 41.7% | 34.0% | 24.3% |
| Altered traditional provider/patient ratios | 33.3% | 63.1% | 3.6% |
| Used a "team nursing" model to care for patients in COVID-19 ICUs | 33.2% | 52.8% | 14.0% |
| Put non-ICU providers to work in the ICUs | 36.1% | 49.2% | 14.7% |
| Expanded APP roles and/or privileges | 24.8% | 36.1% | 39.1% |
| Actions related to telemedicine | |||
| Expanded an ICU telemedicine program to cover more beds in the hospital | 39.1% | 29.5% | 31.4% |
| Introduced an ICU telemedicine program to cover beds within the hospital | 25.6% | 21.1% | 53.3% |
Weighted estimates used inverse probability weighting to account for the sampling strategy and propensity score methods to account for nonresponse. APP = advanced practice providers.
To increase or preserve ventilator capacity, most hospitals bought or borrowed additional mechanical ventilators (70.7%), and most of the remaining hospitals were at least prepared to do so (27.2%). Almost no hospitals actually developed protocols for rationing ventilators (5.6%) or connecting multiple patients to a single ventilator (4.8%), although a majority were prepared to do both (64.4% and 61.3%, respectively).
Many organizational modifications were made to increase or preserve ICU staff. In a majority of hospitals, ICU providers had increased working hours (61.3%) and newly created specialized procedure teams dedicated to patients with COVID-19 (59.5%). Most hospitals also either reassigned providers from other units and roles to ICUs (36.1%) or prepared to do so (49.2%). Table 3 summarizes provider reassignment patterns among hospitals that made this organizational change; unweighted estimates are given in e-Table 2. Relatedly, most hospitals employed or prepared to employ “team nursing” models, in which ICU nurses and medical/surgical nurses cared for patients as a team, to support the reassigned nursing staff (33.2% and 52.8%, respectively). Some hospitals also specifically expanded roles and responsibilities of advanced practice providers (24.8%), thereby expanding staff with prescribing, ordering, and procedural privileges. A majority of hospitals also either brought in new ICU providers (41.7%) or were prepared to do so if needed (34.0%). Finally, many hospitals expanded existing ICU telemedicine programs (39.1%), and a significant minority of hospitals introduced a new telemedicine program (25.6%) to extend critical care expertise to more hospital beds.
Table 3.
Weighted National Estimates of Patterns of Nontraditional ICU Providers in the Roles of ICU Providers
| Type | % |
|---|---|
| Medical/surgical nurses used in the role of ICU nurses | 29.9 |
| ED, PACU, or operating room nurses in the role of ICU nurses | 15.7 |
| Physicians without critical care certification in the role of intensivists | 9.7 |
| PICU clinicians in the role of adult ICU clinicians | 2.2 |
| Other | 13.8 |
Weighted estimates used inverse probability weighting to account for the sampling strategy and propensity score methods to account for nonresponse. PACU = postanesthesia care unit.
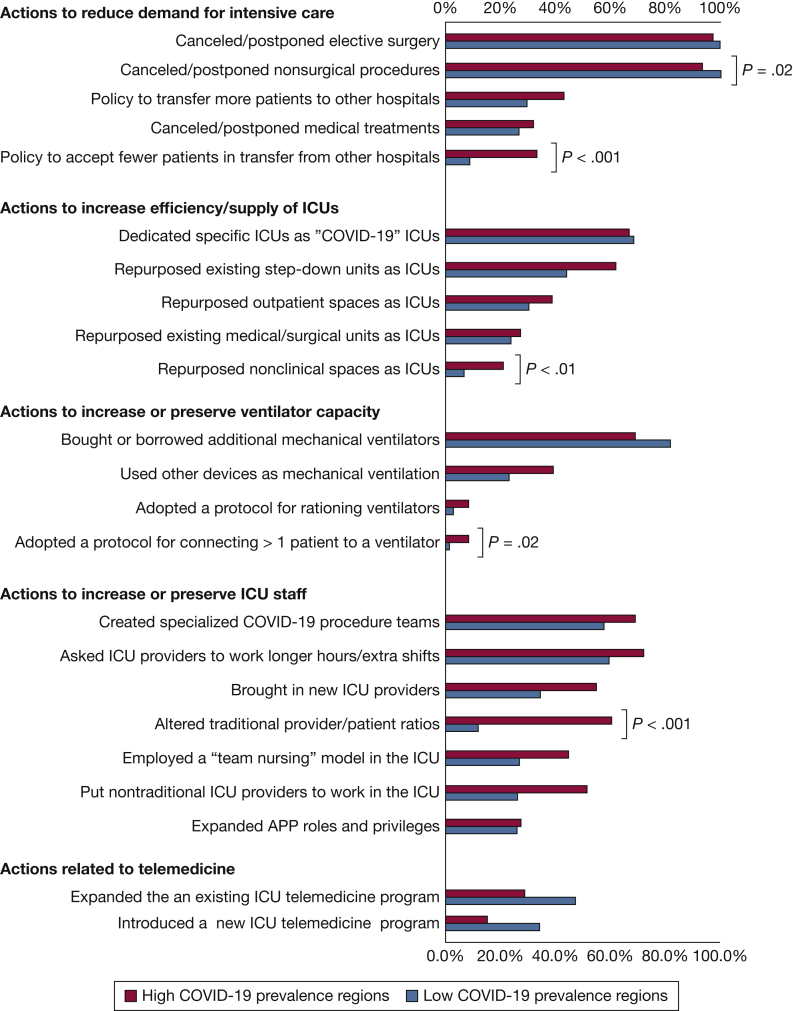
Hospitals in high-prevalence regions took four specific actions more often than those in low-prevalence regions (Fig 2): (1) they adopted policies to accept fewer interhospital transfer patients (32.3% vs 8.7%; P < .001); (2) they repurposed nonclinical spaces as ICUs (19.7% vs 6.2%; P < .01); (3) they adopted a protocol for connecting multiple patients onto a single ventilator (8.3% vs 1.4%; P = .02); and (4) they altered traditional provider-to-patient ratios (56.8% vs 11.5%; P < 0.001). Hospitals in low-prevalence regions more often canceled/postponed nonsurgical procedures compared with those in high-prevalence regions (98.0% vs 91.6%; P = .02).
Figure 2.
Actions taken comparing hospitals in high and low COVID-19 prevalence regions. APP = advanced practice providers.
Discussion
To the best of our knowledge, this study is the first nationally representative survey of organizational actions taken to respond to the surge in demand for critical care services in the United States due to the COVID-19 pandemic. Because of the sampling strategy used, we were able to generate national estimates of response actions and preparations. We found variability across hospitals in most actions, suggesting that hospitals’ individual responses were likely tailored to their local perceived needs, priorities, and resources.
There were a few notable exceptions to this variability. First, virtually all hospitals reported canceling elective procedures, in line with national recommendations at the start of the pandemic.33,34 Canceling elective procedures addressed several surge planning issues: preserving ICU bed capacity, preserving personal protective equipment, freeing up clinicians to staff ICU expansions, and potentially reducing risk of transmission among health care workers and patients, to name a few. However, canceling procedures also had potential downsides. Many procedures considered “elective” are important to patients, and delaying such procedures can cause emotional and physical harm.35,36 Surgical procedures are also a financial lifeline for small hospitals and safety net hospitals that can ill-afford to forgo revenue during a pandemic.37 More research is needed to better understand these tradeoffs. In the interim, the decision to cancel elective surgery should be made based on local considerations after weighing the needs of all relevant stakeholders.
Another action that was notably consistent across hospitals was that most hospitals transformed (or prepared to transform) existing clinical space (predominantly other hospital units) into ICUs but did not create new clinical space or use nonclinical space to add ICU capacity. Prior to this pandemic, the United States had more ICU beds per capita than almost any other country, sometimes by an order of magnitude.38 Although this has been a cause for criticism as a potential source of inefficiency and high-cost/low-value care,39 the COVID-19 crisis has tested this thesis, as some regions of the world have been forced to implement ICU triage protocols due to inadequacy of ICU resources.40 Indeed, early in the pandemic, some projections led experts to call for emergency expansion of hospital and ICU beds.41 By the time this survey was conducted, few US hospitals reached a point where they adopted a protocol for rationing ventilators or for connecting more than one patient to a single ventilator, reflecting that hospital leaders perceived that they could safely deliver care without resorting to explicit rationing of equipment. This suggests that with flexible use of clinical spaces, the US health care system was largely able to meet the demand for ICU beds, although our findings do not rule out the possibility of implicit rationing by clinicians at the bedside. Furthermore, whether those beds are adequately staffed is another important consideration that remains unanswered.
Regarding staffing, hospitals also showed remarkable flexibility. The fact that there was no single dominant strategy for ICU staffing highlights the preceding organizational variability and that hospitals tailored their approaches accordingly. Of note, hospitals in high-prevalence regions were more likely to alter traditional staffing ratios, presumably to assign more patients for a single provider. This pattern may reflect the strong belief in certain staffing ratios and the potential negative impact of strain, with respect to both patient outcomes and clinician wellness. California and Massachusetts have mandated nurse-to-patient ratios (eg, two patients per nurse in the ICU).42,43 Although California’s governor waived these ratios during the pandemic, the governor of Massachusetts did not. Also remarkable is the relatively high proportion of hospitals using innovative staffing approaches such as team nursing, where teams of nurses work collectively to care for a larger number of patients44,45 (eg, four registered nurses and one aide for 10 patients compared with one ICU nurse for two patients), thereby extending the critical care expertise of individual nurses to a larger number of patients.
Our study has a few important limitations. First, although we sent the surveys to a nationally representative hospital sample to generate population estimates, the response rate was low, posing a risk of response bias. We used typical incentives to promote participation; however, busy hospital leaders likely had more limited availability to participate in a voluntary survey. Nonresponders included a higher percentage of larger hospitals in larger communities. We used statistical techniques to account for nonresponse in weighted estimates. Second, because of the nature of the virus transmission, the first “surges” happened in different regions at different times; our survey was administered at one point in time, however, such that hospitals were at variable stages of their pandemic planning and response. In some cases, hospitals may have prepared to take a specific action but not yet taken it, but may proceed to take it following the survey or in the future. This too may have led to inaccuracy in capturing the complete picture of the US response to the pandemic. However, this limitation reflects the reality of conducting organizational research during a fast-moving pandemic. In addition, we specifically aimed to capture data regarding the initial response to the pandemic and accounted for local prevalence in our analyses. Finally, our study was not designed to identify implicit rationing that may have occurred at the bedside.
Interpretation
The current survey of a representative sample of US hospitals summarizes the variability in hospital responses to the mass need for critical care services due to the COVID-19 pandemic. Most hospitals canceled procedures to preserve ICU capacity and scaled up ICU capacity by using existing clinical space, resources, and staffing. Almost no hospitals needed to adopt triage protocols or protocols for ventilator sharing. Future research linking hospital response to patient outcomes can inform planning for additional surges of this pandemic or other events in the future.
Take-home Points.
Study Question: What actions did US hospitals take in response to the surge in critical care demand that resulted from the COVID-19 pandemic?
Results: Hospital response actions were highly variable and largely unrelated to the prevalence of COVID-19 infection in their region, although almost all hospitals canceled elective procedures and very few expanded ICU services into nonclinical spaces.
Interpretation: Actions taken in response to the COVID-19 pandemic were variable across the United States, and future research to understand the impact of specific actions is needed.
Acknowledgments
Author contributions: J. M. K. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. M. P. K., D. K. C., and J. M. K. contributed substantially to the conception of the project and the study design. B. S. D., A. J. A., K. C. V., M. P. K., D. K. C., and J. M. K. contributed to the development of the survey, the analysis and interpretation of the results, and the preparation of the manuscript. All authors contributed to the development of the survey, the analysis and interpretation of the results, and the preparation of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: K. C. V. is supported by resources from the VA Portland Health Care System. A. J. A. is supported by resources from the VA Ann Arbor Health Care System. None declared (M. P. K., D. K. C., B. S. D., J. M. K.).
Role of sponsors: The funding agency had no role in the development of the research or the manuscript. The Department of Veterans Affairs did not have a role in the conduct of the study; in the collection, management, analysis, or interpretation of data; or in the preparation of the manuscript.
Other contributions: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the US Government.
Additional information: The e-Appendixes and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This study was funded by the National Institutes of Health [R35HL144804].
Supplementary Data
References
- 1.Johns Hopkins University Coronavirus Resource Center. https://coronavirus.jhu.edu/
- 2.Petrilli C.M., Jones S.A., Yang J. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatraju P.K., Ghassemieh B.J., Nichols M. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020;382(21):2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doidge J.C., Gould D.W., Ferrando-Vivas P. Trends in intensive care for patients with COVID-19 in England, Wales and Northern Ireland. Am J Respir Crit Care Med. 2021;203(5):565–574. doi: 10.1164/rccm.202008-3212OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karagiannidis C., Mostert C., Hentschker C. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8(9):853–862. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christian M.D., Devereaux A.V., Dichter J.R., Geiling J.A., Rubinson L. Definitive care for the critically ill during a disaster: current capabilities and limitations: from a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133(5):8S–17S. doi: 10.1378/chest.07-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sprung C.L., Zimmerman J.L., Christian M.D. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(3):428–443. doi: 10.1007/s00134-010-1759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams L.M. Exploring the concept of surge capacity. Online J Issues Nurs. 2009;14(2) [Google Scholar]
- 11.Barbisch D.F., Koenig K.L. Understanding surge capacity: essential elements. Acad Emerg Med. 2006;13(11):1098–1102. doi: 10.1197/j.aem.2006.06.041. [DOI] [PubMed] [Google Scholar]
- 12.Wahlster S., Sharma M., Lewis A.K. The coronavirus disease 2019 pandemic’s effect on critical care resources and health-care providers: a global survey. Chest. 2021;159(2):619–633. doi: 10.1016/j.chest.2020.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Society of Critical Care Medicine ICU readiness assessment: we are not prepared for COVID-19. https://www.sccm.org/getattachment/Blog/April-2020/ICU-Readiness-Assessment-We-Are-Not-Prepared-for/COVID-19-Readiness-Assessment-Survey-SCCM.pdf?lang=en-US
- 14.The Coronavirus is Forcing Hospitals to Cancel Surgeries. New York Times. https://www.nytimes.com/2020/03/14/us/coronavirus-covid-surgeries-canceled.html
- 15.Barbash I.J., Sackrowitz R.E., Gajic O. Rapidly deploying critical care telemedicine across states and health systems during the Covid-19 pandemic. NEJM Catalyst Innovations Care Delivery. 2020;1(4) [Google Scholar]
- 16.Yager P.H., Whalen K.A., Cummings B.M. Repurposing a pediatric ICU for adults. N Engl J Med. 2020;382(22) doi: 10.1056/NEJMc2014819. [DOI] [PubMed] [Google Scholar]
- 17.Anderson B.R., Ivascu N.S., Brodie D. Breaking silos: the team-based approach to coronavirus disease 2019 pandemic staffing. Critical Care Explorations. 2020;2(11) doi: 10.1097/CCE.0000000000000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carenzo L., Costantini E., Greco M. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- 19.Griffin K.M., Karas M.G., Ivascu N.S., Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Resp Crit Care Med. 2020;201(11):1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spina S., Marrazzo F., Migliari M., Stucchi R., Sforza A., Fumagalli R. The response of Milan's Emergency Medical System to the COVID-19 outbreak in Italy. Lancet. 2020;395(10227):e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xie J., Tong Z., Guan X., Du B., Qiu H., Slutsky A.S. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020;46(5):837–840. doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wallace D.J., Mohan D., Angus D.C. Referral regions for time-sensitive acute care conditions in the United States. Ann Emerg Med. 2018;72(2):147–155. doi: 10.1016/j.annemergmed.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.GitHub nytimes/COVID-19 data. https://github.com/nytimes/covid-19-data
- 24.Soares M., Bozza F.A., Angus D.C. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41(12):2149–2160. doi: 10.1007/s00134-015-4076-7. [DOI] [PubMed] [Google Scholar]
- 25.Costa D.K., Wallace D.J., Kahn J.M. The association between daytime intensivist physician staffing and mortality in the context of other ICU organizational practices: a multicenter cohort study. Crit Care Med. 2015;43(11):2275. doi: 10.1097/CCM.0000000000001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim M.M., Barnato A.E., Angus D.C., Fleisher L.F., Kahn J.M. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010;170(4):369–376. doi: 10.1001/archinternmed.2009.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kohn R., Madden V., Kahn J.M. Diffusion of evidence-based intensive care unit organizational practices. A state-wide analysis. Ann Am Thorac Soc. 2017;14(2):254–261. doi: 10.1513/AnnalsATS.201607-579OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallace D.J., Angus D.C., Barnato A.E., Kramer A.A., Kahn J.M. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anesi G.L., Lynch Y., Evans L. A conceptual and adaptable approach to hospital preparedness for acute surge events due to emerging infectious diseases. Critical Care Explorations. 2020;2(4) doi: 10.1097/CCE.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seaman S.R., White I.R. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- 31.Schonlau M., Van Soest A., Kapteyn A., Couper M. Selection bias in web surveys and the use of propensity scores. Sociolog Methods Res. 2009;37(3):291–318. [Google Scholar]
- 32.Rao J., Scott A. On simple adjustments to chi-square tests with sample survey data. Ann Statistics. 1987;15(1):385–397. [Google Scholar]
- 33.American College of Surgeons COVID-19: recommendations for management of elective surgical procedures. https://www.facs.org/about-acs/covid-19/information-for-surgeons
- 34.Adams J. United States Surgeon General Twitter Feed. https://twitter.com/Surgeon_General/status/1238798972501852160
- 35.Nurok M., Kahn J.M. Intensive care unit capacity, cancellation of elective surgery, and the US pandemic response. Anesth Analg. 2020;131(5):1334–1336. doi: 10.1213/ANE.0000000000005170. [DOI] [PubMed] [Google Scholar]
- 36.Shehata I.M., Elhassan A., Jung J.W., Urits I., Viswanath O., Kaye A.D. Elective cardiac surgery during the COVID-19 pandemic: proceed or postpone? Best Pract Res Clin Anaesthesiol. 2020;34(3):643–650. doi: 10.1016/j.bpa.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Best M.J., McFarland E.G., Anderson G.F., Srikumaran U. The likely economic impact of fewer elective surgical procedures on US hospitals during the COVID-19 pandemic. Surgery. 2020;168(5):962–967. doi: 10.1016/j.surg.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wunsch H., Angus D.C., Harrison D.A. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36(10):2787–e2788. doi: 10.1097/CCM.0b013e318186aec8. [DOI] [PubMed] [Google Scholar]
- 39.Anesi G.L., Admon A.J., Halpern S.D., Kerlin M.P. Understanding irresponsible use of intensive care unit resources in the USA. Lancet Respir Med. 2019;7(7):605–612. doi: 10.1016/S2213-2600(19)30088-8. [DOI] [PubMed] [Google Scholar]
- 40.Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 41.Moghadas S.M., Shoukat A., Fitzpatrick M.C. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc National Acad Sci. 2020;117(16):9122. doi: 10.1073/pnas.2004064117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Law A.C., Stevens J.P., Hohmann S., Walkey A.J. Patient outcomes after the introduction of statewide ICU nurse staffing regulations. Crit Care Med. 2018;46(10):1563–1569. doi: 10.1097/CCM.0000000000003286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mark B.A., Harless D.W., Spetz J., Reiter K.L., Pink G.H. California's minimum nurse staffing legislation: results from a natural experiment. Health Serv Res. 2013;48(2 pt 1):435–454. doi: 10.1111/j.1475-6773.2012.01465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waters K. Team nursing. Nurs Pract. 1985;1(1):7–15. [PubMed] [Google Scholar]
- 45.Shukla R.K. All-RN model of nursing care delivery: a cost-benefit evaluation. Inquiry. 1983;20(2):173–184. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.