Dear Editors,
A 57-year-old woman with a medical background of tobacco use and chronic obstructive pulmonary disease was admitted to a clinic in Buenos Aires on April 24, 2020, with a 2-week history of diarrhea, abdominal pain, headache and retro-orbital pain, aching joints, dyspnea, subfebrile, pruritic rash, and unspecific thoracic pain. Upon admission, her vital signs were normal. A physical examination revealed a nonblanching, generalized rash with scattered petechiae predominantly on the extremities, upper trunk, and abdomen (Fig. 1). Chest radiography and thoracic computed tomography showed no signs of pneumonia. There were no electrocardiographic changes, and cardiac biomarkers were negative; therefore, coronary syndrome was discarded. Laboratory examinations, including acute phase reactants, were all normal. A human immunodeficiency virus test was negative, and a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) polymerase chain reaction (PCR) test from a nasopharyngeal swab test tested positive. A skin biopsy showed epidermal atrophy and marked superficial angiectasia, dermis with intense edema, and no associated inflammatory changes (Fig. 2).
Fig. 1.
Scattered petechiae on the arm.
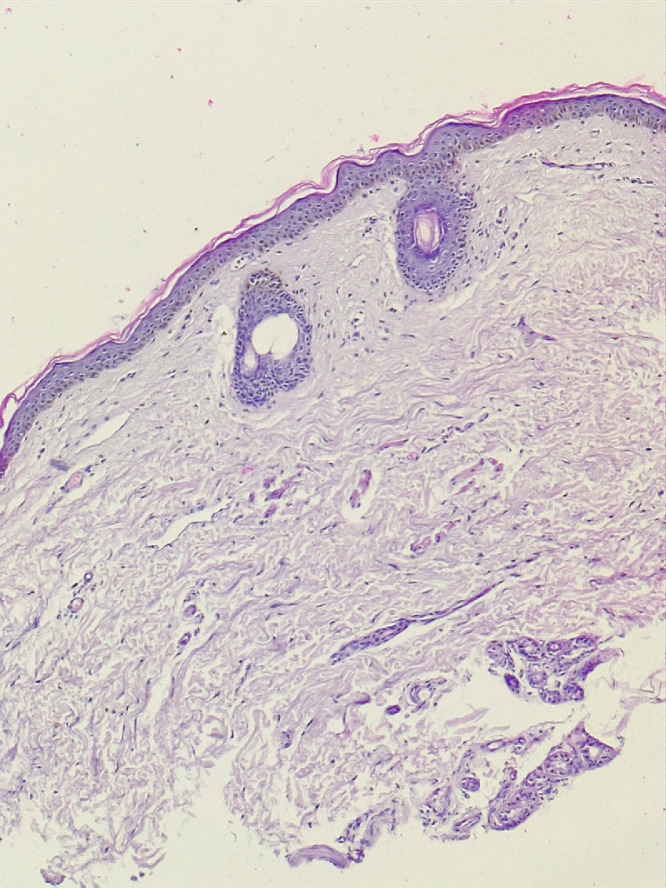
Fig. 2.
Superficial angiectasia and dermis with intense edema (hematoxylin and eosin, 40 ×).
The patient subsequently developed thrombocytopenia, so a Dengue virus (DENV) PCR was performed, which was positive. Consequently, the diagnoses of both COVID-19 and Dengue were made. The patient was treated symptomatically, and her condition gradually improved over 5 days.
SARS-CoV-2 belongs to the coronaviridiae family, which are enveloped viruses with a positive sense single-stranded RNA (Huang et al., 2020). DENV is a mosquito-borne arbovirus of the flaviviridae family. These viruses are enveloped and spherical, with a positive-sensed and single-stranded RNA. The incidence of Dengue infection has been increasing over the past few years in Argentina, as well as in the rest of the world. The vector responsible for the transmission in Argentina is the Aedes aegypti mosquito.
The two entities are difficult to distinguish because they share nonspecific clinical presentations, skin findings, laboratory features, and physiopathology. A range of cutaneous manifestations in COVID-19 patients have been described, with the most common ones being morbilliform rash, petechial rash, widespread urticaria, pseudo-chilblain acral lesions, and vesicular and livedoid eruptions. The exact percentage of infected individuals who develop cutaneous eruptions remains unclear (Young and Fernandez, 2020).
The spectrum of common Dengue-associated exanthemas includes macular-papular rash during the febrile phase, petechial rash on the extremities during the febrile or critical phase, and erythematous widespread rash with islands of white during the recovery phase (Yacoub and Wills, 2015). Dengue exanthemas and purpura have been reported as a more discriminating criterion for Dengue fever rather than COVID-19 (Nacher et al., 2020).
Petechial rash, the cutaneous manifestation that our patient presented, was described in both diseases. Whether this rash was related to DENV or SARS-CoV-2 or result of coinfection could not be established because immunohistochemistry to SARS-CoV-2 in skin biopsy is not available at our institution.
Moreover, there are reports in the literature of false-positive results from rapid serological testing for Dengue (Yan et al., 2020). We recommend confirming the diagnosis by PCR for a higher specificity whenever possible. Physicians should have a high index of suspicion to detect and timely manage each condition and ought to be aware of the possibility of coinfection mainly in endemic regions, such as the case we report in this article.
Conflicts of interest
None.
Funding
None.
Study approval
The author(s) confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies.
References
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel Coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacher M., Douine M., Gaillet M., Flamand C., Rousset D., Rousseau C., et al. Simultaneous Dengue and COVID-19 epidemics: Difficult days ahead? PLoS Negl Trop Dis. 2020;14(8) doi: 10.1371/journal.pntd.0008426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yacoub S., Wills B. Dengue: An update for clinicians working in non-endemic areas. Clin Med (Lond) 2015;15(1):82–85. doi: 10.7861/clinmedicine.15-1-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan G., Lee C.K., Lam L.T.M., Yan B., Chua Y.X., Lim A.Y.N., et al. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect Dis. 2020;20(5):536. doi: 10.1016/S1473-3099(20)30158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S., Fernandez A. Skin manifestations of COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc031. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]