Abstract
Lower limb crush injury is a major source of mortality and morbidity in trauma patients. Complications, especially surgical site infections (SSIs) are a major source of financial burden to the institute and to the patient as it delays rehabilitation. As such, every possible attempt should be made to reduce any complications. We, thus, aimed to compare the outcomes in early vs delayed closure of lower extremity stumps in cases of lower limb crush injury requiring amputation, so as to achieve best possible outcome. A randomised controlled study was conducted in the Division of Trauma Surgery & Critical Care at Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi from 1 September 2018 to 30 June 2019 and included patients undergoing lower limb amputation below hip joint. Patients were randomised in two groups, in one group amputation stump was closed primarily, while in the second group delayed primary closure of stump was performed. We compared rate of SSI, length of hospital stay, and number of surgeries in both the groups. Fifty‐six patients with 63 amputation stumps were recruited in the study. Mean age of patients in the study was 34 years, of which about 95% patients were males. The most common mechanism of injury was road traffic injury in 66% of patients. Mean injury severity score was 12.28 and four patients had diabetes preoperatively. Total 63 extremities were randomised with 30 cases in group I and 33 cases in group II as per computer‐generated random number. Above knee amputations was commonest (57.14%) followed by below knee amputations (33.3%). Two patients died in the current study. In group I, In‐hospital infection was detected in 7 cases (23.3%) and in group II 9 cases (27.3%) had SSI during hospital admission (P > .05). Mean hospital stay in group I was 10.32 ± 7.68 days and in group II was 11 ± 8.17 days (P > .05). Road traffic injuries and train‐associated injuries are a major cause of lower limb crush injuries, leading to limb loss. Delayed primary closure of such wounds requires extra number of surgical interventions than primary closure. There is no difference in extra number of surgical interventions required in both the groups. Thus, primary closure can be safely performed in patients undergoing lower limb amputations following trauma, provided that a good lavage and wound debridement is performed.
Keywords: amputation, crush injury, primary closure, trauma
1. INTRODUCTION
Trauma is the second most common indication for lower limb amputation with diabetes mellitus being the most common cause.1, 2 Trauma to lower extremities is common following Road traffic injuries, railway track injuries, and machine cut injuries. They may have an associated crush injury or vascular injury, which could mandate amputation. Such injuries lead to a poor outcome if treatment is delayed, as most of them are classified as dirty wounds owing to their mechanism of injuries. Crush injuries lead to life‐threatening infection and systemic complications in the form of crush syndrome and compartment syndrome. As such, timely amputation of the limb is necessary to save life in unsalvageable limbs or life‐threatening systemic complications of crush syndrome. However, surgical intervention has its own complications. Low et al reported a prevalence of 27.5% of post‐surgical complications in patients undergoing lower limb amputation following trauma.3 The most common complication was surgical site infections (SSIs), with reported rates ranging from 12% to 27%.4, 5, 6 SSIs have been a surgeon's nightmare ever since surgery was started. For decades, clinicians and researchers have been in search of different ways to reduce SSIs. Surgeons have witnessed the development of surgical gloves to the development of extensive operation rooms with an aseptic environment. However, the challenge of SSIs remains. SSIs are also a major source of morbidity in patients undergoing amputation as they delay rehabilitation and prosthesis placement.
Furthermore, it is also important to understand that SSIs are a major financial burden to an institute by raising both direct as well as indirect costs. Poulsen et al in 1994 showed that SSIs accounted for about 0.5% of annual hospital expenditure.7 Donald Fry noted that superficial SSIs cost about 400 dollars/case while deep/organ space infections cost about 30 000 dollars/case.8 Management of SSIs requires a multimodality approach in the form of antibiotics, surgical or chemical debridement, wound lavages, dressings, and application of Negative pressure wound therapy (NPWT). As such, it becomes important to know the optimum timing of stump closure following amputation for a better outcome. However, there are many studies that have been performed until now for primary closure (PC) or delayed primary closure (DPC) in the case of dirty abdominal wounds, but there is a paucity of studies comparing PC and DPC in the case of amputation stumps.9, 10 The timing of stump closure in performing amputation is not agreed upon and is decided on patient‐to‐patient basis or institutional protocols, which vary across hospital. Delayed closure would prolong hospital stay thus increasing costs while on the other hand early closure has risk of infection and non‐delineation of damaged skin. The optimal approach has not been prospectively studied in any study and remains unknown. We, therefore, aimed to prospectively compare the outcomes in early vs delayed closure of lower extremity stumps in cases of lower limb crush injury requiring amputation due to non‐salvageable limb or life‐threatening systemic complications.
2. METHODOLOGY
A randomised controlled study was conducted in the Division of Trauma Surgery & Critical Care at Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi from 1 September 2018 to 30 June 2019. Ours is a level 1 trauma centre with an annual footfall of about 75000 patients per year. In the Division of Trauma Surgery and Critical Care, the admission rate is about 1900 patients per year and about 150 amputations are performed annually for trauma. In the present study, we included patients of lower extremity injury with a non‐salvageable limb or life‐threatening complications of crush syndrome, planned for amputation either immediate or delayed of either gender or all ages, irrespective of other associated injuries. Each limb was considered separately as an isolated amputation with regard to SSI and number of surgical interventions. In patients undergoing bilateral amputations, right leg was counted as first number and left leg was randomised as next number. In consideration with the biostatistics department of the institute, a sample size of 60 amputations was decided who were further divided into two groups based on skin closure technique.
2.1. Exclusion criteria
The patient who did not give consent for the study.
The patient who underwent guillotine amputation.
Patients with an inadequate available skin cover.
Informed consent was taken from all patients (or their relatives) included in the study.
Patients presenting to the emergency department were triaged and resuscitated as per standard advanced trauma life support protocols. Clinical and epidemiological data of every patient were recorded in a preformed data set by a dedicated floor nurse and later transferred to an electronic database. Patients requiring amputation in index surgery were included and screened for any exclusion criteria. Once fit for recruitment in the study, informed consent was taken. A specific mention of higher amputation/shorter stump was taken and explained as a trade‐off against the possibility of multiple surgeries. The allocation was performed by a computer‐generated random number table and concealed with opaque envelopes. The patient was shifted to operation theatre and after proper anaesthesia, the best level of amputation was decided by the surgeon on table after complete debridement of all contused/crushed muscle and skin and removal of comminuted bone fragments. Muscles were divided at a level allowing skin closure without tension, as far as possible. Myoplasty was performed. At this point patient, was randomised and allocation was performed with computer‐generated random number table concealed with opaque envelopes. The envelope was opened by an independent member of team either floor nurse or anaesthesia team.
Patients were randomised in either of the two groups:
Patient in whom PC was performed.
Patient in whom stump left open for delayed stump closure (48‐72 hours).
Formal amputation stump was closed at a level where normal skeletal, musculotendinous, and fascio‐cutaneous tissues were available, as judged by gross examination. Below‐knee amputation flaps were made in a tapered, cylindrical fashion with a long posterior flap. Above‐knee amputation flaps were fashioned with either transverse or sagittal incisions depending on the surgeon's preference. A drain was kept in all the wounds undergoing PC. Semi‐permeable dressing with absorbent gauze was used for dressing (Figure 1). Broad‐spectrum antibiotics (Amoxicillin + clavulanic acid) were started preoperatively and continued postoperatively. If SSI was present, then culture‐based antibiotics were started.
Figure 1.

Intra‐operative pictures depicting various stages of stump closure. A, Myoplasty. B, Skin flaps (In group 2, these flaps were left as such and were approximated 48 to 72 hours later). C, Closure of skin flaps over a suction drain. D, Soft compression dressing over stump
In delayed closure, scheduled relook and closure was performed after 48 to 72 hours, as per operation room logistic. In the second surgery after debridement and thorough wash, delayed closure/revision amputation was performed. The closure was performed in layers with or without a drain.
The following characteristics were assessed in both groups:
Rate of SSI.
Length of hospital stay.
Number of surgeries in both the groups.
Healing was defined as complete epithelisation of the wound tract, as ascertained by lack of any raw area, granulation or discharge in suture line, minimal or no output in drain (if kept), and no expressible collection in the stump.
Follow‐up of patients was performed first at 7 ± 3 days of discharge or in first outpatient visit whichever was earlier and second follow‐up at 28 ± 7 days. In the follow‐up, stump examination was performed. SSI, healing of the wound, and local complications were noted. The study was approved by the Institutional Ethical Committee (IECPG‐379/30 August 2018).
2.2. Statistical analysis
Data were analysed using statistical package for social sciences (SPSS) version 21, IBM Inc. Descriptive data were reported for each variable. Descriptive statistics such as mean and standard deviation for continuous variables and frequency along with percentages of categorical variables were calculated. Summarised data were presented using tables and graphs. Shapiro Wilk test was used to check, in which all variables were following the normal distribution. Data were found to be normally distributed (P‐value was more than .05). Therefore, bivariate analyses were performed using the parametric tests, that is, independent t test (for comparing two independent groups). Chi‐square test and Fischer exact test were used for frequency analysis. The level of statistical significance was set at a P‐value of less than .05.
3. RESULTS
In the current study, a total of 63 extremities was included in 56 patients with seven bilateral amputations. Out of 56 patients, 3 (5.4%) were female and 53 (94.6%) were male with a mean age of 34.20 ± 12.59 years. The most common mechanism of injuries were road traffic injuries (66.1%) followed by train‐associated injuries (32.1%) (Table 1).
Table 1.
Epidemiological description of patients in the study
| Parameters | Group I (N = 30) | Group II (N = 33) | P value |
|---|---|---|---|
| Male: female | 28:2 | 32:1 | .5 |
| Mean age (y) | 35.6 ± 13.8 | 33.3 ± 13.1 | .5 |
| Mode of injury | |||
| RTI | 14 (46.7%) | 25 (75.8%) | .02 |
| Train‐associated injury | 16 (53.3%) | 7 (21.2%) | |
| Others | 0 | 1 (3%) | |
| Interval from injury to amputation | |||
| <48 h | 26 (86.6%) | 27 (81.8%) | .06 |
| >48 h‐1 wk | 3 (10.0%) | 5 (15.15) | |
| >1‐3 wk | 1 (3.3%) | 1 (3.0%) | |
| ISS | 12.9 ± 5.6 | 11.5 ± 4.8 | .3 |
| NISS | 16.1 ± 6.9 | 15.3 ± 5.8 | .6 |
| MESS score | 7.7 ± 2.2 | 7.1 ± 1.3 | .9 |
| Presence of shock on initial presentation | 6 (20.0%) | 4 (12.1%) | .3 |
| Other associated injury | |||
| Chest injuries | 1 (3.3%) | 2 (6.0%) | |
| Liver injury | 0 | 1 (3.0%) | |
| Bladder injury | 0 | 1 (3.0%) | |
| Pelvic fracture | 0 | 1 (3.0%) | |
| Diagnostic laparoscopy | 0 | 1 (3.0%) | |
| Comorbidity | |||
| Diabetes | 1 (3.3%) | 4 (12.1%) | .2 |
| COPD | 2 (6.7%) | 0 | |
| Hypertension | 0 | 1 (3.0%) | |
| Psychiatric disorder | 1 (3.3%) | 0 |
Abbreviations: COPD, chronic obstructive pulmonary disease; ISS, injury severity score; MESS, mangled extremity severity score; NISS, new injury severity score; RTI, road traffic injury.
Mean injury severity score was 12.28 ± 5.08 and mean new injury severity score 15.46 ± 6.4 and the scores were comparable between two groups (Figure 2).
Figure 2.
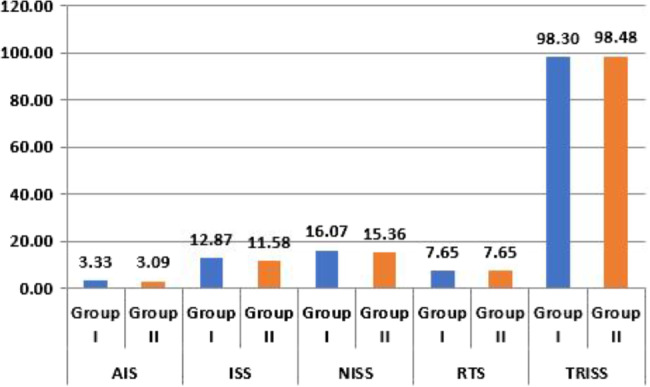
Injury scores in two groups
In group I, 30 amputations and in group II, 33 amputations were randomised. In group I, male: female ratio was 28:2 and group II was 32:1. In group I, mean age was 35.57 ± 13.885 and group II 33.33 ± 2.3. Among the mechanism of injury, In group I, train‐associated injuries were maximum (53.3%), followed by road traffic injuries (46.7%). In group II, road traffic injuries were more (75.8%) compared with train‐associated injuries (21.2%), and only one case of machine‐cut injury in group II. In group I, train‐associated injury was significantly high (P‐value <.05).
Out of 63 cases, 19 presented with already amputated or near‐total amputation stump. In group I, mean mangled extremity severity score (MESS) was 7.75 ± 2.245 and in group II it was 7.13 ± 1.254. In group I, cases presenting with initial features of shock were 6 (20%) and in group II, 4 cases (12.1%) presented with shock. All 10 cases responded to resuscitation. After stabilisation of vitals, parameter patients were shifted to the operation theatre for surgery. In group I, associated injuries were present in two cases (6.6%) and in group II five cases (15%) had other associated injuries.
Out of 63, 10 cases were initially tried for limb salvage then subsequently decided to undergo amputation. In group I, initial limb salvage was tried in 4 patients and in 6 patients in group II. For more than 2 weeks trial of limb salvage given for one patient in group I. In our study above‐knee amputation had the highest number (57.14%) followed by below‐knee amputations (33.33%). The distribution along the two groups was comparable and was not significant (Figure 3).
Figure 3.
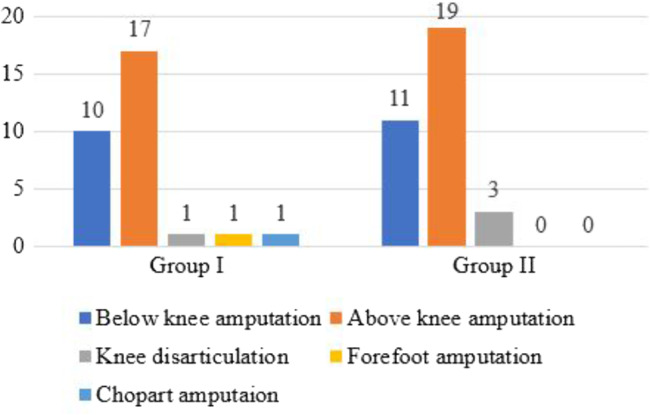
Distribution of types of amputation between two groups
Two patients (4.76%) expired, of which one patient had a bilateral amputation. However, none of them expired because of stump‐related illnesses. One of them died because of abdominal sepsis while second patient died because of cardiogenic shock, who was a known case of coronary artery disease.
Cases were further evaluated for SSI in the hospital, after 7 to 10 days of the discharge as per follow‐up and at 4 weeks of discharge. In group I, In‐hospital infection was detected in 7 cases (23.3%) and in group II 9 cases (27.3%) had SSI during hospital admission. In group I out of seven cases, three had deep SSI and In group II four cases had Deep SSI. At 1 week follow‐up in group I, three cases (10%) had SSI and in group II five cases (15.2%) had SSI. One patient of group II above‐knee amputee who had pus discharge with fever readmitted after 3 weeks and revision amputation was required for pus cavity just at the end of the femur bone.
We calculated the length of hospital stay in both groups. In our study, we excluded the patient in whom In‐hospital stay was increased because of other reasons. We also excluded the patients who were unknown and unattended. Mean hospital stay in group I was 10.32 ± 7.68 days and in group II was 11 ± 8.17 days. However, in group II, as expected because of delay PC, patients had a longer stay as compared to group I. In group I, total cases included for the comparison of length of hospital stay were 22 and in group II 23. In group I, cases that were discharged in 10 days of duration were 15 out of 22 and group II was 13 out of 23. Patients in group I who require more than 20 days stay were four, in one patient because of other limb foot injury require revision amputation after 2 weeks, in another one patient increase in hospital stay because of initial limb salvage then amputation after 7 days and other two patients require multiple debridements for SSIs increasing prolonged hospital stay. In group II, three patients stayed more than 20 days, one patient underwent initial fasciotomy and external fixation then subsequently requiring knee disarticulation, which got infected required grafting on a small area later, and other two patients required multiple surgeries and debridement because of SSI then followed by revision amputation prolonging hospital stay (Table 2).
Table 2.
Comparison of outcomes in two groups
| Parameters | Group I (N = 30) | Group II (N = 33) | P value |
|---|---|---|---|
| Mean length of hospital stay | 10.31 ± 7.68 | 11.0 ± 8.17 | .78 |
| 0‐5 d | 6 (20%) | 6 (18.18%) | .622 |
| 6‐10 d | 9 (30%) | 7 (21.21%) | |
| 11‐15 d | 3 (10%) | 5 (15.15%) | |
| 16‐20 d | 0 | 2 (6%) | |
| >20 d | 4 (13.3%) | 3 (9%) | |
| Length of stay (LOS) delay due to other reasons | 7 (23.3%) | 8 (24.245) | |
| Number of extra surgeries required | 6 (20.0%) | 5 (15.2%) | .403 |
| Revision higher up (one joint above) | 1 (3.0%) | 2 (6.0%) | .402 |
| Amputation revision (local revision) | 3 (10%) | 4 (12.12%) | .121 |
| Wound gapping with follow‐up | 1 (3.3%) | 2 (6.1%) | .610 |
| Surgical Site infection rate | |||
| In hospital infection | 7 (23.3%) | 9 (27.3%) | .474 |
| At 7 d follow up | 3 (10.0%) | 5 (15.2%) | .707 |
| At 4 wk follow up | 2 (6.7%) | 1 (3.0%) | .711 |
| Distribution according to outcome | .121 | ||
| Death | 1 (3.3%) | 2 (6.6%) | |
| Discharge | 29 (96.7%) | 31 (93.4%) |
We studied the extra number of surgeries that were required in both groups. The extra number of surgeries required in group I was 6 (20%) and in group II it was 5 (15.2%). The difference was not statistically significant.
Further, we studied the need for revision amputation in both groups. It was divided into two groups:
Local revision of bone: In group 1, it was performed in three cases, while in group II, it was performed in four cases.
Change of amputation level: In group I, only one case (3.0%) underwent revision from below‐knee amputation to above knee amputation. In group II, two cases required revision amputations, one case (3.0%) with Knee disarticulation underwent above‐knee amputation and one case (3.0) with below‐knee amputation revised to above‐knee amputation. The main cause for revision was deep SSI leading to wound gappng.
4. DISCUSSION
Amputations are a major source of morbidity. Any complication following an amputation delays rehabilitation and prosthesis placement. As such, it becomes important that the best possible outcome is achieved at the earliest. However, there is a huge void in the literature on optimum timing for the closure of amputation stumps, so as to avoid any infective complications. In the present study, we studied the impact of PC vs DPC in patients undergoing lower limb amputations following trauma.
The mean age for participants in the present study was 35.57 ± 13.88 in group I and in group II 33.33 ± 13.13 respectively. This is in concordance with the statement that “trauma is a disease of young.”11 The total number of males was 53 out of 56 in our study. This may be explained by the fact the injury burden in our country is predominantly absorbed by the male population. It is important especially in developing countries where the male population works more in the field and thus is exposed to the accidental hazard. Similar results were shown by Low et al3 who did a study in patients undergoing traumatic lower limb amputation. They found that the mean age was 42.3 years for males and 47.5 years for females with a male: Female ratio 4:1.Gandla Kiran Kumar et al4 studied the incidence and cause of lower limb amputation in a tertiary care centre. They included a total of 243 patients with a mean age group of 53.5 years with a male population of 81.89% and included both traumatic and nontraumatic amputations.
In the present study, the most common mechanism of injury was road traffic injuries (61.9%), followed by train‐associated injury (36.5%). Eric Edison Low et al3 found that the most common mechanism of injury was road traffic injuries (61.65%) followed by fall (8.02%). Road traffic injuries are by far the most common mechanism of injury in patients with crush injury lower limb. Train‐associated injury predominated more in group I (53.3%) as compared to group II (21.2%). Such a high incidence of train‐associated injuries may be because India is having one of the largest railway networks in the world. This suggests that stricter implementation of road traffic rules and railway protection rules is required to prevent these injuries (Table 3).
Table 3.
Comparison of epidemiological parameters of the current study with other studies
| Yasar et al21 | Low et al3 | Agha et al17 | Kumar4 | Maqsood et al6 | Current study | |
|---|---|---|---|---|---|---|
| Type of study | Retrospective | Retrospective | Prospective | Retrospective | Prospective | Randomised study |
| Year of study | January 2001‐December 2009 | January 2011‐December 2012 | May 2015‐April 2016 | June 2016‐May 2018 | December 2012‐October 2013 | September 2018‐June 2019 |
| Number (Extremities) | 399 | 2879 | 45 | 243 | 33 | 63 |
| Mean age (y) | 23 ± 6 | Male 42.3Female 47.5 | 66 | 53.5 | 43.5 | 34.4 |
| M: F | 398:1 | 4:1 | 29:16 | 4:1 | 5.7:1 | 20:1 |
| Study population | Traumatic | Traumatic | Traumatic + Non‐traumatic | Traumatic + Non‐traumatic | Traumatic + Non‐traumatic | Traumatic |
| Most common mechanism of injury | Landmine | RTI | NA | NA | RTI | RTI |
| Most common indication of amputation | Crush injury | Crush injury | Diabetes PAOD | Diabetes + PAOD | PAOD | Crush injury |
| Most common major amputation | BKA‐50.7% | BKA‐46% | AKA‐68.1% | BKA | BKA‐66.67% | AKA‐57% |
| AKA‐14.56% | AKA‐37.5% | BKA‐29.8% | AKA‐27.88% | BKA‐33% | ||
| Most common complications of amputation stump | Stump complications | NA | Wound infection (17.8%) | Wound infection 64 (26.33%) | Wound infection 4 (12.12%) | Wound infection 16 (25.39%) |
Abbreviation: AKA, above knee amputation; BKA, below knee amputation; PAOD, peripheral arterial occlusive disease; RTI, road traffic injury.
We further evaluated MESS scores in the study population. MESS scores have been utilised for long in identifying patients at risk for limb loss. Helfet et al first utilised this score in predicting the need for amputation in patients with lower extremity trauma. They found that MESS for salvaged limbs ranged from three to six, whereas the amputated limbs ranged from 7 to 12. The authors concluded that a MESS of seven or greater predicted amputation with 100% accuracy.12 In the present study, the mean MESS was seven. However, the minimum MESS score was four in a patient who underwent amputation and a total of 19 cases (10 in group I and 9 in group II) presented with already amputated/near‐total amputation status. Since its inception, MESS has been utilised extensively in trauma. However, in recent studies authors have not been able to achieve great accuracy and have developed alternative scoring systems. As per Loja et al,13 MESS of eight predicted in‐hospital amputation in only 43.2% of patients. During 2013 and 2015, 230 patients with lower extremity arterial injuries were recruited in the PROOVIT registry. MESS of eight or greater was associated with a longer stay in the hospital, 81.3% of limbs were ultimately salvaged and 18.7% required primary or secondary amputation. Menakuru et al found that of 148 patients, a MESS of >7 had a sensitivity of only 44% and a specificity of 70% in predicting amputation.14 Fodor et al concluded that MESS correctly identified the need for amputation in only 25% of cases,15 whereas Schiro et al found the range of reported accuracy of a MESS >7 to be anywhere between 0% and 93.4% in the literature.16 This decrease in accuracy of MESS from days of its introduction to now may be because of advancements made over the years in management and reconstruction of complex soft tissue injuries.
Further, we studied the most common amputation required. In the present study, above‐knee amputation (57%) was commonest, which is similar to a few studies. However, in the majority of the studies most common amputation was below‐knee. This difference is attributed to the level of injury with which the patient presented following trauma. Peripheral vascular diseases usually involve smaller vessels and the level of the amputation usually remains below the knee, while in trauma setting the level of amputation is dictated by the injury itself.
While studying the complications, we found SSIs being the most common in 25.4% of cases. The complication has been the most frequent one in other studies as well with Gandla et al reporting a similar rate.4 The rates were lower in studies by Maqsood et al and Agha et al, which may be attributed to the fact that their study population included both traumatic and non‐traumatic indications for amputation (Table 3).6, 17 Traumatic wounds, as has been discussed, are usually dirty owing to their mechanism of injury. Also, because trauma is an acute event, the patient's reserves may not be adequate, thus, slowing the healing process. However, we do believe that further studies are required to establish the differences in SSIs, if any, in traumatic and non‐traumatic population.
We further compared SSIs between PC and DPC groups. In the present study, the SSI during hospitalisation was detected in 7 (23%) cases in group I of which four were superficial and three were deep SSIs, while in group II, nine cases (27%) developed SSIs of which five were superficial and four were deep SSI. The difference between the two was not statistically significant. After an extensive literature search, we found that very few studies have been performed comparing PC with DPC in lower limb amputations. Further, the studies that have been performed comparing the two techniques are in patients with land mine injuries, wet gangrene, and critical limb ischemia (Table 4). Simper et al in a retrospective review of 106 cases following war injuries, studied complication rates of DPC. They found a 13% SSI rate and recommended DPC as a method of treatment. However, it was a retrospective review and there was no comparison group.18 Atesalp et al reviewed 474 cases of landmine injuries and compared PC with DPC. They found a slightly higher rate in the PC group when compared with DPC (87.4% vs 81.2%) but it was not statistically significant.5 However, Silva et al in a retrospective cohort study in 207 patients with critical limb ischemia showed significantly better SSI rates in the DPC group.19 This may be because of the fact that they included only critical limb ischemia patients in whom the vascular compromise impairs the healing process and is a frequent cause of wound dehiscence. Fischer et al randomised 47 patients with wet gangrene into PC and DPC groups. They found significantly better results with DPC.20 This difference between the present study and study by Fischer et al is attributed to the fact that Fischer et al did gulliotine amputation in the first stage followed by definite formal amputation at a later date, while in the present study we performed formal amputation at the first stage and left skin flaps open which were closed at a later date. Their study was also limited to patients with wet gangrene in whom there are higher chances of bloodstream infections, while in acutely injured patients setting up bloodstream infection would require time.
Table 4.
Table comparing outcomes of amputations in the different studies for delayed primary closure with present study
| Simper et al18 | Atesalp et al5 | Silva et al19 | Fisher et al20 | Maricevic et al22 | Current study | |
|---|---|---|---|---|---|---|
| Type of study | Retrospective | Retrospective | Nonrandomised retrospective cohort study | Prospective randomised | Retrospective | Randomised study |
| Study year | 1989 | 2004‐2011 | September 1984‐December 1986 | April 1992–1994 | September 2018‐June 2019 | |
| Mean age (y) | Young age | 22.1 | PC‐64.8 | PC‐67 | 26 | PC‐35.5 |
| DPC‐63.8 | DPC‐68.1 | DPC‐33.3 | ||||
| M:F ratio | All male | 471: 3 | PC‐61:45 | NA | 68:7 | PC‐28:2 |
| DPC‐62:39 | DPC‐32:1 | |||||
| Mechanism of injury | Explosion of mine Bomb blast Gunshot | Land mine injuries | Nontraumatic | Nontraumatic | War wounded | Trauma (RTI, train associated) |
| Study population | TraumaticBelow knee amputation | TraumaticBelow knee amputation | Critical limb ischemia | Wet gangrene | TraumaticAll extremities | TraumaticBelow hip joint |
| Total extremities included | 106 | 474 | 207 | 47 | 76 | 63 |
| Amputation stump closure (numbers) | PC‐NIL | PC‐392 | PC‐106 | PC‐24 | PC‐70 | PC‐30 |
| DPC‐106 | DPC‐82 | DPC‐101 | DPC‐23 | DPC‐6 | DPC‐33 | |
| Infection rate/complication of stump | PC‐87.4% | PC‐44.5% | PC‐21% | PC‐8 | PC‐23.3% | |
| DPC‐13% | DPC‐81.2% | DPC‐28.3% | DPC‐0% | DPC‐17 | DPC‐27.3% | |
| P value | NA | NA | 0.0006 | 0.05 | NA | 0.711 |
| Length of hospital stay (d) | NA | NA | PC‐16 | PC‐52.6 | NA | PC‐10.3 |
| DPC‐25 | DPC‐37.6 | DPC‐11 |
Abbreviations: DPC, delayed primary closure; PC, primary closure; RTI, road traffic injury.
Complications following amputation are a major concern as they affect financially as well, with increased demand for resources. We, in the present study, further studied the requirement for additional surgeries in the form of the need for debridement and revision amputations after stump complications. The number of additional surgeries required was comparable in both the groups and was not statistically significant (20% vs 15.2%; P − .4). However, it is important to note that patients who undergo DPC would require at least two surgeries, while PC would require only one surgery if there are no associated complications. This adds to a financial burden to the institute and to the patient.
Similarly, the requirement for revision amputations was also not different statistically (10% vs 12%; P − .1). This is in concordance with the study by Simper et al who reported a revision amputation rate of 13% in the DPC group.18 Another important modality in the treatment, which has risen up fast in management of complex soft tissue wounds, is NPWT. Its effectiveness has been established beyond doubt, but it does add up significantly to treatment costs. In the present study, five patients required NPWT during the course of their treatment. However, the results of NPWT continue to be encouraging and if there are no cost issues, its use in management of complex wounds needs to be promoted.
While comparing the length of hospital stay between the two groups, we did not find any statistically significant difference (10.3 vs 11 days; P − .78). Silva et al showed a longer stay in the DPC group when compared with the PC group (25 vs 16 days); however, it was statistically not significant. Furthermore, we need to remain aware of the fact that patients with the DPC group had to stay for 2 to 3 days more than the PC group, as they have to undergo mandatory second surgery 48 hours later. This suggests that this technique does not impose financial burden on the institute or to the patient in terms of hospital stay. However, our sample size is small and we would recommend further studies and cost analysis for drawing a definitive conclusion on this aspect. In the present study, the mortality rate was 4% (2/56). Two patients succumbed to their illness. One patient died because of other associated injury and while the second patient died because of associated heart disease coronary artery disease. The mortality rate of the current study is in concordance with other studies, who report a mortality rate of 5% to 10%.
The present study does have its own limitations. Larger sample size would have increased the strength and accuracy. Surgeon to surgeon variations in techniques was not considered. Also, cost analysis between the two groups could have given more insight into the overall advantage of either technique.
To conclude, road traffic injuries and train‐associated injuries are a major cause of lower limb crush injuries, leading to limb loss. It is important as this affects the young population of the country. There is no statistically significant difference in rates of SSIs and length of stay in primary vs delayed PC in patients undergoing lower limb amputation following trauma. There is no difference in the extra number of surgical interventions required in both groups. However, the DPC group has an inherent requirement of two surgeries while the PC group requires only one surgery if there is no complication. Thus, PC can be safely performed in patients undergoing lower limb amputations following trauma, provided that a good lavage and wound debridement is performed.
Abbreviations
- AIS
abbreviated injury score
- DPC
delayed primary closure
- ISS
injury severity score
- MESS
mangled extremity severity score
- NISS
new injury severity score
- NPWT
negative pressure wound therapy
- PC
primary closure
- RTS
revised trauma score
- SSI
surgical site infection
- TRISS
trauma and injury severity score
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Katiyar AK, Agarwal H, Priyadarshini P, et al. Primary vs delayed primary closure in patients undergoing lower limb amputation following trauma: A randomised control study. Int Wound J. 2020;17:419–428. 10.1111/iwj.13288
REFERENCES
- 1. Abang IE. Indications and pattern of limb amputation: a tertiary hospital experience, South‐South. Nigeria Recent Adv Biol Med. 2018;4(2018):41‐45. [Google Scholar]
- 2. Kayssi A, de Mestral C, Forbes TL, Roche‐Nagle G. A Canadian population‐based description of the indications for lower‐extremity amputations and outcomes. Can J Surg. 2016;59(2):99‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Low EE, Inkellis E, Morshed S. Complications and revision amputation following trauma‐related lower limb loss. Injury. 2017;48(2):364‐370. [DOI] [PubMed] [Google Scholar]
- 4. Kumar GK, Souza CD, Diaz EAI. Incidence and causes of lower‐limb amputations in a tertiary care center: evaluation of the medical records in a period of 2 years. Int J Surg. 2018;2(3):16‐19. [Google Scholar]
- 5. Ateşalp AS, Erler K, Gür E, Solakoglu C. Below‐knee amputations as a result of land‐mine injuries: comparison of primary closure versus delayed. J Trauma. 1999;47(4):724‐727. [DOI] [PubMed] [Google Scholar]
- 6. Maqsood M, Ali N, Bhat A, Bangroo FA, Dhanda MS, Singh R. Current trends of major lower limb amputations at a tertiary care centre of Jammu, India. Int J Med Sci Res Pract. 2015;2(2):77‐80. [Google Scholar]
- 7. Poulsen KB, Bremmelgaard A, Sørensen AI, Raahave D, Petersen JV. Estimated costs of postoperative wound infections: a case‐control study of marginal hospital and social security costs. Epidemiol Infect. 1994;113(2):283‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fry DE. The economic costs of surgical site infection. Surg Infect (Larchmt). 2002;3(suppl 1):S37‐S43. [DOI] [PubMed] [Google Scholar]
- 9. Duttaroy DD, Jitendra J, Duttaroy B, et al. Management strategy for dirty abdominal incisions: primary or delayed primary closure? A randomized trial. Surg Infect (Larchmt). 2009;10(2):129‐136. [DOI] [PubMed] [Google Scholar]
- 10. Siribumrungwong B, Chantip A, Noorit P, et al. Comparison of superficial surgical site infection between delayed primary versus primary wound closure in complicated appendicitis. Ann Surg. 2018;267(4):631‐637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pooja GD, Sangeeta L. Prevalence and aetiology of amputation in Kolkata, India: a retrospective analysis. Hong Kong Physiother J. 2013;31(1):36‐40. [Google Scholar]
- 12. Helfet DL, Howey T, Sanders R, Johansen K. Limb salvage versus amputation. Preliminary results of the mangled extremity severity score. Clin Orthop Relat Res. 1990;256:80‐86. [PubMed] [Google Scholar]
- 13. Loja MN, Sammann A, DuBose J, et al. The mangled extremity score and amputation: time for a revision. J Trauma Acute Care Surg. 2017;82(3):518‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Menakuru SR, Behera A, Jindal R, Kaman L, Doley R, Venkatesan R. Extremity vascular trauma in civilian population: a seven‐year review from North India. Injury. 2005;36(3):400‐406. [DOI] [PubMed] [Google Scholar]
- 15. Fodor L, Sobec R, Sita‐Alb L, Fodor M, Ciuce C. Mangled lower extremity: can we trust the amputation scores? Int J Burns Trauma. 2012;2(1):51‐58. [PMC free article] [PubMed] [Google Scholar]
- 16. Schirò GR, Sessa S, Piccioli A, Maccauro G. Primary amputation vs limb salvage in mangled extremity: a systematic review of the current scoring system. BMC Musculoskelet Disord. 2015;16(1):372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Agha RA, Muneer H, Alqaseer A, Ismaeel T, Badr O. Major lower limb amputation: causes, characteristics and complications. Bahrain Med Bull. 2017;39(3):159‐161. [Google Scholar]
- 18. Simper LB. Below knee amputation in war surgery: a review of 111 amputations with delayed primary closure. J Trauma. 1993;34(1):96‐98. [PubMed] [Google Scholar]
- 19. Silva LR, Fernandes GM, Morales NU, et al. Results of one‐stage or staged amputations of lower limbs consequent to critical limb ischemia and infection. Ann Vasc Surg. 2018;46:218‐225. [DOI] [PubMed] [Google Scholar]
- 20. Fisher DF, Clagett GP, Fry RE, Humble TH, Fry WJ. One‐stage versus two‐stage amputation for wet gangrene of the lower extremity: a randomized study. J Vasc Surg. 1988;8(4):428‐433. [PubMed] [Google Scholar]
- 21. Yaşar E, Tok F, Kesikburun S, et al. Epidemiologic data of trauma‐related lower limb amputees: a single center 10‐year experience. Injury. 2017;48(2):349‐352. [DOI] [PubMed] [Google Scholar]
- 22. Maricevic A, Erceg M, Gekic K. Primary wound closure in war amputations of the limbs. Int Orthop. 1998;21(6):364‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]


