Abstract
This literature review was conducted to summarise empirical evidence relating to psychosocial health following ostomy surgery during hospitalisation and after discharge. Both qualitative and quantitative studies were searched from 2000 to 2017 using PubMed, CINAHL, Ebrary, Elsevier, Science Direct, and Scopus. Twenty‐seven articles were included that examined the patient's psychosocial health following colostomy or ileostomy surgery. Among the 27 included studies, 11 adopted qualitative research methods and 16 used quantitative designs. Most of the studies were conducted to determine psychosocial problems and emotions of the individuals, their adaptation to the stoma, and their quality of life. Most of the psychosocial problems identified in these studies were poor body image perception and self‐respect, depression, sexual problems, and lower psychosocial adaptation. This literature review has illustrated the patient's psychosocial health following stoma surgery. Further studies exploring the effect of psychosocial interventions could be planned.
Keywords: psychosocial problems, qualitative, quantitative, research, stoma
1. INTRODUCTION
Stomas are formed surgically, by exteriorising the bowel to the abdominal surface. Every year, stoma is created for the surgical treatment of conditions such as colorectal cancer, inflammatory bowel disease, colorectal, and trauma. The exact incidence and prevalence of ostomy surgery is unknown. One report stated that there is an estimated range of 650 000 to 730 000 people live with a permanent ostomy in the United States.1
Stoma formation can prolong the lives of patients and help them to return to a healthy life. However, this process may cause the individual to experience various problems in terms of physiological, social, and psychological aspects. Individuals with stoma experience psychological problems such as depression, anxiety, changes in body image, low self‐esteem, sexual problems, denial, loneliness, hopelessness, and stigmatisation.2, 3 Social problems are that loss of interest and less participation in social activities, avoidance of travelling, decreased working activities, worsening partner relationship, decreased contact with friends/relatives.2, 3 These problems can adversely affect the individual's adaptation to stoma and ability to deal with stoma.
As colorectal cancer tends to have a better outcome and is associated with less morbidity than malignant disease at other sites (e.g., stomach, lungs, and liver), psychosocial status is particularly important. Psychosocial adaptation is also positively associated with quality of life. The studies show that individuals with stoma have their qualities of life negatively affected because of physiological and social issues.4, 5, 6, 7, 8 Therefore, to increase the quality of life for an individual with a stoma, resolving psychosocial issues as well as physiological issues and establishing adaptation to the stoma are required. When the literature is reviewed, it can be seen that research on the psychosocial issues of individuals with stoma began approximately 50 years ago. Despite this fact, patients still have issues in dealing with psychosocial problems.
This literature review was conducted to summarise empirical evidence relating to psychosocial health following colostomy or ileostomy surgery during hospitalisation and after discharge. The study questions were as follows:
What are the most common psychosocial problems?
Which factors did affect psychosocial adaptation to ostomy?
Which measurement tools were the most used in determining psychosocial problems?
Is there any difference between qualitative and quantitative studies?
2. METHODS
A literature review including both qualitative and quantitative studies was performed. The literature was searched from 2000 to 2017 using PubMed, CINAHL, Ebrary, Elsevier, Science Direct, and Scopus with the following MESH search terms: psychosocial problems and ostomy. Related search terms in all fields were “psychological problems, social problems, ostomy, stoma, ileostomy, colostomy, quality of life.” The studies that are regularly published on databases, that are edited and can be accessed electronically as well as those accessible via the archives of scientific journals were reviewed. The searches were carried out in April 2018 by the researcher. The studies from 2000 to 2017 were included and evaluated.
Inclusion criteria were: (a) be related to psychosocial problems, (b) published between 2000 and 2017, (c) be research article, (d) using descriptive or cross‐sectional or prospective designs, (e) be written in English, and (f) available in full length. Exclusion criteria were: (a) be written in different languages, (b) using methodological or experimental designs on psychosocial problems, (c) be review article, and (d) using quality of life scale to measure psychological dimensions.
3. RESULTS
The computerised database searches identified a total of 1274 studies. The author reviewed 84 studies and excluded 57 studies that did not meet eligibility criteria. Subsequently, 27 full‐text articles were retrieved and reviewed. Articles having no full text (n = 7), not written in English (n = 8), being review article (n = 16), using methodological or experimental research design on psychosocial problems (n = 9), and using quality of life scale to measure psychological dimensions (n = 8), and not addressing the psychosocial problems (n = 9) were excluded. Twenty‐seven articles were included that examined the patient's psychosocial health following colostomy or ileostomy surgery (Figure 1). Among the 27 included studies, 11 adopted qualitative research methods and 16 used quantitative designs. Sample sizes of qualitative designs ranged from 7 to 30, whereas those of quantitative designs ranged from 50 to 209.
Figure 1.
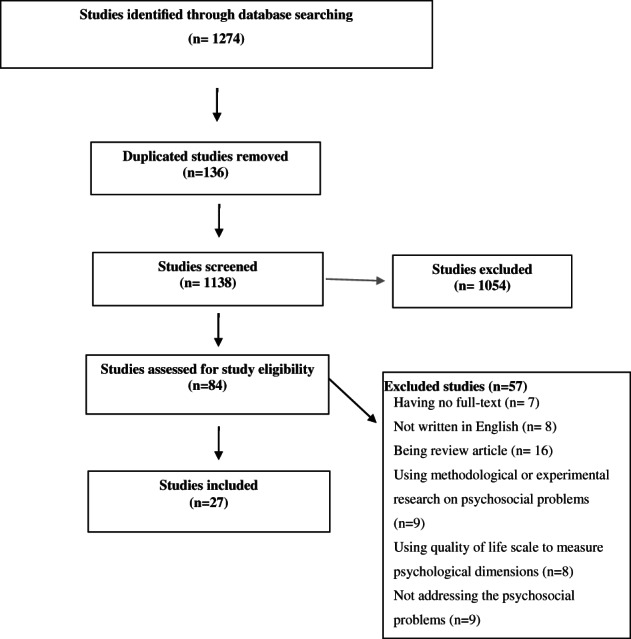
Flow chart
In qualitative studies, participant postoperative recovery experiences were elicited via one‐on‐one, open‐ended, conversational interview, in‐depth interviews, unstructured interviews, semistructured interviews or focus group interviews, or informal, unstructured, and audiotaped interview. In quantitative studies, self‐reported questionnaires and scales were used such as psychosocial adjustment scale, ostomy adjustment inventory, body image scale, self‐esteem scale, and anxiety and depression scale for data collection.
3.1. Findings of qualitative studies
The findings of four qualitative studies show that participants explained different feelings after stoma creation such as uncontrollable feelings of uncertainty, feelings of stigma, being different and having decreased self‐respect and confidence, and feeling frustrated and helpless. Also, living with uncertainty also influenced social life of the subjects. On the other hand, altered body image was another problem that was identified in two qualitative studies. According to these studies, stoma formation altered the body in terms of appearance, function, and sensation, undermining the unity between body and self. Participants believed that their attractiveness had decreased since surgery and expressed emotional distress when recalling personal feelings around their altered body appearance. Also, studies reviewed above found that altered body image can result in sexual problems. In one study, some of the participants believed that the ileostomy negatively affected their body image and sexual life. Persons with new ostomies expressed fear that their spouses would be disturbed by the physical changes in their body; they further reported loss of libido in one study. Another study found that some patients did not believe strong enough, and some did not yet believe any desire. One study showed that experiences of acceptance of intimate partners and understanding in general terms were mirrored in confidence of participants to resume sexual relationships. One study did highlight sexual problems amongst participants, especially in the early period after surgery and stoma formation. In addition to other issues, social relations and support from partner of family were found important in five studies. One of them found that provision or withdrawal of support of husbands or partners can have a considerable impact on the psychosocial adjustment of female patients with ostomies. In other study, participants described support received from family members and linked this support to improved adaptation to their ostomy. A study found that stoma‐forming surgery changes the way an individual relates to their social environment and connects with others, creating self‐consciousness and impeding social confidence and autonomy. The other study showed that patients had some degree of cognitive and mental problems that they were concerned about and also participants reported having encountered family problems for a few months after their colostomy.
3.2. Findings of quantitative studies
Among quantitative studies, psychosocial problems such as anxiety, depression, poor body image, and impairment in social relations were determined in eight studies. One study found that 50% of patients with stoma reported higher than normal levels of anxiety and 16% reported mild to moderate levels of depression. Although persons living with a stoma are at risk of experiencing anxiety and depression, most were not receiving psychological support in another study. Also, one study found that a stoma is an intervention in the patient's social and intimate life and patients cope with the situation very slowly and very painfully. Another study found that work and social function were influenced by hope, skills, gender, and education. In addition, one study found that patients experiencing physical and psychosocial problems had poor body image than those of patients who did not experience such problems. On the other hand, creation of an ostomy leads to a significant change in the body image of the patient in two studies (Table 1).
Table 1.
Quantitative studies related to psychosocial problems of patients with stoma
| Authors | Year | Study design | Aims of study | Results of study |
|---|---|---|---|---|
| Mäkelä and Niskasaari | 2006 | Descriptive | To evaluate the problems faced by those with permanent stomas and to survey patient satisfaction and quality of life of patients | Some of the patients (42%) had sexual problems such as impotence, dyspareunia, and frigidity and 34% of patients not adapted to their stoma. Of the non‐adapted patients, some of the non‐adapted patients did not accept the altered body image and had problems in social life. |
| General mental health was worse in 34% patients, and social functioning had deteriorated in 42% patients after stoma surgery. | ||||
| Simmons et al | 2007 | Descriptive | To examine adjustment and its relationship with stoma acceptance and social interaction, and the link between stoma care self‐efficacy and adjustment | Stoma care, self‐efficacy, stoma acceptance, interpersonal relationship, and the location of the stoma were strongly associated with adjustment. |
| Cotrim and Pereira | 2008 | Descriptive, cross‐sectional study | To identify and assess the impact of colorectal cancer on colorectal cancer patients and their families | The stoma patients also had significantly higher depression and anxiety, and poorer sexual activity than non‐stoma patients. |
| Kılıç et al | 2009 | Descriptive | To investigate the effects of permanent ostomy on body image, sexual functioning, self‐esteem, and marital adjustment | Permanent ostomy caused impairment in perceived body image, dyadic adjustment, and sexual functioning (touch, avoidance, and satisfaction, vaginismus, anorgasmy). |
| Michálková | 2010 | Descriptive | To ascertain the most frequent psychosocial needs of ostomates | A stoma is an intervention in the ostomate's social and sexual life. The client copes with the situation very slowly and very painfully. |
| Sharpe et al | 2011 | Prospective | To investigate the effect of having a stoma on body image in patients with colorectal cancer and to determine whether disturbances in body image predicted distress | Stoma patients showed more body image disturbance at the baseline. Body image was a strong predictor of initial levels of anxiety, depression, and distress and subsequent anxiety and distress. |
| Li et al | 2012 | Descriptive, cross‐sectional, exploratory | To explore the relationships among demographic and clinical characteristics, spiritual well‐being, and psychosocial adjustment | The study found that spiritual well‐being was significantly related to the quality of adjustment of patients to life after colostomy surgery, and adjustments in sexual relationships tended to be poor. |
| Knowless et al | 2013 | Descriptive, cross‐sectional | To explore illness perceptions and coping style, anxiety, depression, and health related quality of life in persons with Crohn's disease | Persons living with a stoma are at risk of experiencing anxiety and depression, and of having an impaired quality of life (specifically, sexuality and body image, work and social functioning). Despite the high prevalence of anxiety or depression in this study, most were not receiving psychological support. |
| Knowless et al | 2013 | Descriptive, cross‐sectional | To characterise the mediators of anxiety and depression in an inflammatory bowel disease stoma cohort | Fifty percent reported higher than normal levels of anxiety and 16% reporting mild to moderate levels of depression. |
| Cheng et al | 2013 | Descriptive | To assess ostomy knowledge, self‐care ability, and psychosocial adjustment in Chinese patients with a permanent colostomy and to investigate the correlation among these three characteristics | Patients with higher levels of knowledge about stoma care and those who can manage all aspects of care independently were more psychosocially adjusted to their stomas than persons with less knowledge and more dependence on others for care. |
| Liao and Qin | 2014 | Descriptive | To determine the level of stoma‐specific quality of life and to determine which factors associate with stoma‐specific quality of life among patients with a stoma | Stoma patients experienced difficulties functioning in work and social situations, with sexuality and body image. Hope and skills were also shown to be predictors of work/social function. Hope is positively correlated with quality of life. |
| Hu et al | 2014 | Cross‐sectional | To evaluate persons living with a colostomy to characterise and describe relationships among adjustment, self‐care ability, and social support | Overall adjustment to a colostomy was moderate. |
| Self‐care ability and social support of patients were positively correlated with the adjustment level. | ||||
| Aktas and Gocmen Baykara | 2015 | Descriptive, cross‐sectional | To assess the effect of the stoma on self‐image and partner perception | More than half of the patients with stoma (60.0%) encountered psychosocial problems such as (anxiety, refraining from sexual intercourse, depression, decrease in self‐confidence, avoidance of social activities, and staying away from friends. Patients experiencing physical and psychosocial problems had poor body image than those of patients who did not experience such problems. |
| Karadağ et al | 2015 | Prospective | To assess adaptation among patients > 18 years of age with a new temporary or permanent colostomy or ileostomy living in Turkey and receiving care at a participating stomatherapy unit | Many factors, such as preoperative information, the ability to perform care, and countermeasures against stomal and peristomal complications, and influence adjustment. |
| Gautam and Poudel | 2016 | Descriptive cross sectional | To determine the effect of gender on psychosocial adjustment of colorectal cancer survivors with ostomy | Both men and women had significant impairment in the psychosocial adjustment, however, men had significantly lower psychosocial adjustment score. |
| Jayarajah and Samarasekera | 2017 | An analytical cross‐sectional | To identify the factors that influence adaptation to altered body image | The mean body image disturbance questionnaire score was 2.22 ± 0.88 (range, 1‐5). Of the participants, 17.07% had mean body image disturbance higher than 3. |
Another common problem identified in quantitative studies was adjustment problems (n = 8). Five of these studies found that patients with stoma have adjustment problems. On the other hand, one study found that spiritual well‐being was significantly related to the quality of adjustment of patients to life after colostomy surgery. In another study, many factors, such as preoperative information, the ability to perform care, and countermeasures against stomal and peristomal complications, influence adjustment. In addition, one study found that patients with higher levels of knowledge about stoma care and those who can manage all aspects of care independently were more psychosocially adjusted to their stomas (Table 1).
Finally, sexual problems were important psychosocial problems for these people in some of the quantitative studies (n = 8). Stoma is a serious life situation for the individual and causes sexual problems. According to these studies, stoma patients had sexual problems such as impotence, dyspareunia, frigidity, refraining from sexual intercourse and experienced difficulties in sexual functioning (touch, avoidance, and satisfaction, vaginismus, and anorgasmy), and their adjustments in sexual relationships tended to be poor. Also, stoma patients had poorer sexual activity than non‐stoma patients (Table 1).
4. DISCUSSION
Psychological problems such as depression, anxiety, changes in body image, low self‐esteem, feelings of uncertainty, and social problems such as less participation in social activities, decreased working activities, decreased contact with friends / relatives, and sexual problems can adversely affect the individual's adaptation to stoma and ability to deal. To increase the life quality of patients with a stoma, psychosocial problems should be considered.2, 3
Via qualitative research studies, it can be possible to access in‐depth information regarding the psychosocial problems of individuals with stomas. In this literature review, 11 of the studies were qualitative.9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 These studies examined the relationship between stoma and psychological problems such as adaptation problems, feelings of uncertainty and stigma, and identified the effects of stomas on body image, sexuality, and social life, and showed the necessity to provide individualised training, consultancy, and psychosocial support. In particular, conducting qualitative research that examines the emotions and opinions of individuals in‐depth is considered to be a significant step. It is thought that qualitative studies are observed to play a guiding role in planning interventions towards the psychosocial problems of the patients with stoma.
From 2000s to this day, various quantitative studies conducted using descriptive, cross‐sectional, and prospective designs showed the psychosocial problems of individuals with stomas and their adaptation. Psychosocial problems identified in these studies were that poor body image perception and self‐respect, anxiety and depression,6, 20, 21, 22, 23, 24 influenced coping,25 lower psychosocial adaptation26, 27, 28, 29, 30, 31, 32, 33, and sexual dysfunction or sexual problems such as impotence, dyspareunia, frigidity, and refraining from sexual intercourse.6, 20, 21, 22, 23, 31, 33 Studies that examine the psychosocial problems and adaptation of individuals with stoma regarded as positive progress.
This literature review showed that there are numerous qualitative and quantitative studies on psychosocial problems of patients with stoma. Quantitative and qualitative research methods complement each other because they generate different types of knowledge that are useful.34 Several psychosocial problems were identified after stoma surgery in these quantitative and qualitative studies. It is thought that human emotions are difficult to quantify, so qualitative research seems to be a more effective method of investigating emotional responses deeply than quantitative research.
Qualitative researchers believe that truth is complex and dynamic and can be found only by studying people as they interact with and in their sociohistorical settings.34 In qualitative studies, feelings of the patients, life experiences, and meaning of them was described in‐depth after stoma. Therefore, it is thought that the real feelings of patients after stoma creation are shown by qualitative studies. On the other hand, quantitative research studies provide advantages by the large size of samples.
The increase in the number of studies on psychosocial health of individuals with stoma in recent years and the use of different methods in these studies can both be regarded as positive developments. However, in the literature, the interventional studies to solve psychosocial problems of individuals with stoma are limited in number.7, 35, 36 Therefore, it is thought that interventions towards resolving individuals' psychosocial problems are being ignored/neglected.
Health professionals often focus on only the physical problems of the patients and possibly neglect psychosocial needs. Certain interventions such as relaxation training, supportive group therapy, cognitive‐behavioural therapy, emotional and social support, general interactional skills like supportive communication, and listening and counselling can be applied to solve and prevent psychosocial problems.7, 37 For continuous care of patients with stoma after hospital discharge, the role of the health professionals becomes important. Health professionals especially nurses could provide appropriate interventions and educate patients on stoma care following surgery, help to create social platforms such as stoma support groups and be consultant to solve psychosocial problems.
There are some limitations of the study. Most of the studies conducted between 1960 and 2000 cannot be accessed. Another limitation is that the social and psychological well‐being of the patients is evaluated with quality of life scales. Therefore, these studies were not reviewed.
5. CONCLUSION
This literature review has illustrated the patient psychosocial health following stoma surgery. Psychosocial problems associated with stoma formation commonly identified in quantitative studies were anxiety, depression, poor body image, sexual problems, impairment in social relations, and adjustment problems. In qualitative studies, different feelings such as uncertainty, stigma, being frustrated, being different, and altered body image were explained after stoma creation. In addition to these feelings, social relations and support from partner of family were found to be important. It is estimated that more patients will likely suffer from psychological problems related to stoma surgery in the future. Based on the results of this literature review, health professionals could provide psychosocial care by implementing interventions to solve psychosocial problems of patients following stoma surgery. Further studies exploring the effect of psychosocial interventions could be planned.
Ayaz‐Alkaya S. Overview of psychosocial problems in individuals with stoma: A review of literature. Int Wound J. 2019;16:243–249. 10.1111/iwj.13018
REFERENCES
- 1. Cooke C. American ostomy census: counting surgeries and ostomy patients in the US. Phoenix. 2009;5:28‐29. 63, 67. [Google Scholar]
- 2. Ayaz S. Approach to sexual problems of patients with stoma by PLISSIT Model: An Alternative. Sex Disabil. 2009;27:81‐71. [Google Scholar]
- 3. Borwell B. Continuity of care for the stoma patient: psychological considerations. Br J Community Nurs. 2009;14:326‐331. [DOI] [PubMed] [Google Scholar]
- 4. Anaraki F, Vafaie M, Behboo R, Maghsoodi N, Esmaeilpour S, Safaee A. Quality of life outcomes in patients living with stoma. Indian J Palliat Care. 2013;18:176‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Knowles SR, Wilson J, Wilkinson A, et al. Psychological well‐being and quality of life in Crohn's disease patients with an ostomy: a preliminary investigation. J Wound Ostomy Continence Nurs. 2013;46:623‐629. [DOI] [PubMed] [Google Scholar]
- 6. Liao C, Qin Y. Factors associated with stoma quality of life among stoma patients. Int J Nurs Sci. 2014;1:196‐201. [Google Scholar]
- 7. Koplin G, Müller V, Heise G, Pratschke J, Schwenk W, Haase O. Effects of psychological interventions and patients' affect on short‐term quality of life in patients undergoing colorectal surgery. Cancer Med. 2016;5:1502‐1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Iqbal F, Kujan O, Bowley DM, Keighley MR, Vaizey CJ. Quality of life after ostomy surgery in muslim patients: a systematic review of the literature and suggestions for clinical practice. J Wound Ostomy Continence Nurs. 2016;43:385‐391. [DOI] [PubMed] [Google Scholar]
- 9. Altschuler A, Ramirez M, Grant M, et al. The influence of husbands' or male partners' support on women's psychosocial adjustment to having an ostomy resulting from colorectal cancer. J Wound Ostomy Continence Nurs. 2009;36:299‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dabirian A, Yaghmaei F, Rassouli M, Tafreshi MZ. Quality of life in ostomy patients: a qualitative study. Patient Prefer Adherence. 2011;5:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Danielsen AK, Soerensen EE, Burcharth K, Rosenberg J. Impact of a temporary stoma on patients' everyday lives: feelings of uncertainty while waiting for closure of the stoma. J Clin Nurs. 2013;22:1343‐1352. [DOI] [PubMed] [Google Scholar]
- 12. Cengiz B, Bahar Z. Perceived barriers and home care needs when adapting to a fecal ostomy. J Wound Ostomy Continence Nurs. 2017;44:63‐68. [DOI] [PubMed] [Google Scholar]
- 13. Danielsen AK, Soerensen EE, Burcharth K, Rosenberg J. Learning to live with a permanent intestinal ostomy: impact on everyday life and educational needs. J Wound Ostomy Continence Nurs. 2013;40:407‐412. [DOI] [PubMed] [Google Scholar]
- 14. Persson E, Hellström AL. Experiences of Swedish men and women 6 to 12 weeks after ostomy surgery. J Wound Ostomy Continence Nurs. 2002;29:103‐108. [DOI] [PubMed] [Google Scholar]
- 15. Sinclair LG. Young adults with permanent ileostomies experiences during the first 4 years after surgery. J Wound Ostomy Continence Nurs. 2009;36:306‐316. [DOI] [PubMed] [Google Scholar]
- 16. Thorpe G, McArthur M. Social adaptation following intestinal stoma formation in people living at home: a longitudinal phenomenological study. Disabil Rehabil. 2017;39:2286‐2293. [DOI] [PubMed] [Google Scholar]
- 17. Thorpe G, Arthur A, McArthur M. Adjusting to bodily change following stoma formation: a phenomenological study. Disabil Rehabil. 2016;38:1791‐1802. [DOI] [PubMed] [Google Scholar]
- 18. Savard J, Woodgate R. Young peoples' experience of living with ulcerative colitis and an ostomy. Gastroenterol Nurs. 2009;32:33‐41. [DOI] [PubMed] [Google Scholar]
- 19. Lim SH, Chan SWC, He HG. Patients' experiences of performing self‐care of stomas in the initial postoperative period. Cancer Nurs. 2015;38:185‐193. [DOI] [PubMed] [Google Scholar]
- 20. Aktas D, Gocmen Baykara Z. Body image perceptions of persons with a stoma and their partners: a descriptive, cross‐sectional study. Ostomy Wound Manage. 2015;61:26‐40. [PubMed] [Google Scholar]
- 21. Cotrim H, Pereira G. Impact of colorectal cancer on patient and family: implications for care. Eur J Oncol Nurs. 2008;12:217‐226. [DOI] [PubMed] [Google Scholar]
- 22. Kılıç E, Taycan O, Belli KA, Ozmen M. The effect of permanent ostomy on body image, self‐esteem, marital adjustment, and sexual functioning. Turk Psikiyatri Derg. 2007;18:302‐310. [PubMed] [Google Scholar]
- 23. Michálková H. Psychosocial problems of stoma clients. J Nurs Soc Stud Public Health. 2010;1:62‐70. [Google Scholar]
- 24. Sharpe L, Patel D, Clarke S. The relationship between body image disturbance and distress in colorectal cancer patients with and without stomas. J Psychosom Res. 2011;70:395‐402. [DOI] [PubMed] [Google Scholar]
- 25. Knowles SR, Cook SI, Tribbick D. Relationship between health status, illness perceptions, coping strategies and psychological morbidity: a preliminary study with IBD stoma patients. J Crohns Colitis. 2013;7:e471‐e478. [DOI] [PubMed] [Google Scholar]
- 26. Cheng F, Meng AF, Yang LF, Zhang YN. The correlation between ostomy knowledge and self‐care ability with psychosocial adjustment in Chinese patients with a permanent colostomy: a descriptive study. Ostomy Wound Manage. 2013;59:35‐38. [PubMed] [Google Scholar]
- 27. Gautam S, Poudel A. Effect of gender on psychosocial adjustment of colorectal cancer survivors with ostomy. J Gastrointest Oncol. 2016;7:938‐945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hu A, Pan Y, Zhang M, et al. Factors influencing adjustment to a colostomy in Chinese patients: a cross‐sectional study. J Wound Ostomy Continence Nurs. 2014;41:455‐459. [DOI] [PubMed] [Google Scholar]
- 29. Jayarajah U, Samarasekera DN. Psychological adaptation to alteration of body image among stoma patients: a descriptive study. Indian J Psychol Med. 2017;39:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Karadağ A, Karabulut H, Baykara ZG, et al. A prospective, multicentered study to assess social adjustment in patients with an intestinal stoma in Turkey. Ostomy Wound Manage. 2015;61:16‐29. [PubMed] [Google Scholar]
- 31. Li CC, Rew L, Hwang S. The relationship between spiritual well‐being and psychosocial adjustment in Taiwanese patients with colorectal cancer and a colostomy. J Wound Ostomy Continence Nurs. 2012;39:161‐169. [DOI] [PubMed] [Google Scholar]
- 32. Simmons KL, Smith JA, Bobb KA, Liles LL. Adjustment to colostomy: stoma acceptance, stoma care self‐efficacy and interpersonal relationships. J Adv Nurs. 2007;60:627‐635. [DOI] [PubMed] [Google Scholar]
- 33. Mäkelä JT, Niskasaari M. Stoma care problems after stoma surgery in northern Finland. Scand J Surg. 2006;95:23‐27. [DOI] [PubMed] [Google Scholar]
- 34. Grove SK, Gray JR, Burns N. Understanding Nursing Research Building an Evidence‐Based Practice. St. Louis, MO: Elsevier Saunders; 2015. [Google Scholar]
- 35. Cheung YL, Molassiotis A, Chang AM. The effect of progressive muscle relaxation training on anxiety and quality of life after stoma surgery in colorectal cancer patients. Psychooncology. 2003;12:254‐266. [DOI] [PubMed] [Google Scholar]
- 36. Karabulut HK, Dinç L, Karadag A. Effects of planned group interactions on the social adaptation of individuals with an intestinal stoma: a quantitative study. J Clin Nurs. 2014;23:2800‐2813. [DOI] [PubMed] [Google Scholar]
- 37. Hoon LS, Chi Sally CW, Hong‐Gu H. Effect of psychosocial interventions on outcomes of patients with colorectal cancer: a review of the literature. Eur J Oncol Nurs. 2013;17:883‐891. [DOI] [PubMed] [Google Scholar]


