Dear Editors,
1.
Venous leg ulcers (VLUs) are a common disease with prevalence up to 2% in the population over 65 years of age.1 In many industrial countries, treatment costs of VLUs are approximately 1% of the healthcare budget.2 Many of these patients suffer from pain and non‐healing wounds for many years, sometimes for decades. Especially the correct and early diagnosis of VLU with an effective treatment is essential for a good chance of healing. Pathophysiological hypertension and hypervolemia are observed in the venous system of the lower extremities caused by reflux in the superficial, deep, or mainly superficial and deep veins.3 In addition to clinical examination, duplex sonography of the vein system of the leg up to the groin is the gold standard for assessing venous insufficiency.4 In our clinical routine, we had the impression that VLU are more common on the left lower leg in women. Therefore, we wanted to objectively analyse this question on the basis of our patient data.
Clinical data of 731 patients with the sonographic confirmed diagnosis VLU from the Department of Dermatology, University of Essen in Germany, were collected. In a database search, examinations of differences in the side distribution (right/left/both sides) were undertaken, with regard to gender (male/female). Data collection and analysis were performed with the IBM software SPSS 22. In the cohort, 284 patients were male (38.9%) and 447 patients were female (61.1%). Among the males, a total of 105 patients (37%) had the VLU on the right leg, 110 patients (38.7%) on the left leg, and 69 patients at both legs (24.3%). In women, 133 patients (29.8%) had the VLU on the right leg, 194 patients (43.4%) on the left leg, and 120 patients (26.8%) at both sides. A VLU was more frequent in 13.6% of women and 1.7% of men on the left leg (Figure 1). A one‐sided exact Fisher test showed that these differences were significant (χ 2=0.061; P = .037). Thus, VLU occurs significantly more frequently in women on the left leg.
Figure 1.
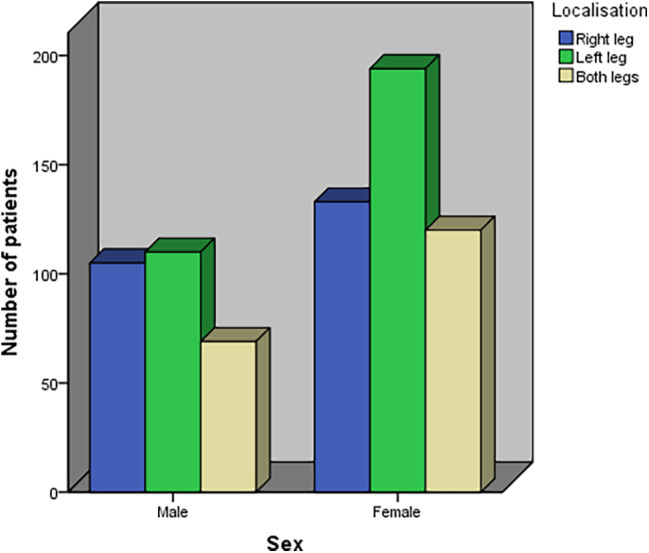
Comparison of localisations of venous leg ulcers in men and women [Color figure can be viewed at wileyonlinelibrary.com]
To the best of our knowledge, this is the first analysis to examine the differences in the distribution of the manifestation sides of the VLU between men and women. Now the question arises where these differences originate from. A possible explanation would be the pelvic congestion syndrome (PCS). PCS is a disorder of the pelvic vein circulation with dilatation of the veins that leads to pelvic pain that is impaired after coitus, during pregnancy, and during menstruation. Further clinical signs are vulvovaginal, gluteal, and lower limb varices. Underlying syndromes that lead to a PCS are May‐Thurner syndrome (MTS), Nutcracker syndrome, or the absence of the valves of the ovarian veins.5 MTS is an anatomical variant, where the right common iliac artery crosses the left common iliac vein. This anatomical variant leads to compression of the left common iliac vein and thus to an increase in venous blood pressure in the left lower extremity. It is well known that this can lead to chronic venous insufficiency or even VLU. In addition, deep vein thrombosis may occur in the left leg.6, 7 The Nutcracker syndrome is pathophysically characterised through compression of the left renal vein between aorta and superior mesenteric artery and leads to consecutive chronic venous insufficiency and VLU in the left leg. 8 Absence of ovarian vein valves occurs twice more often on the left side than on the right side.5
The biggest problem in clinical routine is diagnostics, as PCS cannot usually be detected with standard diagnostics such as duplex ultrasound of the leg veins.4 As an example, a retrospective radiologic study showed in 120 patients that a compression of the iliac vein is more often in patients with clinical diagnosis of chronic venous insufficiency than in the healthy population.9 Therapeutically, the insertion of endovascular stents, operations with thrombectomy, and reconstruction of the pelvic veins can be considered.
In our retrospective study, the number of patients with PCS was not objectified. This would be a very important aspect for a prospective study. Despite this limitation, based on our data, it is necessary for all clinically active therapists to consider the possibility of an underlying PCS in everyday clinical practice, especially in women with VLU of the left lower leg. This is particularly important if the duplex ultrasound of the leg veins, which usually ends in the groin, does not confirm pathological findings, but the patient has clinical signs of chronic venous insufficiency. For these patients, we consider further diagnostic steps, for example, with angiography to be useful in order to detect an already existing PCS. The endovascular treatment could then support the wound healing.10
In conclusion, our data support the hypothesis that PCS may be more frequently present undetected in females with VLU on the left lower leg. However, further prospective studies are needed to clearly prove this causal relationship.
2. ACKNOWLEDGMENTS
Open access funding enabled and organized by Projekt DEAL. [Correction added on 13 November 2020, after first online publication: Projekt Deal funding statement has been added.]
REFERENCES
- 1. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh vein study. J Epidemiol Community Health. 1999;53:149‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheng Q, Gibb M, Graves N, Finlayson K, Pacella RE. Cost‐effectiveness analysis of guideline‐based optimal care for venous leg ulcers in Australia. BMC Health Serv Res. 2018;18:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kanth AM, Khan SU, Gasparis A, Labropoulos N. The distribution and extent of reflux and obstruction in patients with active venous ulceration. Phlebology. 2015;30:350‐356. [DOI] [PubMed] [Google Scholar]
- 4. O'Donnell TF, Passman MA, Marston WA, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery® and the American venous forum. J Vasc Surg. 2014;60:3‐59. [DOI] [PubMed] [Google Scholar]
- 5. Borghi C, Dell'Atti L. Pelvic congestion syndrome: the current state of the literature. Arch Gynecol Obstet. 2016;293:291‐301. [DOI] [PubMed] [Google Scholar]
- 6. Alkhater M, Jockenhöfer F, Stoffels I, Dissemond J. May‐Thurner syndrome: an often overlooked cause for refractory venous leg ulcers. Int Wound J. 2017;14:578‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Butros SR, Liu R, Oliveira GR, Ganguli S, Kalva S. Venous compressions syndromes: clinical features, imaging findings and management. Br J Radiol. 2013;86:20130284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol. 2014;3:277‐281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liu P, Peng J, Zheng L, et al. Application of computed tomography venography in the diagnosis and severity assessment of iliac vein compression syndrome: a retrospective study. Medicine. 2018;97:12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pogorzelski R, Toutounchi S, Ostrowski T, Celejewski K, Gałązka Z. Long‐term results of endovascular treatment for may‐Thurner syndrome. Kardiol pol. 2017;75:815. [DOI] [PubMed] [Google Scholar]


