ABSTRACT
Background
Since 2003–4, the United States has seen large declines in sugar-sweetened beverage (SSB) intake overall, especially among non-Hispanic white (NHW) subpopulations. However, obesity prevalence has not shown comparable declines in the 2 highest SSB-consuming groups, adolescents and young adults. Little is understood about the quality of the diet excluding SSBs (non-SSB diet).
Objectives
The objective of this study was to evaluate differences in non-SSB diet quality in SSB consumers and nonconsumers in adolescents and young adults and in the 3 major race/ethnic subgroups.
Methods
This study utilized data from the NHANES, a cross-sectional, nationally representative survey of the US population. Data from 6426 participants aged 12–29 y from the NHANES (2009–2014) was included. Quality of the non-SSB diet was measured using the 2015 Healthy Eating Index (HEI). Multivariate linear regressions controlled for sociodemographic characteristics and included interactions by race/ethnicity [NHWs, non-Hispanic blacks (NHBs), Hispanics]. Individuals were classified as non-, low- (<10% of daily calories), or high-SSB consumers (≥10% of daily calories), according to the US Dietary Guidelines added sugar intake recommendation.
Results
Non-SSB HEI scores differed among SSB consumer groups (53 for adolescent nonconsumers compared with 46 for high consumers, P < 0.001; 57 for young adult nonconsumers compared with 45 for high consumers, P < 0.001), although all scores were low and require improvement. Among NHBs, significant differences in non-SSB HEI were found only between non- and low-SSB consumers. In Hispanics, associations varied by age group, with significant differences found for young adults but no association found for adolescents.
Conclusions
Low non-SSB HEI scores in SSB consumers suggest that reducing SSB consumption alone will not be a sufficient strategy for improving dietary quality in adolescents and young adults. Future policies must also consider improving the non-SSB diet.
Keywords: sugar sweetened beverages, diet quality, young adults, adolescents, healthy eating index, disparities
Introduction
Despite public health efforts to combat the obesity epidemic, obesity prevalence has not declined for adolescents and young adults (1, 2). From 1999–2000 to 2015–2016, the high prevalence of obesity in adolescents failed to decline (18% in 2007 to 21% in 2015) and significantly increased in young adults (31% to 36%) (1, 2). Increasingly, a method of tackling the obesity epidemic has been the reduction of sugar-sweetened beverages (SSBs) due to the association of SSBs with higher caloric intake (3–8). Although this increase in total caloric intake can be partly explained by the additional calories consumed in SSBs, this caloric increase alone does not fully explain the higher caloric intake of an SSB consumer's diet (6, 8–12). Therefore, increased caloric intake must also be attributable to some additional component of the diet. Poor dietary quality as measured by the Healthy Eating Index (HEI) has been associated with higher BMI and a higher probability of being overweight or obese (13–15). If the current trends for American diet quality continue, the Healthy People 2020 goals for food and nutrient consumption will not be met until after 2030 (16). In addition, high SSB consumption is associated with measures of poor dietary quality, irrespective of caloric intake; however, knowledge of the association between SSB consumption and the quality of the rest of the diet without SSBs (hereafter referred to as the non-SSB diet) is limited (17–21). Without understanding the healthfulness of the non-SSB diet, it is unclear if recent declines in SSB consumption (22–25) and the continued targeting of SSBs will be sufficient to improve the overall dietary quality of current SSB consumers.
Although declining SSB consumption has led to reductions in added sugar intake in adolescents and young adults, this age group continues to have the highest prevalence of heavy SSB consumers, as defined by the consumption of >500 kcal/d, which makes them an important group to target for dietary interventions (26). Adolescents and young adults are also exposed to obesogenic environments, including high school and university settings with easily accessible foods containing solid fats and added sugars (empty calories), and are the desirable targets of marketing for foods and beverages that are high in empty calories (26, 27). Both of these factors can contribute to poor quality of the non-SSB diet. Furthermore, it is important to understand variation within different race/ethnic groups. Compared with non-Hispanic whites (NHWs), non-Hispanic black (NHB) and Hispanic young adults and youth have a higher prevalence of obesity (1) and are more likely to consume SSBs (26, 28). Similarly, NHBs have lower HEI scores when compared with NHWs (29). Hispanics have been found to consume more fruits and vegetables than NHBs and NHWs (30). Given these examples of dietary differences between race/ethnic groups, it is necessary to assess the relation between SSB consumption and the non-SSB diet within these subpopulations.
The primary objective of this study was to evaluate differences in the non-SSB diet quality between low- and high-SSB consumers and nonconsumers in adolescents and young adults using 2009–2014 data from the NHANES. The secondary objective was the assessment of these associations within major race/ethnic subpopulations.
Methods
Study design and population
The study population was composed of 6426 adolescents (aged 12–18 y) and young adults (19–29 y) from the 2009–2010, 2011–2012, and 2013–2014 waves of the NHANES (Supplemental Figure 1). The latter is a nationally representative, cross-sectional study of the noninstitutionalized US population with a stratified, 4-stage probability sampling design (31). Certain subpopulations are oversampled including Hispanics, NHBs, and lower-income individuals. Data across all 3 waves of NHANES were combined to ensure a large enough sample size for analysis of race/ethnic subpopulations. The secondary dataset of deidentified data was deemed exempt from Institutional Review Board approval by the University of North Carolina at Chapel Hill Human Subjects Review Group.
Dietary data
Dietary data were obtained from the dietary intake component of NHANES, called What We Eat In America (32–34), where one to two 24-h recalls are administered in a subsample of the surveyed population. Data were collected using the multiple-pass method with day 1 from an in-person interview and day 2 from a telephone interview about 7–10 d later. When available, both days of dietary data were used. Of the 3281 adolescents with dietary data, 88% had 2 d of data. Of the 3145 young adults with dietary data, 85% had 2 d of data.
SSB exposure
SSB consumption was defined as the consumption of a liquid beverage with added sugar including water, presweetened coffee and tea, carbonated soft drinks, fruit drinks and nectars, sports drinks, energy drinks, and alcoholic beverages including beer, wine, liquor, and mixed beverages. Although encompassing alcoholic beverages, only those with added sugar were included in the SSB definition. These beverages were not included in the non-SSB HEI measurement. Any alcoholic beverages without added sugar would be grouped in the non-SSB HEI. Individuals were categorized as high- or low-SSB consumers based on their added sugar intake from SSBs as a percentage of total calories. The amount of added sugar contained in each beverage was obtained by linking the NHANES dietary data to the USDA's Food Patterns Equivalents Database (35). For each individual, added sugar was summed across all SSBs, converted to calories by multiplying grams of added sugar by 4 kcal, and dividing by the total calories consumed. For individuals with 2 d of dietary data, the added sugar calories from SSBs for both days were summed and divided by the sum of the total calories consumed over both days. This method is consistent with how component scores are calculated for the simple HEI algorithm used later to measure non-SSB dietary quality (36). To distinguish high and low consumers, the 2015–2020 US Dietary Guidelines recommendation was used as a guideline. It is suggested that adults and children reduce their added sugar intake to <10% of total daily calories (37). Therefore, high-SSB consumers included those who consumed ≥10% of their total daily calories as added sugar from SSBs. Low consumers included those who consumed 1% to <10% of their total daily calories as added sugar from SSBs. Non-SSB consumers included those who consumed <1% of their total daily calories as added sugar from SSBs. Because the US Dietary Guidelines pertain to added sugar in the entire diet rather than only in beverages, our thresholds will conservatively categorize individuals who are “high” SSB consumers.
Non-SSB diet quality
Dietary quality was measured using the 2015 HEI (36). HEI in this study was calculated without calories or added sugar from SSBs to analyze the quality of the rest of the diet, which will be referred to as the non-SSB HEI or non-SSB diet quality. The non-SSB HEI is calculated by summing 13 component scores, where a higher score indicates a healthier diet. NHANES provided data for calories, saturated fat, unsaturated fat, and grams of sodium whereas the USDA's Food Patterns Equivalent Database provided data for servings of fruits and vegetables in cup equivalents, servings of dairy in cup equivalents, servings of whole grains and protein foods in ounce equivalents, and grams of added sugar for the corresponding waves of NHANES data. The non-SSB HEI was calculated using the National Cancer Institute's (NCI's) simple HEI scoring algorithm calculated per person (36). When available, 2 d of dietary data were used by summing the amount and dividing by the total calories across 2 d before applying the HEI algorithm (36). Only 1 d of dietary data was used to calculate the non-SSB HEI for those individuals who did not respond to the telephone interview with a repeat 24-h dietary recall. For unadjusted analysis (Supplemental Table 1), dietary outcomes included total non-SSB HEI score and select non-SSB HEI component scores, including whole fruits, total vegetables, whole grains, saturated fat, and added sugar, whereas the dietary outcome for adjusted analysis was the total non-SSB HEI score. All 13 dietary components are included in the HEI analysis, but we do not present all in our tables to simplify the presentation.
Covariate data
Covariate data were obtained from the NHANES demographic questionnaires (38–40). The multivariate regression model included age, sex, race/ethnicity [NHWs (referent), NHBs, and Hispanics including Mexican Americans and other Hispanics], poverty income ratio (family income as a percentage of the federal poverty level), and parental education [less than high school, high school (referent), some college, and college]. Parental education was used for the analysis in adolescents (ages 12–18 y). Instead of using parental or individual education level for young adults (ages 19–29 y), no education covariate was used in the regression to avoid bias. For this age group, head of household education could refer to either the individual or a parent and lead to misclassification, whereas the respondent's education is highly correlated with age. Sensitivity analyses were conducted to evaluate for potential confounders, including height, day of the week of dietary recall (Mon–Thurs compared with Fri–Sun), and physical and sedentary activity. Physical activity and sedentary activity were both defined as dichotomous variables where the top 10% of total minutes of each activity were flagged as 1 and the other 90% were flagged as 0. We evaluated confounding using change-in-estimates criteria (41), where confounders would be added if they changed our associations by >10%. In each sensitivity analysis, the association between SSB consumer type and non-SSB HEI was not affected, so they were not included in the model.
Statistical analysis
All analyses were performed using NHANES sample weights to derive nationally representative estimates. Dietary day 1 weights were used because our sample includes all individuals aged 12–29 y with ≥1 d of dietary data (42). Because data were pooled across 3 waves from 2009 to 2014, the weights were recalculated by dividing by 3 (42). The sample was stratified to separately analyze adolescents (12–18 y) and young adults (19–29 y). Two-sample t tests were used to compare the differences between the weighted proportions of sociodemographic characteristics among SSB consumers and nonconsumers. Linear regression models examined the association between SSB consumer type and non-SSB dietary quality while controlling for the covariates mentioned previously. Low consumers were used as the referent given they had the largest sample size. To assess differences within race/ethnic groups, race/ethnicity was interacted with SSB consumption and tested using the Wald test. Statistical analyses were performed using Stata 15 (StataCorp). Estimates were calculated with Stata's survey command to adjust for NHANES complex survey design. Significant differences among dietary outcomes between SSB consumer types were identified using Stata margins and contrast postestimation commands. All hypothesis testing was 2-sided with a significance level of P < 0.05.
Results
Of the 3281 adolescents (ages 12–18 y) in the sample, 20.2% were nonconsumers, 47.9% were low-SSB consumers, and 32.0% were high-SSB consumers (Table 1). Young adults (ages 19–29) showed a similar pattern where, of the 3145 individuals, nonconsumers comprised 20.8% of the sample, low-SSB consumers comprised 42.8%, and high-SSB consumers comprised 36.5%. Nonconsumers for both age groups were more likely to be female, identify as NHW, and have a household income ≥185% of the federal poverty level, whereas high consumers of either age group were more likely to be male, identify as NHB, and have a household income <185% of the federal poverty level. Among adolescents, nonconsumers were more likely to have a head of household with ≥1 college degree.
TABLE 1.
Weighted description of US adolescents and young adults by sugar-sweetened beverage consumption level, NHANES 2009–20141
| Consumer type, % | |||||
|---|---|---|---|---|---|
| n | Nonconsumer | Low consumer | High consumer | ||
| Ages 12–18 y | n = 618 | n = 1650 | n = 1013 | ||
| Gender | |||||
| Male | 1681 | 17.9a, c | 49.5b | 32.5 | 100% |
| Female | 1600 | 22.4a, c | 46.2b | 31.4 | 100% |
| Race/ethnicity2 | |||||
| Hispanic | 1115 | 14.7a, c | 57.1b | 28.1 | 100% |
| Non-Hispanic white | 902 | 22.7a, c | 43.0b | 34.3 | 100% |
| Non-Hispanic black | 804 | 13.5a, c | 50.5b | 35.9 | 100% |
| Household income as % of poverty | |||||
| <185 | 1714 | 16.6a, c | 48.3b | 35.1 | 100% |
| ≥185 | 1567 | 22.8a, c | 47.6b | 29.7 | 100% |
| HH education | |||||
| Less than high school | 371 | 11.4a, c | 55.9b | 32.8 | 100% |
| High school | 1241 | 16.4a, c | 45.2 | 38.4 | 100% |
| Some college | 902 | 20.5a, c | 46.4b | 33.1 | 100% |
| College or higher | 666 | 26.7a | 49.5b | 23.8 | 100% |
| Ages 19–29 y | n = 581 | n = 1350 | n = 1214 | ||
| Gender | |||||
| Male | 1553 | 18.8a, c | 43.8b | 37.5 | 100% |
| Female | 1592 | 22.9a, c | 41.7b | 35.5 | 100% |
| Race/ethnicity | |||||
| Hispanic | 848 | 13.0a, c | 45.1 | 41.8 | 100% |
| Non-Hispanic white | 1129 | 24.6a, c | 41.8b | 33.7 | 100% |
| Non-Hispanic black | 729 | 42.1a, c | 42.1 | 44.8 | 100% |
| Household income as % of poverty | |||||
| <185 | 1729 | 17.6a | 42.4 | 40.0 | 100% |
| ≥185 | 1416 | 23.6a, c | 43.0b | 33.3 | 100% |
Data collected from NHANES 2009–2014 and corrected for complex survey design using day 1 dietary sample weights. HH, head of household.
Excluded from the demographics were other race/ethnicities such as Asians, American Indians, etc. due to low sample size.
Proportions are different when compared between nonconsumers and low consumers at P < 0.05.
Proportions are different when compared between low consumers and high consumers at P < 0.05.
Proportions are different when compared between nonconsumers and high consumers at P < 0.05.
Descriptive statistics of components of the non-SSB diet are summarized in Supplemental Table 1. Estimates are survey-weighted but unadjusted. For both adolescents and young adults, high- and low-SSB consumers had greater caloric intake from the non-SSB diet when compared with nonconsumers (Supplemental Table 1). However, low-SSB consumers were found to have a greater total energy intake even compared with high-SSB consumers. In addition, non-SSB HEI decreased as SSB consumption increased for both adolescents and young adults. The component that most improved non-SSB HEI scores was the score for added sugar, indicating that added sugar consumption in the non-SSB diet falls within the 2015 US Dietary Guidelines. As SSB consumption decreased, the component scores for added sugar, saturated fat, whole fruit, total vegetables, and whole grains in the non-SSB diet improved for both males and females.
Results for adjusted, multivariate models of the association between non-SSB HEI scores and SSB consumption can be found in Figure 1 and Supplemental Table 2. Both adolescents and young adults were found to have significantly different non-SSB HEI scores among different SSB consumer groups. When compared with low consumers as the referent group, adolescent nonconsumers had a predicted non-SSB HEI score that was 4 points higher (P < 0.001), whereas the predicted non-SSB HEI for high consumers was 3 points lower (P < 0.001). The predicted non-SSB HEI for young adult nonconsumers was 6 points higher (P < 0.001) than low consumers, and that for high consumers was 6 points lower (P < 0.001).
FIGURE 1.
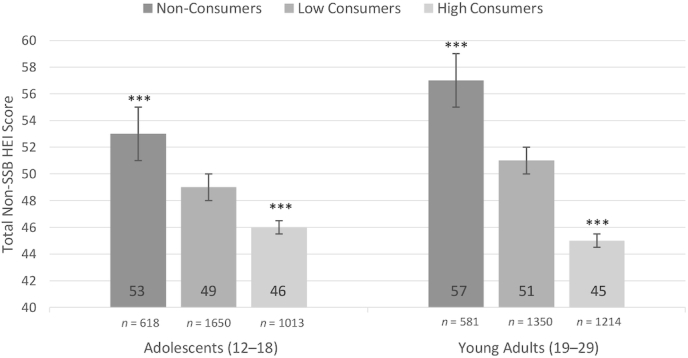
Non-SSB diet quality of SSB consumers by age group ± SE. The study population was composed of 6426 adolescents (aged 12–18 y) and young adults (aged 19–29 y) from NHANES 2009–2014. Results are adjusted for relevant sociodemographic covariates, including age, sex, race/ethnicity, and poverty income level. Adolescent results were also adjusted for parental education level. SSB consumption was categorized as nonconsumers, low consumers, and high consumers where nonconsumers consume <1% of their total daily calories as added sugar from SSBs, low consumers consume 1% to <10% of their total daily calories as added sugar from SSBs, and high consumers consume ≥10% of their total daily calories as added sugar from SSBs. Non-SSB diet quality was measured using the 2015 Health Eating Index, which was calculated without calories or added sugar from SSBs to analyze the quality of the rest of the diet without SSBs. ***Significant compared with low-SSB consumers (referent), P < 0.001. HEI, Healthy Eating Index; SSB, sugar-sweetened beverage.
Further analysis included interactions between race/ethnic groups to assess potential disparities in non-SSB HEI scores among adolescents (Figure 2, Supplemental Table 3) and young adults (Figure 3, Supplemental Table 3). Similar patterns of non-SSB HEI scores in relation to SSB consumption were found for NHWs when compared with the overall study population, although they varied among NHBs and Hispanics. NHW adolescents and young adults both have significantly different non-SSB HEI scores for nonconsumers and high-SSB consumers when compared with low-SSB consumers (P < 0.001). Notably, NHW young adult high consumers had the lowest predicted non-SSB HEI when compared with all other groups, with a score of 44. In NHB young adults, nonconsumers’ predicted non-SSB HEI score was significantly higher than that of low consumers by 7 points (P < 0.001). Hispanics’ and NHB adolescents’ predicted non-SSB HEI scores were not associated with SSB consumption. However, in Hispanic young adults, nonconsumers had a predicted score 5 points higher (P < 0.05) than that of low consumers, and the score for high consumers was 6 points lower (P < 0.001) than for low consumers. The highest predicted score was 59 points for Hispanic young adult nonconsumers.
FIGURE 2.
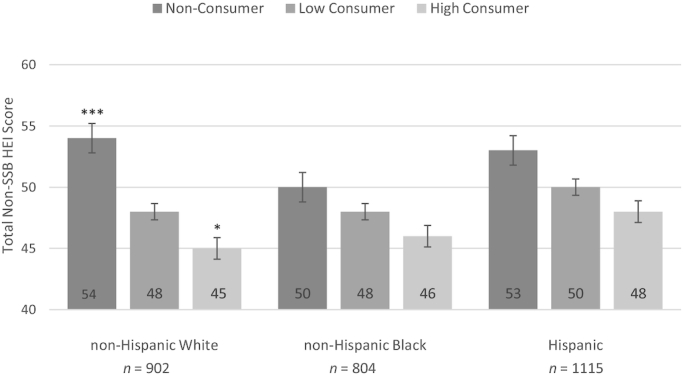
Non-SSB diet quality of adolescent SSB consumers by race/ethnic group ± SE. Model was fitted using interaction terms between SSB consumers and race/ethnicity. The study population was composed of 6426 adolescents (12–18 y) and young adults (19–29 y) from NHANES 2009–2014. Results are adjusted for relevant sociodemographic covariates, including age, sex, race/ethnicity, and poverty income level. Adolescent results were also adjusted for parental education level. SSB consumption was categorized as nonconsumers, low consumers, and high consumers where nonconsumers consume <1% of their total daily calories as added sugar from SSBs, low consumers consume 1% to <10% of their total daily calories as added sugar from SSBs, and high consumers consume ≥10% of their total daily calories as added sugar from SSBs. Non-SSB diet quality was measured using the 2015 Healthy Eating Index, which was calculated without calories or added sugar from SSBs to analyze the quality of the rest of the diet without SSBs. *,***Significant compared with low-SSB consumers (referent) within same race/ethnic group; *P < 0.05, ***P < 0.001. HEI, Healthy Eating Index; SSB, sugar-sweetened beverage.
FIGURE 3.
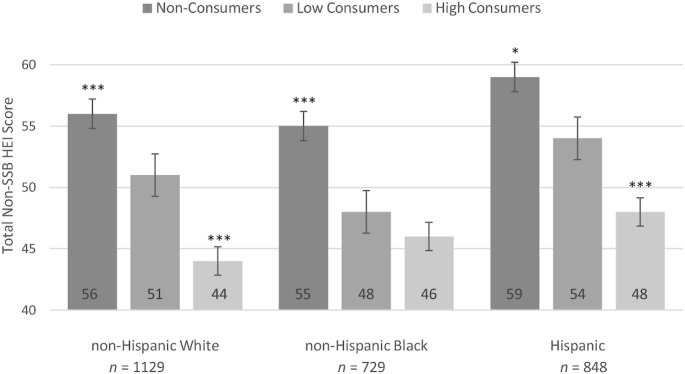
Non-SSB diet quality of young adult SSB consumers by race/ethnic group ± SE.Model was fitted using interaction terms between SSB consumers and race/ethnicity. The study population was composed of 6426 adolescents (12–18 y) and young adults (19–29 y) from NHANES 2009–2014. Results are adjusted for relevant sociodemographic covariates, including age, sex, race/ethnicity, and poverty income level. Adolescent results were also adjusted for parental education level. SSB consumption was categorized as nonconsumers, low consumers, and high consumers where low consumers were defined as those who consumed between 1% and <10% of their total daily calories in added sugar from SSBs. Non-SSB diet quality was measured using the 2015 Healthy Eating Index, which was calculated without calories or added sugar from SSBs to analyze the quality of the rest of the diet without SSBs. *,***Significant compared with low-SSB consumers (referent) within same race/ethnic group; *P < 0.05, ***P < 0.001. HEI, Healthy Eating Index; SSB, sugar-sweetened beverage.
Discussion
This study examined the association between SSB consumption and the quality of the non-SSB diet in adolescents and young adults using the 2015 HEI and the most current dietary data from NHANES. In general, for both adolescents and young adults, as SSB consumption increased there were significantly lower total non-SSB HEI scores. Notably, although there was an improvement in non-SSB HEI scores with lower SSB consumption, scores ranged no higher than 59, which indicates a diet that “needs improvement,” whereas a score of ≤51 represents a “poor” diet (43). However, when non-SSB HEI scores were compared by race/ethnicity, patterns emerged for each group that have distinct implications for potential nutrition interventions.
Among NHWs, non-SSB diet quality was significantly worse as SSB consumption increased. Additionally, both adolescent and young adult NHW high consumers had the poorest dietary quality across all race/ethnic groups, making NHWs the highest-risk group (26). This strong association suggests that interventions targeting SSB consumption can only lead to improvement of diet quality if a reduction in SSB intake causes the non-SSB diet of high consumers to converge with that of nonconsumers. If low non-SSB HEI scores are due to foods typically paired with SSBs such as pizza, burgers, and fried potatoes, as found in one study (44), then simply reducing SSB consumption might improve non-SSB dietary quality. However, it is important to note that although reducing SSB consumption would be of some value, it would not be sufficient to reach a good-quality diet given that even NHW nonconsumers have poor non-SSB HEI scores.
In comparison, there was not a strong association between SSB consumption and non-SSB diet quality in NHBs. In adolescents, there was no significant difference between nonconsumers’ and low consumers’ non-SSB HEI scores, nor between those of low consumers and high consumers. This suggests that NHB adolescents have poor overall diet quality regardless of their SSB consumption. Given the lack of any association, reducing SSB consumption and changing any dietary behaviors related to this consumption might not improve dietary quality. Therefore, interventions targeting SSB consumption should also equally emphasize improving diet quality for this group in particular, such as increasing fruit, vegetable, and whole grain consumption. Furthermore, the decreased accessibility of healthy food options in many minority neighborhoods must be considered (45, 46). If there are few to no healthy options, then minority groups will have unhealthier diets no matter which SSB consumer category they fall into.
Among Hispanics, results differed between adolescents and young adults. For Hispanic adolescents, there was no association between SSB consumption and dietary quality, whereas there was a significant association in young adults. Notably, Hispanic young adults who are high SSB consumers had a higher non-SSB HEI score than both NHW and NHB young adult high-SSB consumers. Previous research has found that Hispanics have higher fruit and vegetable consumption, which leads to higher total HEI scores. Although Hispanics consume more SSBs compared with NHWs (27, 28, 30), the quality of the rest of the diet is independent of that. In addition, Hispanic young adults were found to have some of the highest total non-SSB HEI scores when compared with NHW and NHB adolescents and young adults. This will be important for future interventions targeting Hispanic young adults’ SSB consumption. If SSBs are removed from the diet and the rest of the diet tends to be of better quality than the rest of the population, then this group could benefit solely from SSB-focused interventions. Furthermore, the dietary patterns of young adult nonconsumers could be used to inform culturally relevant dietary interventions in adolescents.
The results of this study have implications for obesity and chronic disease prevention in all adolescents and young adults. Reducing SSB consumption has been suggested as an effective strategy to decrease total caloric intake and/or improve the quality of the diet (47), yet these results suggest this cannot be a stand-alone strategy. Low- and high-SSB consumers had higher caloric intake compared with the non-SSB consumers, so even if SSB consumption declines, reduction of calories from the remaining parts of the diet is still important for obesity prevention. In addition, although SSB consumption in adolescents and young adults has been declining (25), our study found consistently low non-SSB HEI scores across all age and race/ethnic groups. Poor non-SSB HEI scores are driven by low HEI component scores for total vegetable, total fruit, and whole grain consumption (Supplemental Table 1) indicating that these are aspects of the diet that could also benefit from targeted interventions. A study of the general US population found that the only 2010 HEI components expected to reach the Healthy People 2020 goals are empty calories and whole fruit (16). Therefore, future interventions aimed at reducing obesity and chronic disease should promote total vegetable and whole grain and legume consumption along with reduced SSB consumption.
The negative association between SSB consumption and non-SSB dietary quality is consistent with previous research. Only 1 other study has examined the quality of the non-SSB diet, finding increased SSB consumption to be associated with lower 2010 HEI scores in both overall diet quality and the non-SSB diet for adolescents in the United States (48). The present study adds to this body of literature by excluding SSBs from the diet quality calculations in a broader age group and using the most recent NHANES dietary data with the 2015 HEI. In addition, no other study, to the best of our knowledge, has examined variation in the association between SSB consumption and non-SSB dietary quality by race/ethnic group.
There are several limitations to this study. The data from a 24-h recall are prone to recall bias and self-reported dietary data are often misreported, where energy intake and foods that are considered to be “less healthy” are underreported (49, 50). This can lead to lower reporting of added sugar and SSB consumption, which can underestimate the number of SSB consumers or overestimate non-SSB HEI scores. Additionally, only 2 d of dietary recall were used for this study, which might incorrectly classify nonconsumers or be sensitive to outliers if individuals consume foods outside their normal dietary patterns on interview days. However, the NCI method of combining 2 d of dietary data was used to limit measurement error when calculating SSB consumption and non-SSB HEI scores. In addition, we categorized low- and high-SSB consumers based on recommendations that added sugar intake be limited to 10% of total intake. However, this recommendation is for the entire diet. SSBs make up a portion of the potential sources of added sugar, but there is no widely accepted definition of “high” SSB consumption. Our threshold conservatively classifies individuals as high consumers and might misclassify “high” consumers into the “low” consumer category. Another limitation is that this cross-sectional analysis cannot demonstrate a causal relation between SSB consumption and diet quality. Lastly, only 3 race/ethnic groups were used due to small samples sizes for the highly heterogeneous “other” races category. Further research is needed to inform targeted public health interventions in other race/ethnic groups.
Despite these limitations, there are several strengths to this study. Recall data allowed all foods consumed by an individual to be captured in the analysis. Additionally, the use of the multipass methods helped to ensure the validity of the 24-h recall data. NHANES is a nationally representative survey that allows conclusions to be drawn about the US population of adolescents and young adults. NHBs and Hispanics are oversampled in NHANES to increase sample size. This provided enough data to evaluate the association between SSB consumption and diet quality in age and race/ethnic subpopulations, which adds to the current literature on these associations and helps inform more targeted public health interventions.
In conclusion, this study found that the quality of the non-SSB diet was lower with higher SSB consumption, suggesting that those who consume more SSBs also consume foods of poorer quality compared with those who do not consume SSBs. Furthermore, this association was found to differ among race/ethnic groups. Future research is needed to determine whether this difference is attributable to the general food preferences of SSB consumers or to foods that are typically only consumed when paired with SSBs. If high-SSB consumers prefer unhealthy foods, then they might substitute SSBs with other foods of poor quality. Nevertheless, the results of this analysis suggest that a focus on SSBs alone might not be a sufficient strategy without additional dietary interventions because all age and race/ethnic groups have low non-SSB HEI scores, indicating a diet that requires improvement. In addition to policies that target SSBs, dietary interventions are needed to improve the quality of the diet to affect the prevalence of obesity and chronic diseases.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Dr Phil Bardsley and Ms Karen Ritter for great data management and programming support. We also thank Ms Denise Ammons for graphics support.
The authors’ responsibilities were as follows—AMD, AML, and BMP: designed research; AMD: conducted statistical analysis; AMD, AML, and BMP: wrote the paper; BMP: had primary responsibility for final content; and all authors: read and approved the final manuscript.
The authors report no conflicts of interest.
Notes
Funding is from the Arnold Ventures and the NIH CPC P2C HD050924 and T32 HD007168. Funders had no direct role in the study design, analysis, or manuscript preparation.
Supplemental Tables 1–3 and Supplemental Figure 1 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: HEI, Healthy Eating Index; NCI, National Cancer Institute; NHB, non-Hispanic black; NHW, non-Hispanic white; SSB, sugar-sweetened beverage.
Contributor Information
Alex M Doherty, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Allison M Lacko, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Barry M Popkin, Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Data Availability
Data described in the manuscript, code book, and analytic code will be made publicly and freely available without restriction at https://github.com/AMLacko/SSB-diet-YA.
References
- 1. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS data brief no. 288. US Department of Health and Human Services; 2017. [PubMed] [Google Scholar]
- 2. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. DellaValle DM, Roe LS, Rolls BJ. Does the consumption of caloric and non-caloric beverages with a meal affect energy intake?. Appetite. 2005;44(2):187–93. [DOI] [PubMed] [Google Scholar]
- 4. Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav. 1996;59(1):179–87. [DOI] [PubMed] [Google Scholar]
- 5. Mattes RD. Beverages and positive energy balance: the menace is the medium. Int J Obes. 2006;30:S60–5. [Google Scholar]
- 6. Mourao DM, Bressan J, Campbell WW, Mattes RD. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes. 2007;31(11):1688–95. [DOI] [PubMed] [Google Scholar]
- 7. Reid M, Hammersley R, Hill AJ, Skidmore P. Long-term dietary compensation for added sugar: effects of supplementary sucrose drinks over a 4-week period. Br J Nutr 2007;97(1):193–203. [DOI] [PubMed] [Google Scholar]
- 8. DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes. 2000;24(6):794–800. [DOI] [PubMed] [Google Scholar]
- 9. Bleich SN, Wolfson JA. U.S. adults and child snacking patterns among sugar-sweetened beverage drinkers and non-drinkers. Prev Med. 2015;72:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Piernas C, Mendez MA, Ng SW, Gordon-Larsen P, Popkin BM. Low-calorie- and calorie-sweetened beverages: diet quality, food intake, and purchase patterns of US household consumers. Am J Clin Nutr. 2014;99(3):567–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Piernas C, Ng SW, Mendez MA, Gordon-Larsen P, Popkin BM. A dynamic panel model of the associations of sweetened beverage purchases with dietary quality and food-purchasing patterns. Am J Epidemiol. 2015;181(9):661–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ruff RR, Akhund A, Adjoian T, Kansagra SM. Calorie intake, sugar-sweetened beverage consumption, and obesity among New York City adults: findings from a 2013 population study using dietary recalls. J Community Health. 2014;39(6):1117–23. [DOI] [PubMed] [Google Scholar]
- 13. Sundararajan K, Campbell MK, Choi Y-H, Sarma S. The relationship between diet quality and adult obesity: evidence from Canada. J Am Coll Nutr. 2014;33(1):1–17. [DOI] [PubMed] [Google Scholar]
- 14. Nicklas TA, Baranowski T, Cullen KW, Berenson G. Eating patterns, dietary quality and obesity. J Am Coll Nutr. 2001;20(6):599–608. [DOI] [PubMed] [Google Scholar]
- 15. An R. Diet quality and physical activity in relation to childhood obesity. Int J Adolesc Med Health. [Internet]2017;29(2):20150045. 10.1515/ijamh-2015-0045. [DOI] [PubMed] [Google Scholar]
- 16. Wilson MM, Reedy J, Krebs-Smith SM. American diet quality: where it is, where it is heading, and what it could be. J Acad Nutr Diet. 2016;116(2):302–10.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O'Neil CE, Nicklas TA, Liu Y, Franklin FA. Impact of dairy and sweetened beverage consumption on diet and weight of a multiethnic population of head start mothers. J Am Diet Assoc. 2009;109(5):874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Frary CD, Johnson RK, Wang MQ. Children and adolescents' choices of foods and beverages high in added sugars are associated with intakes of key nutrients and food groups. J Adolesc Health. 2004;34(1):56–63. [DOI] [PubMed] [Google Scholar]
- 19. Mullie P, Deliens T, Clarys P. Relation between sugar-sweetened beverage consumption, nutrition, and lifestyle in a military population. Mil Med. 2016;181(10):1335–9. [DOI] [PubMed] [Google Scholar]
- 20. Sharkey JR, Johnson CM, Dean WR. Less-healthy eating behaviors have a greater association with a high level of sugar-sweetened beverage consumption among rural adults than among urban adults. Food Nutr Res. [Internet]2011;55. 10.3402/fnr.v55i0.5819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rodriguez-Artalejo F, Garcia EL, Gorgojo L, Garces C, Royo MA, Martin Moreno JM, Benavente M, Macias A, De Oya M. Consumption of bakery products, sweetened soft drinks and yogurt among children aged 6–7 years: association with nutrient intake and overall diet quality. Br J Nutr. 2003;89(3):419–29. [DOI] [PubMed] [Google Scholar]
- 22. Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr. 2014;99(3):609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Powell ES, Smith-Taillie LP, Popkin BM. Added sugars intake across the distribution of US children and adult consumers: 1977–2012. J Acad Nutr Diet. 2016;116(10):1543–50.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slining MM, Popkin BM. Trends in intakes and sources of solid fats and added sugars among U.S. children and adolescents: 1994–2010. Pediatr Obes. 2013;8(4):307–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr. 2011;94(3):726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet. 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poti JM, Slining MM, Popkin BM. Where are kids getting their empty calories? Stores, schools, and fast-food restaurants each played an important role in empty calorie intake among US children during 2009–2010. J Acad Nutr Diet. 2014;114(6):908–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Poti JM, Mendez MA, Ng SW, Popkin BM. Highly processed and ready-to-eat packaged food and beverage purchases differ by race/ethnicity among US households. J Nutr. 2016;146(9):1722–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Raffensperger S, Kuczmarski MF, Hotchkiss L, Cotugna N, Evans MK, Zonderman AB. Effect of race and predictors of socioeconomic status on diet quality in the HANDLS study sample. J Natl Med Assoc. 2010;102(10):923–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306. [DOI] [PubMed] [Google Scholar]
- 31. Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. Vital and Health Statistics Series 2, No. 162. National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey data. [Internet]. Hyattsville (MD): US Department of Health and Human Services, CDC; 2009–2010; [cited January 8, 2019]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2009-2010/DR1IFF_F.htm [Google Scholar]
- 33. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey data. [Internet]. Hyattsville (MD): US Department of Health and Human Services, CDC; 2011; [cited January 8, 2019]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/DR1IFF_G.htm [Google Scholar]
- 34. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey data. [Internet]. Hyattsville (MD): US Department of Health and Human Services, CDC; 2013–2014; [cited January 8, 2019]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DR1IFF_H.htm [Google Scholar]
- 35. US Department of Agriculture, Agriculture Research Service . Overview of food patterns equivalents database [Internet]. [cited December2018]. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/ [Google Scholar]
- 36. National Cancer Institute . The Healthy Eating Index scoring algorithm method. [Internet]. Updated February 12, 2018; [cited December 2018]. Available from: https://epi.grants.cancer.gov/hei/hei-scoring-method.html [Google Scholar]
- 37. US Department of Health and Human Services, US Department of Agriculture . 2015–2020 dietary guidelines for Americans, 8th ed.[Internet]. December2015; [cited January 8, 2019]. Available from: http://health.gov/dietaryguidelines/2015/guidelines/ [Google Scholar]
- 38. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey 2009–2010 (demographics file). Hyattsville (MD): US Department of Health and Human Services, CDC [cited; December 2018] [Internet]. Available from:; https://wwwn.cdc.gov/Nchs/Nhanes/2009-2010/DEMO_F.htm [Google Scholar]
- 39. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey 2011–2012 (demographics file). Hyattsville (MD): US Department of Health and Human Services, CDC [cited December 2018] [Internet]. Available from:https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/DEMO_G.htm [Google Scholar]
- 40. Centers for Disease Control and Prevention (CDC) , National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey 2013–2014 (demographics file). Hyattsville (MD): US Department of Health and Human Services, CDC [cited December 2018] [Internet]. Available from:https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DEMO_H.htm [Google Scholar]
- 41. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital and Health Statistics Series 2, No. 161. National Center for Health Statistics, 2013.: [PubMed] [Google Scholar]
- 43. Hurley KM, Oberlander SE, Merry BC, Wrobleski MM, Klassen AC, Black MM. The healthy eating index and youth healthy eating index are unique, nonredundant measures of diet quality among low-income, African American adolescents. J Nutr. 2009;139(2):359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mathias KC, Slining MM, Popkin BM. Foods and beverages associated with higher intake of sugar-sweetened beverages. Am J Prev Med. 2013;44(4):351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gustafson A, Hankins S, Jilcott S. Measures of the consumer food store environment: a systematic review of the evidence 2000–2011. J Community Health. 2012;37(4):897–911.. doi:10.1007/s10900-011-9524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bader MDM, Purciel M, Yousefzadeh P, Neckerman KM. Disparities in neighborhood food environments: implications of measurement strategies. Econ Geogr. 2010;86(4):409–30. [DOI] [PubMed] [Google Scholar]
- 47. Wang YC, Orleans CT, Gortmaker SL. Reaching the healthy people goals for reducing childhood obesity: closing the energy gap. Am J Prev Med. 2012;42(5):437–44. [DOI] [PubMed] [Google Scholar]
- 48. Leung CW, DiMatteo SG, Gosliner WA, Ritchie LD. Sugar-sweetened beverage and water intake in relation to diet quality in US children. Am J Prev Med. 2018;54(3):394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rasmussen LB, Matthiessen J, Biltoft-Jensen A, Tetens I. Characteristics of misreporters of dietary intake and physical activity. Public Health Nutr. 2007;10(3):230–7. [DOI] [PubMed] [Google Scholar]
- 50. Lafay L, Mennen L, Basdevant A, Charles MA, Borys JM, Eschwege E, Romon M. Does energy intake underreporting involve all kinds of food or only specific food items? Results from the Fleurbaix Laventie Ville Sante (FLVS) study. Int J Obes Relat Metab Disord. 2000;24(11):1500–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book, and analytic code will be made publicly and freely available without restriction at https://github.com/AMLacko/SSB-diet-YA.


