Abstract
To assess the efficacy of topical silicone gel in the management of scars, we conducted this meta‐analysis. The systematic search was performed on PubMed, Web of Science and Embase, and six randomised controlled trials with a total of 375 patients were involved. The outcome data of Vancouver Scar Scale were extracted from the studies and their effect sizes were calculated using Review Manager 5.3. As a result, topical silicone gel significantly reduced pigmentation, height, and pliability scores postoperatively compared with placebos or no treatment (Pigmentation: standard mean difference [SMD] = −0.55 [−0.83 to –0.26], P = .0002; Height: SMD = −0.73 [−1.02 to –0.44], P < .00001; Pliability: SMD = −0.49 [−0.95 to –0.03], P = .04). Topical silicone gel and silicone gel sheet were comparably effective (P > .05). The performance of topical silicone gel and other non‐silicone topical treatment was also similar (P > .05). In summary, topical silicone gel was effective in post‐operative scar prevention.
Keywords: prevention, scar, silicone gel, topical therapy, treatment
1. INTRODUCTION
Pathological scars including hypertrophic scars and keloids are very common diseases. Hypertrophic scars occurred in 16% patients with burns and the prevalence of keloids in Black Africans was reported to be around 3.5%.1, 2 Hypertrophic scars can develop from skin injuries caused by trauma, surgery, and burns, while keloids arise from skin wounds caused by trauma, shaving, surgery, and vaccination.2, 3
Silicone gel has been used in scar management since the 1980 seconds.4 Silicone‐based products were deemed as the first‐line, gold standard therapy for scar management and have shown efficacy in both prevention and treatment of pathological scars.5 According to the Cochrane meta‐analysis by O'Brien and Jones, silicone gel sheet as a way of pathological scar prevention was effective in high‐risk patients and improvement in scar thickness and scar colour was also reported in patients using silicone gel sheet for pathological scar treatment.6
Topical silicone gel, another silicone‐based product for scar management, is also widely used in clinical practice. However, in a meta‐analysis by Hsu et al, topical silicone gel did not outperform placebos in pathological scar prevention, while silicone gel sheet once again showed efficacy.7 We conducted a systematic review and meta‐analysis to see whether application of silicone gel in scars was effective. In addition, we wanted to explore whether the form of dressings really mattered to treatment efficacy.
2. METHODS
2.1. Search strategy
Following the searching strategies described by O'Brien and Jones,6 we conducted a comprehensive electronic search of Embase, Web of Science, and Pubmed from the time of database establishment to November 2019. The reference lists of publications in this field were also manually searched for additional studies.
2.2. Study selection
Inclusion criteria: (a) Randomised controlled trials (RCTs), (b) patients were given topical silicone gel or other therapies for scar prevention or treatment, and (c) Vancouver Scar Scale (VSS) or patient and Observer Scar Assessment Scale (POSAS) were used for scar evaluation. Studies were excluded if they were abstracts only or duplications, performed inaccurate statistical analysis or applied combined treatment rather than single treatment.
2.3. Data retrieval
The following information was extracted:(a) The publication years and authors of involved studies, (b) countries of the main authors, (c) scar types, (d) sample sizes, (e) interventions and controls, (f) treatment duration and follow‐up periods, and (g) outcome measurement.
2.4. Qualitative assessment
The quality of each included study was reviewed using the Cochrane risk of bias assessment tool. According to the assessment tool, the quality of each article was evaluated based on the following six items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. The classifications of low risk, high risk, and unclear risk were given to each study based on authors' judgements. Divergences were resolved through a discussion.
2.5. Statistical analysis
A meta‐analysis to investigate the efficacy of topical silicone gel in scar management was conducted using Review Manager software (version 5.3, provided by the Cochrane collaboration). For continuous outcomes, we estimated the standard mean difference with 95% confidence intervals. The chi‐square test and I 2 statistic were applied to evaluate the heterogeneity across studies. P value for chi‐square test >0.1or I 2 > 50% indicated significant heterogeneity. For studies with insignificant heterogeneity, a fixed‐effect model (Mantel‐Haenszel method) was used for analysis. Otherwise, a random‐effect model was used. A P‐value <.05 was considered statistically significant.
3. RESULTS
3.1. Search process
Altogether, 487 studies and 1 additional study from the references of pertinent publications in this field were identified after an exhaustive search. After removal of duplicates and screening based on their titles and abstracts, 23 studies remained for full‐text assessment. In the 23 studies, four RCTs used POSAS for scar evaluation.8, 9, 10, 11 Since, scores from different scar scales could not be pooled together and a lack of attainable data to process quantitative analysis from studies using POSAS, our meta‐analysis only focused on studies using VSS. In addition, five RCTs using VSS did not report results in the form of mean ± standard deviation and were excluded.12, 13, 14, 15, 16 Finally, six RCTs with a total of 375 patients were included17, 18, 19, 20, 21, 22 (Figure 1). The baseline characteristics of the six studies were shown in Table 1.
Figure 1.
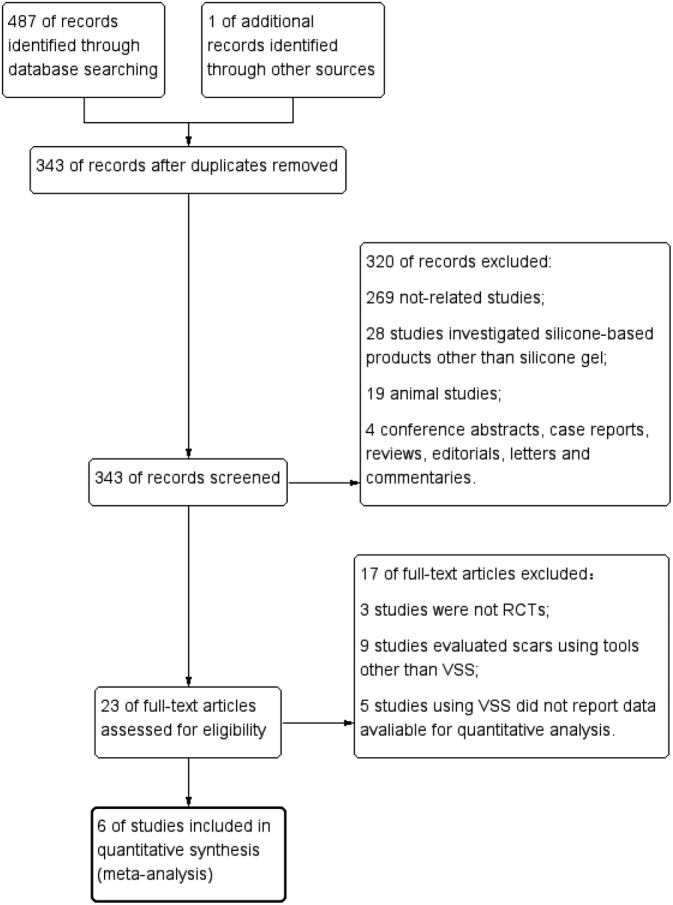
Study flow diagram
Table 1.
Study characteristics of all randomised trials included in the meta‐analysis
| Studies | Country of main authors | Sample size | Scar cause | Intervention | Control | Treatment group size: control group size | Treatment duration | Follow up length |
|---|---|---|---|---|---|---|---|---|
| Karagoz 200922 | Turkey | 45 | Untreated postburn hypertrophic scars within 6 mo | SG | SGS/ onion Extract | 15:15 (SGS):15 (onion extract) | 6 mo | 6 mo |
| Kong 201419 | Korea | 96 |
Tricompartmental cemented total knee arthroplasty |
SG | Petrolatum | 48:48 | 1 mo | 12 mo |
| Meseci 201718 | Turkey | 60 | Surgery for benign gynaecological diseases through a primary Pfannenstiel incision | SG | No treatment/ methylprednisolone cream | 21:18 (no treatment):21 (methylprednisolone cream) | 3 mo | 6 mo |
| Lin 201820 | China | 20 | horizontal Caesarean section using Pfannenstiel incision | SG | SGS | 20:20 (each surgical wound divided into 2 halves) | 3 mo | 12 mo |
| Song 201817 | Korea | 90 | Gynaecologic laparoscopic surgery | SG |
No treatment/ onion extract |
30:30 (no treatment): 30 (onion extract) | 12 wK | 12 wK |
| Shirazi 201921 | Iran | 64 | Hypospadias surgical repair | SG | Vaseline | 32:32 | 2 mo | 8 mo |
Abbreviations: SG, silicone gel; SGS, silicone gel sheet.
3.2. Characteristics of included studies
Among all these 375 patients, 166 patients received topical silicone gel, 35 patients received silicone gel sheet, 66 patients received non‐silicone treatment, and 128 patients receive placebos or no treatment (Each surgical wound of 20 patients was divided into two halves and each half received treatment randomly in the study by Lin et al).20 Besides silicone gel in the treatment group, the control group included silicone gel sheet, onion extract, methylprednisolone cream, vaseline (petrolatum), and no treatment at all. The treatment duration ranged from 1 to 6 months and the follow‐up period ranged from 12 weeks to 12 months. Except for one study, which included patients with untreated post‐burn hypertrophic scar, the remaining five studies all included patients with post‐operative wounds for prevention.
3.3. Qualitative assessment results
The details of the qualitative assessment are shown in Figure 2. Studies by Lin et al and Song et al illustrated randomization procedures in detail.17, 20 Only the study by Song et al reported allocation concealment.17 The study by Shirazi et al mentioned its nature of a double‐blind RCT, while the studies by Song et al, Kong et al, and Meseci et al only mentioned their outcome assessment blindness methods.17, 18, 19, 21 The study by Lin et al declared the lacking of blindness in their study and the study by Karagoz et al did not report any blindness at all.20, 22 Half of the studies got high attrition bias risk due to partial loss of data in their final outcomes.18, 19, 20 Clinical trials registration was mentioned in all studies except for two, which did not provide registration numbers.18, 22
Figure 2.
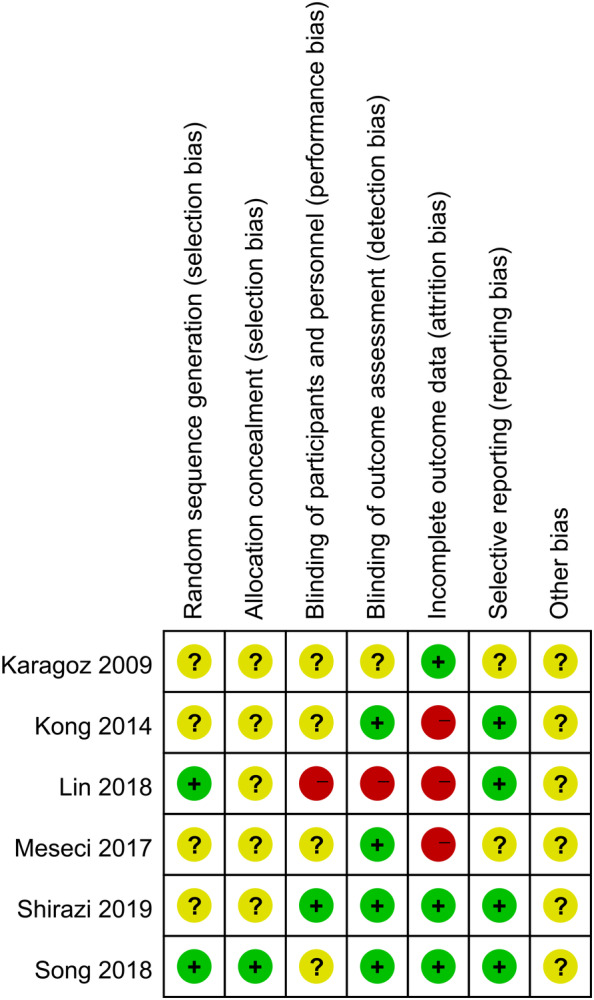
Qualitative assessment. Green circle = low bias risk, red circle = high bias risk, yellow circle = unclear bias risk
3.4. Topical silicone gel versus placebos or no treatment
The VSS score comparison between silicone gel group and placebo or no treatment group was conducted in four out of the six studies with a total of 259 patients.17, 18, 19, 21
In the comparison of scar vascularity, pliability, pigmentation, and height at 3‐month follow‐up, low heterogeneity was found across the studies (I 2 = 0, P > .1). A fixed‐effect mode was applied and the VSS scores were not significantly different in patients receiving silicone gel or those receiving placebos or no treatment for scar prevention (P > .05) (Figure 3). As for total VSS score comparison, a random‐effect mode was applied due to high heterogeneity (I 2 = 88%; P = .005). No statistically significant VSS score difference was pooled between the silicone gel group and the control group (SMD = −0.74; 95% CI: −1.94 to 0.46; P = .23) (Figure 3).
Figure 3.
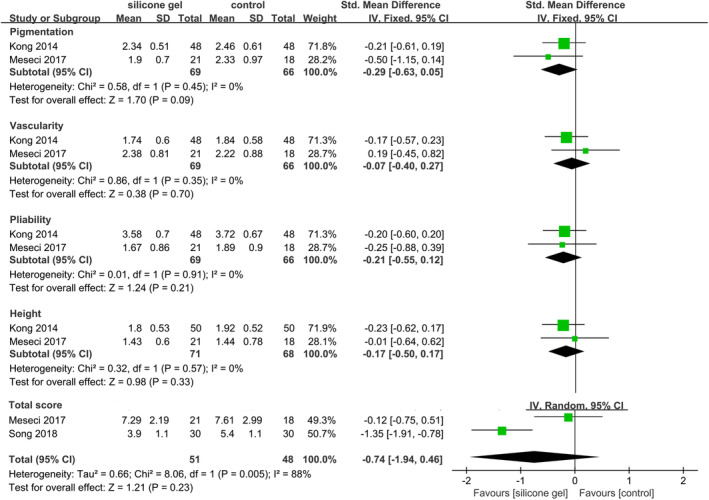
Forest plot comparison of Vancouver Scar Scale scores between silicone gel and placebos or no treatment at 3 months after surgery
For the comparison of pigmentation and height scores at 6‐ to 8‐month follow‐up, low heterogeneity was found among the studies (I 2 = 0, P = .71 and I 2 = 48%, P = .15 for pigmentation and height, respectively). A fixed‐effect mode was applied and the outcome showed that patients receiving silicone gel had significantly lower scores than those in the control group (SMD = −0.55, 95% CI: −0.83 to −0.26, P = .0002 and SMD = −0.73, 95% CI: −1.02 to 0.44, P < .00001 for pigmentation and height, respectively). In the comparison of vascularity and pliability scores at 6‐ to 8‐month follow‐up, a random‐effect mode was used due to high heterogeneity (I 2 = 60%, P = .08 and I 2 = 59%, P = .09 for vascularity and pliability, respectively). No statistically significant difference was pooled between the two groups for vascularity scores (SMD = −0.45; 95% CI: −0.92 to 0.01; P = .05), whereas significant lower pliability scores were found in the silicone gel group than in the placebo or no treatment group (SMD = −0.49; 95% CI: −0.95 to −0.03; P = .04) (Figure 4).
Figure 4.
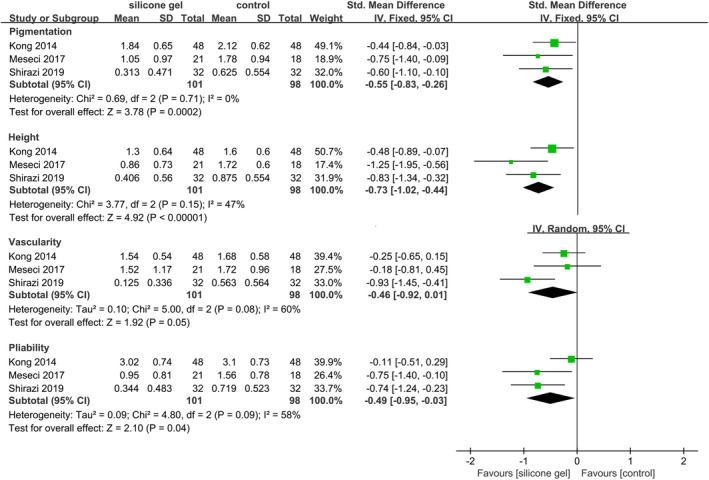
Forest plot comparison of Vancouver Scar Scale scores between silicone gel and placebos or no treatment at 6 to 8 months after surgery
3.5. Topical silicone gel versus silicone gel sheet
The VSS score comparison between silicone gel and silicone gel sheet was assessed in two studies with a total of 50 patients.20, 22 No heterogeneity was present in height, vascularity, pigmentation, and pliability score comparison, (I 2 = 0; P > .01) and a fixed‐effect mode was applied. The pooled estimate showed that no significant efficacy difference was present between silicone gel and silicone gel sheet (P > .05). (Figure 5).
Figure 5.
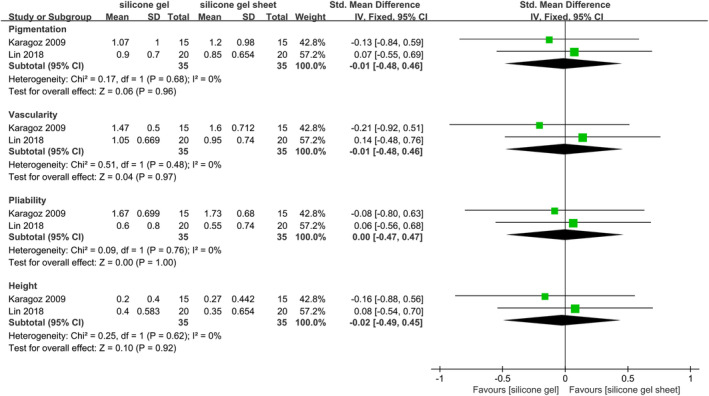
Forest plot comparison of Vancouver Scar Scale scores between silicone gel and silicone gel sheet
3.6. Topical silicone gel versus non‐silicone treatment
In the VSS total score comparison including 3 studies and 132 patients, significant heterogeneity was present (I 2 = 81%; P = .005) and a random‐effect mode was used for analysis.17, 18, 22 No significant efficacy difference was observed between patients using silicone gel and patients using non‐silicone treatment (SMD = −0.18; 95% CI: −1.02 to −0.65; P = .67) (Figure 6).
Figure 6.
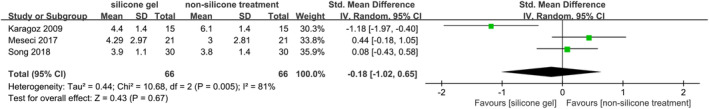
Forest plot comparison of Vancouver Scar Scale total scores between silicone gel and non‐silicone therapies
4. DISSCUSSION
The meta‐analysis by Hsu et al extracted occurrence rate of pathological scars, while our study extracted VSS scores and got contrary outcomes.7 Topical silicone gel was significantly more effective in post‐operative scar prevention than placebos or no treatment when evaluated at 6 or more months after surgery, especially for height, pigmentation, and pliability relief (P < .05). Nevertheless, no superior efficacy was pooled when the follow‐up period was 3 months (P > .05). The superior efficacy of topical silicone gel in VSS score reduction within 6 months after surgery was reported in several RCTs, which used VSS but were not included due to limited useful data.12, 13, 14, 15 In the recommendations by Gold et al, silicone‐based products were recommended with a 2‐month course for surgical or traumatic wounds, and if ineffective, alternative injection treatment was recommended.23 According to our meta‐analysis, the efficacy of silicone gel on post‐operative scar prevention may not be significant until 6 months after surgery. Thus, 2 months may not be long enough for topical silicone gel to show efficacy. We recommend that at least 2‐month application of topical silicone gel is needed and a longer than 6‐month follow‐up is necessary to validate its efficacy in scar prevention. Whether and how the length of treatment influences efficacy needs further research.
Despite our results favouring silicone gel being effective in scar prevention, in studies where POSAS were used, outcomes were conflicting. Bruijn et al reported that silicone gel group did not outperform no treatment group, yet meridian colour therapy showed promising scar prevention efficacy.24 The negative outcome was confirmed by Cadet et al where silicone gel did not outdo placebos at all.8 On the other hand, van der Wal et al reported that silicone gel could better relieve scar roughness and itching than placebos within 6 month after burns.9 The study by Bianchi et al also reported promising results for silicone gel in scar prevention.11 More high‐quality studies (Considering the fact that most of our involved studies were not double‐blind) using either VSS or POSAS are needed to clarify the efficacy of silicone gel in scar prevention.
Our result showed that no efficacy difference between silicone gel and silicone gel sheet was found in scar management. Although the two‐pooled studies compared silicone gel and silicone gel sheet for prevention efficacy and treatment efficacy respectively, our outcome was still an implication that the two forms of silicone‐based products were similarly effective. Our meta‐analysis outcome was confirmed by studies by Kim et al and Chang et al where gel and sheet performed equally in post‐operative scar prevention.16, 25 In addition, application of silicone gel and silicone gel sheet was comparably satisfactory by Visual Analogue Scale.20, 25 With comparable efficacy and safety, patient compliance may be another important factor for clinicians to consider. Kim et al reported that it was significantly more inconvenient for patients to use sheet than topical gel (P < .05).16 Clinicians are supposed to prescribe silicone gel or sheet considering different scar locations, lifestyles and ages of patients to achieve good compliance, and treatment efficacy at the same time.
Besides topical gel and sheet, cohesive silicone bandage, a new form of silicone‐based product, has shown better scar elasticity relief efficacy than silicone gel sheet.26 The authors explained that the betterment may come from unique microstructure of the bandage which ensured standardised pressure together with uninterrupted contact with the skin.26 Pressure therapy has been proved to be effective in hypertrophic burn scar treatment.27 Although both silicone gel and pressure therapy were effective, Wiseman et al reported that the combination of the two therapies did not outperform each treatment modality alone.10 Investigations into how pressure therapy should be correctly applied in scar management may help to develop new silicone‐based products and improve their efficacy.
All the non‐silicone therapies involved in our study were topical treatment and silicone gel was similarly effective to them (P > .05). Notably, scar treatment and prevention trials were also put together in this part of analysis. In our subgroup analysis, silicone gel performed significantly better than onion extract in post‐burn hypertrophic scar treatment but was similarly effective to onion extract in post‐operative scar prevention, and the subgroup difference was statistically significant (P = .008), which accounted for the high heterogeneity (Figure A1). The difference implied us that silicone gel was likely to be more effective in treatment setting rather than prevention setting.
Since, one topical therapy could hardly outperform another topical therapy; silicone gel combined treatment may yield more promising outcomes. Some combined treatment has already shown potential superior efficacy.28 The combination of herbal extracts and a silicone derivative has been reported to reduce scar development.29 Moreover, silicone gel combined with laser therapies has also shown promising efficacy in scar prevention.30, 31 In addition to combined treatment, we could also use methods like ultrasound or nanotechnology to improve the efficacy of single therapy. Wahba et al reported silicone gel phonophoresis outperformed steroid or onion extract phonophoresis for treating post‐burn hypertrophic scars.32 In a word, silicone gel as well as other silicone‐based products could serve as the “cornerstone” for various combined scar treatment, which is the future trend for scar management.
Several limitations should be considered when exploring our results. First, our meta‐analysis only included six studies and all the included studies had a sample size less than 100. Therefore, we may be subject to small‐effect bias. Second, several RCTs meeting our inclusion criteria reported outcomes in graphs, which could not be put in our quantitative analysis. If we could include these studies, more solid evidence was likely to be provided. Third, significant heterogeneity was present in our analysis. In the process of data search and analysis, application of various scar measurement tools in different studies was perplexing and brought difficulty in forming evidence‐based research. VSS and POSAS were the two most common subjective scar evaluation tools nowadays, but a recent study showed that objective evaluation presented better intra‐ and inter‐rater reliability, which helped inter‐study comparison.33 Besides causes illustrated above, the inferior inter‐rater reliability of VSS may also contribute to the heterogeneity observed in our analysis. Besides, as has been mentioned in the meta‐analysis by Hsu et al, scar locations could potentially influence treatment efficacy, therefore, could also more or less cause heterogeneity in our pooled analysis.7 Thus, we suggest that objective scar measurement and associated evidence should be taken and published more, and potential influencing factors like ages, scar types, and scar locations should also be investigated.
In conclusion, topical silicone gel was effective in the prevention of scars, although the efficacy may not be significant until around 6 months after surgery. The efficacy and safety profile of silicone gel was comparable to silicone gel sheet in scar management. No difference in treatment efficacy between topical silicone gel and other non‐silicone topical therapies including onion extract and steroid cream was found. However, most of the current trials investigated silicone gel as a preventive agent for scars and more studies using topical silicone gel or other silicone‐based products to treat hypertrophic scars or keloids are needed.
CONFLICT OF INTEREST
No conflicts of interest declared.
AUTHOR CONTRIBUTIONS
F. W. accounted for acquisition, analysis and interpretation of data, drafted the manuscript, and approved the version to be published. X. L. participated in the acquisition of data, and she also helped to draft and revise the manuscript and approved the version to be published. X. W. helped to draft and revise the manuscript and approved the version to be published. X. J. made substantial contributions to conception and design of the study, revised the manuscript, and approved the version to be published.
ACKNOWLEDGEMENTS
This study was supported by the National Natural Science Foundation of China, Grant/Award Number: 81872535.
APPENDIX A.
Figure A1.
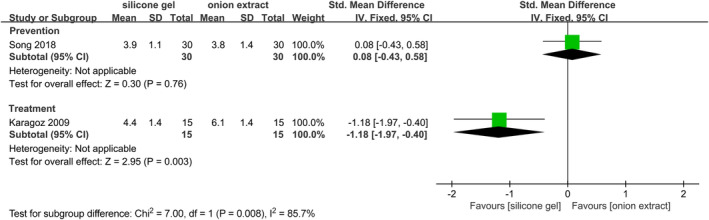
Forest plot comparison of efficacy between silicone gel and onion extract divided by application purpose
Wang F, Li X, Wang X, Jiang X. Efficacy of topical silicone gel in scar management: A systematic review and meta‐analysis of randomised controlled trials. Int Wound J. 2020;17:765–773. 10.1111/iwj.13337
Funding information National Natural Science Foundation of China, Grant/Award Number: 81872535
REFERENCES
- 1. Lonie S, Baker P, Teixeira RP. Healing time and incidence of hypertrophic scarring in paediatric scalds. Burns. 2017;43(3):509‐513. [DOI] [PubMed] [Google Scholar]
- 2. Kouotou EA, Nansseu JR, Omona Guissana E, et al. Epidemiology and clinical features of keloids in Black Africans: a nested case‐control study from Yaounde, Cameroon. Int J Dermatol. 2019;58(10):1135‐1140. [DOI] [PubMed] [Google Scholar]
- 3. Kant S, van den Kerckhove E, Colla C, van der Hulst R, Piatkowski de Grzymala A. Duration of scar maturation: retrospective analyses of 361 hypertrophic scars over 5 years. Adv Skin Wound Care. 2019;32(1):26‐34. [DOI] [PubMed] [Google Scholar]
- 4. Perkins K, Davey RB, Wallis KA. Silicone gel: a new treatment for burn scars and contractures. Burns Incl Therm Inj. 1983;9(3):201‐204. [DOI] [PubMed] [Google Scholar]
- 5. Meaume S, Le Pillouer‐Prost A, Richert B, Roseeuw D, Vadoud J. Management of scars: updated practical guidelines and use of silicones. Eur J Dermatol. 2014;24(4):435‐443. [DOI] [PubMed] [Google Scholar]
- 6. O'Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;9:CD003826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hsu KC, Luan CW, Tsai YW. Review of silicone gel sheeting and silicone gel for the prevention of hypertrophic scars and keloids. Wounds. 2017;29(5):154‐158. [PubMed] [Google Scholar]
- 8. Cadet N, Hardy I, Dudek D, et al. Prospective case‐control trial evaluating silicone gel for the treatment of direct brow lift scars. Can J Ophthalmol. 2018;53(1):29‐33. [DOI] [PubMed] [Google Scholar]
- 9. van der Wal MB, van Zuijlen PP, van de Ven P, Middelkoop E. Topical silicone gel versus placebo in promoting the maturation of burn scars: a randomized controlled trial. Plast Reconstr Surg. 2010;126(2):524‐531. [DOI] [PubMed] [Google Scholar]
- 10. Wiseman J, Ware RS, Simons M, et al. Effectiveness of topical silicone gel and pressure garment therapy for burn scar prevention and management in children: a randomized controlled trial. Clin Rehabil. 2019;34(1):120‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bianchi FA, Roccia F, Fiorini P, Berrone S. Use of Patient and Observer Scar Assessment Scale for evaluation of facial scars treated with self‐drying silicone gel. J Craniofac Surg. 2010;21(3):719‐723. [DOI] [PubMed] [Google Scholar]
- 12. Chan KY, Lau CL, Adeeb SM, Somasundaram S, Nasir‐Zahari M. A randomized, placebo‐controlled, double‐blind, prospective clinical trial of silicone gel in prevention of hypertrophic scar development in median sternotomy wound. Plast Reconstr Surg. 2005;116(4):1013‐1020. discussion 21‐2. [DOI] [PubMed] [Google Scholar]
- 13. Chittoria RK, Padi TR. A prospective, randomized, placebo controlled, double blind study of silicone gel in prevention of hypertrophic scar at donor site of skin grafting. J Cutan Aesthet Surg. 2013;6(1):12‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kwon SY, Park SD, Park K. Comparative effect of topical silicone gel and topical tretinoin cream for the prevention of hypertrophic scar and keloid formation and the improvement of scars. J Eur Acad Dermatol Venereol. 2014;28(8):1025‐1033. [DOI] [PubMed] [Google Scholar]
- 15. Nimpoonyakampong K, Somcharit L, Namviriyachote N, Praditsuktavorn B, Chinaroonchai K, Muangman P. Comparison of efficacy of herbal extract plus silicone gel and silicone gel for the prevention postburn hypertrophic scars. J Medl Assoc of Thailand. 2017;100(3 Supplement 2):S126‐S131. [Google Scholar]
- 16. Kim SM, Choi JS, Lee JH, Kim YJ, Jun YJ. Prevention of postsurgical scars: comparsion of efficacy and convenience between silicone gel sheet and topical silicone gel. J Korean Med Sci. 2014;29(Suppl 3):S249‐S253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Song T, Kim KH, Lee KW. Randomised comparison of silicone gel and onion extract gel for post‐surgical scars. J Obstet Gynaecol. 2018;38(5):702‐707. [DOI] [PubMed] [Google Scholar]
- 18. Meseci E, Kayatas S, Api M, Boza A, Cikman MS. Comparison of the effectiveness of topical silicone gel and corticosteroid cream on the pfannenstiel scar prevention—a randomized controlled trial. Ginekol pol. 2017;88(11):591‐598. [DOI] [PubMed] [Google Scholar]
- 19. Kong CG, Kim GH, Kim DW, In Y. The effect of topical scar treatment on postoperative scar pain and pruritus after total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134(4):555‐559. [DOI] [PubMed] [Google Scholar]
- 20. Lin YS, Ting PS, Hsu KC. Does the form of dressings matter? A comparison of the efficacy in the management of postoperative scars between silicone sheets and silicone gel: a randomized controlled trial. Medicine. 2018;97(32):e11767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shirazi M, Mohammadi AA, Shamohammadi I, Mahboubi A, Makarem A. Efficacy of silicone gel in reducing scar formation after hypospadias repair: a randomized placebo‐controlled trial. Res Rep Urol. 2019;11:291‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karagoz H, Yuksel F, Ulkur E, Evinc R. Comparison of efficacy of silicone gel, silicone gel sheeting, and topical onion extract including heparin and allantoin for the treatment of postburn hypertrophic scars. Burns. 2009;35(8):1097‐1103. [DOI] [PubMed] [Google Scholar]
- 23. Gold MH, McGuire M, Mustoe TA, et al. Updated international clinical recommendations on scar management: part 2—algorithms for scar prevention and treatment. Dermatol Surg. 2014;40(8):825‐831. [DOI] [PubMed] [Google Scholar]
- 24. de Bruijn CMA, Hoff FW, Bruggeman‐Westermann MM, et al. Optimizing VAP scars after childhood cancer treatment: a pilot study. Support Care Cancer. 2017;25(12):3651‐3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chang CS, Wallace CG, Hsiao YC, et al. Clinical evaluation of silicone gel in the treatment of cleft lip scars. Sci Rep. 2018;8(1):7422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moortgat P, Meirte J, Maertens K, Lafaire C, De Cuyper L, Anthonissen M. Can a cohesive silicone bandage outperform an adhesive silicone gel sheet in the treatment of scars? A randomized comparative trial. Plast Reconstr Surg. 2019;143(3):902‐911. [DOI] [PubMed] [Google Scholar]
- 27. Ai JW, Liu JT, Pei SD, et al. The effectiveness of pressure therapy (15‐25 mmHg) for hypertrophic burn scars: a systematic review and meta‐analysis. Sci Rep. 2017;7:40185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fang QQ, Chen CY, Zhang MX, et al. The effectiveness of topical anti‐scarring agents and a novel combined process on cutaneous scar management. Curr Pharm des. 2017;23(15):2268‐2275. [DOI] [PubMed] [Google Scholar]
- 29. Chuangsuwanich A, Arunakul S, Kamnerdnakta S. The efficacy of combined herbal extracts gel in reducing scar development at a split‐thickness skin graft donor site. Aesthetic Plast Surg. 2013;37(4):770‐777. [DOI] [PubMed] [Google Scholar]
- 30. Alberti LR, Vicari EF, De Souza Jardim Vicari R, Petroianu A. Early use of CO2 lasers and silicone gel on surgical scars: prospective study. Lasers Surg Med. 2017;49(6):570‐576. [DOI] [PubMed] [Google Scholar]
- 31. Safra T, Shehadeh W, Koren A, et al. Early intervention with pulse dye and CO2 ablative fractional lasers to improve cutaneous scarring post‐lumpectomy: a randomized controlled trial on the impact of intervention on final cosmesis. Lasers Med Sci. 2019;34(9):1881‐1887. [DOI] [PubMed] [Google Scholar]
- 32. Wahba ES, Hamada HA, Khatib AE. Effect of silicone gel versus Contractubex or corticosteroid phonophoresis for post‐burn hypertrophic scars: a single‐blind randomized controlled trial. Physiother Q. 2019;27(1):1‐5. [Google Scholar]
- 33. Lee KC, Bamford A, Gardiner F, et al. Investigating the intra‐ and inter‐rater reliability of a panel of subjective and objective burn scar measurement tools. Burns. 2019;45(6):1311‐1324. [DOI] [PMC free article] [PubMed] [Google Scholar]


