Dear Editors,
The malignant transformation of chronic wounds is rare and is seen most frequently in burn scars. Despite the infrequency of such a transformation, the management of chronic ulcers requires close follow up, including skin biopsies of all suspected lesions.
Chronic ulceration may predispose patients to the development of malignancies such as basal cell carcinoma, squamous cell carcinoma, leiomyosarcoma, and melanoma.1, 2 Here, we report a case of melanoma that arose in a chronic pressure ulcer.
A 35‐year‐old man developed a complication following an injection at 6 months of age, which resulted in paraplegia, but he remained ambulatory with the aid of a wheelchair. A pressure ulcer developed in the sacral area 15 years after his injury. He had been treated conservatively, which resulted in variation in the size of the ulcer over the past 19 years. However, the ulcer had grown in the last year.
On physical examination, the ulcer measured 10 × 6 × 1 cm (length, width, and depth), with a white hyperkeratotic crust and whitish‐grey discoloration (Figure 1). Multiple punch biopsies of the edge and central areas were performed repetitively. They were reported as lymphocyte infiltration because of chronic wound. Final biopsies were taken under dermoscopy. The histological examination demonstrated large round cells and atypical melanocytic hyperplasia, with irregularly sized nuclei. Immunohistochemically, the tumour cells stained positively with HMB 45 and SOX‐10. The Ki‐67 proliferation index was 30% (Figure 2). Based on these findings, melanoma was diagnosed.
Figure 1.

The ulcer was covered with white hyperkeratotic plaque and greyish discoloration
Figure 2.
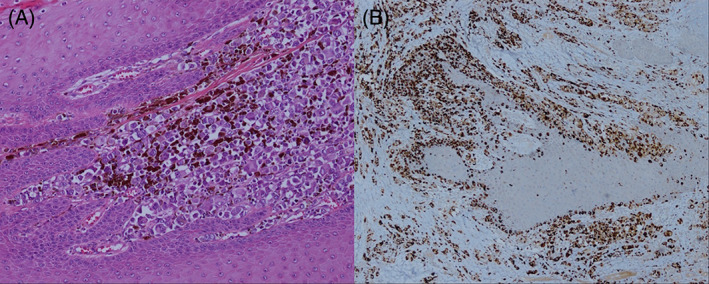
(A) Atypical melanocytes lining the dermoepidermal junction and extending into the dermis (haematoxylin eosin staining, ×100 magnification); (B) diffuse positivity in the tumour cells (HMB‐45 stain, ×40 magnification)
The lesion was excised widely with an internal hemipelvectomy; the anus was included, and a colostomy was opened. The para‐aortic lymph nodes were dissected at the same session. The final pathology report of the specimen was compatible with superficial spreading melanoma (Clark's level IV, Breslow 15 mm) (Figure 2). The dissected lymph nodes were negative for malignancy, and position emission tomography (PET) showed no findings suggesting distant metastasis.
The reason why a malignant transformation develops in chronic ulcers is unknown. Toxins released from the ulcer or repeated trauma to the ulcer may induce dormant preneoplastic cells.3 Neuman et al proposed that implantation of epithelial cells into the dermis provokes a foreign body reaction, resulting in chronic inflammation.4
A skin biopsy is recommended to look for malignant change if an ulcer is resistant to treatment. The malignancy most frequently associated with chronic ulcers is squamous cell carcinoma, followed by basal cell carcinoma and adenocarcinoma.2 Despite treatment, enlargement with discoloration was the primary finding in our patient. We advise close follow up and skin biopsies for growing, treatment‐resistant pressure ulcers.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest to disclose.
REFERENCES
- 1. Senet P, Combemale P, Debure C, et al. Malignancy and chronic leg ulcers: the value of systematic wound biopsies: a prospective, multicenter, cross‐sectional study. Arch Dermatol. 2012;148(6):704‐708. [DOI] [PubMed] [Google Scholar]
- 2. Combemale P, Bousquet M, Kanitakis J, Bernard P, Angiodermatology Group, French Society of Dermatology . Malignant transformation of leg ulcers: a retrospective study of 85 cases. J Eur Acad Dermatol Venereol. 2007;21(7):935‐941. [DOI] [PubMed] [Google Scholar]
- 3. Nthumba PM. Marjolin's ulcers: theories, prognostic factors and their peculiarities in spina bifida patients. World J Surg Oncol. December 5, 2010;8:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Neuman Z, Ben‐Hur N, Shulman J. Trauma and skin cancer: implantation of epidermal elements and possible cause. Plast Reconstr Surg. December 1963;32:649‐656. [DOI] [PubMed] [Google Scholar]


