Abstract
Frequently considered chronic wounds for reconstruction are wounds lacking healing progress despite good wound care. And those needing microsurgical reconstruction are chronic wounds that are unable to close by local flap or skin grafts, wounds with exposed vital structure such as tendon and bones, and wounds that have prolonged infections such as osteomyelitis and skin necrosis. The reconstruction for soft tissue defects not only aims to provide coverage but to restore function and acceptable form as well. Wound preparation prior to microsurgical reconstruction consists of improving or restoring vascular supply, stabilising skeletal structures, and obtaining clinically clean wounds. Microsurgery is a surgical discipline that combines magnification with a advanced microscope, specialised precision tools, and various operating techniques. Thus microsurgery allows flap to be transferred far from the donor site restoring form and function to areas of the body that have lost skin, fat, muscle movement, and/or skeletal support. Microsurgery has expanded reconstructive surgery's elements and strategies and is still evolving. Along with the multidisciplinary approach and good principle of wound care, the repair and restoration strategies using microsurgery have widened the possibilities for limb salvage from complex chronic wounds.
1. INTRODUCTION
As reconstructive surgeons, we are often consulted on difficult wounds that conservative care may not be enough to heal. Frequently considered chronic wounds for reconstruction are wounds lacking healing progress despite good wound care. And those needing microsurgical reconstruction are chronic wounds that are unable to close by local flap or skin grafts, wounds with exposed vital structure such as tendon and bones, and wounds that have prolonged infections such as osteomyelitis and skin necrosis. These chronic ulcers have become a major challenge to health care professionals all over the world. Reports show that in the United States alone, these wounds affect an estimated 2.4‐4.5 million people.1, 2 Chronic leg and foot ulcers occur in many adults with vascular disease or diabetes and are attributed to chronic venous insufficiency, arterial disease, prolonged pressure, or neuropathy.2, 3 Thus, chronic wounds can be classified as vascular ulcers (venous and arterial), diabetic ulcers, and pressure ulcers.4 These ulcers last on average 12 to 13 months, recur in up to 60% to 70% of patients, can lead to loss of function and decreased quality of life, and are a significant cause of morbidity.2, 3 Moreover, care for such conditions has been reported to cost 2% to 3% of the health care budgets in developed countries.2, 3 From the patient perspective, the most frightening fact may be that these chronic ulcers when left untreated or mistreated may lead to amputation. There are many reasons an amputation may be necessary. The most common is poor circulation because of damage or narrowing of the arteries, called peripheral arterial disease. Without adequate blood flow, the body's cells cannot take oxygen and nutrients they need from the bloodstream. As a result, the affected tissue begins to die and infection may set in. Causes for amputation other than from chronic wounds may include severe injury from trauma, cancer, uncontrolled infection, neuroma, uncontrolled chronic osteomyelitis, and frostbite. Although inevitable amputations do occur, reconstructive options may lead to limb salvage.5, 6
Today, the reconstruction for soft tissue defects aims not only to provide just coverage but to restore function and acceptable form as well. Once the wound is evaluated to have good or restored vascular supply, stable skeletal structures, and a relatively clean wound, soft tissue reconstruction is then considered. The concept of a reconstructive ladder was proposed to achieve wounds with adequate closure using a stepladder approach from simple to complex procedures. Although still valued and widely taught, the reconstructive ladder comes from the concept of the wound‐closure ladder that dates back beyond the era of modern reconstructive surgery.7 A skin graft after granulation over the exposed anterior tibial bone can still provide coverage but may end in inadequate coverage that can lead to complications such as additional soft‐tissue loss, osteomyelitis, functional loss, increased medical cost, unstable wounds, and even amputation. Using a well‐vascularised flap, whether it is a local or a free with adequate padding will provide superior results in addition to coverage. In addition, other techniques including tissue expansion, skin stretching, and negative pressure wound therapy have had a new impact in approaching reconstructive options.8 A simpler reconstructive option may not necessarily produce optimal results especially for lower‐extremity coverage. Thus to provide optimal form and function, we jump up and down the rungs of the ladder like getting off the elevator at the ideal floor. Restoring the missing components such as muscle, bone, and skin using a combined flap with the microsurgery approach may provide an ideal solution to complex defects. The reconstructive elevator requires creative thoughts and consideration of multiple variables to achieve the best form and function rather than a sequential climb up the ladder. (Figure 1) This paradigm of thought does not eliminate the concept of the reconstructive ladder but replaces it with a ladder of wound closure that makes its mark in the field where a variety of advanced reconstructive procedures and techniques is not readily available. Traditionally, upper and middle one third of the lower leg can be reconstructed with regional muscles like gastrocnemius and soleus muscles or by using perforator‐based local skin flaps also known as propeller flaps. However, because of the scarcity of available tissues, the lower third of the leg and the foot may require reconstruction using tissues distant from the defect when the defects are moderate or large. It involves using microsurgery. Microsurgery is a surgical discipline that combines magnification with an advanced microscope, specialised precision tools, and various operating techniques. These techniques are primarily used to anastomose small blood vessels (arteries and veins) and to coapt nerves. A flap is a piece of living tissue that carries its own blood supply and is moved from one area of the body to another. When the blood supply is cut (pedicle) and transferred far away from the original site, it becomes a free flap. By anastomosing the vessels from the flap (pedicle) to the recipient vessels, it restores the vascular supply to the flap and allows the distant flap to survive and provide adequate coverage. Flap surgery can restore form and function to areas of the body that have lost skin, fat, muscle movement, and/or skeletal support. Microsurgery will not only allow wound coverage but can entail restoration of function and form.
Figure 1.
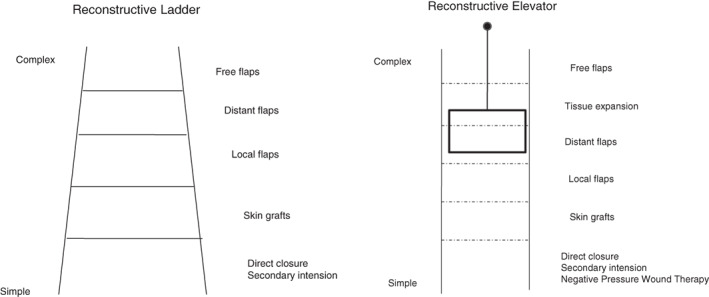
Reconstructive approach is shown comparing the classical reconstructive ladder to reconstructive elevator. The reconstructive elevator requires creative thoughts and consideration of multiple variables to achieve the best form and function rather than a sequential climb up the ladder
Thus, in chronic wounds where wound is stalling, complex, and challenging, using the microsurgery approach in conjunction with the multidisciplinary approach can provide adequate and timely coverage. In this review, we will focus on patient selection, mutidisciplanary approach, wound preparation, surgical techniques, and outcomes regarding microsurgical reconstruction using free flaps.
2. PATIENT SELECTION, MULTIDISCIPLINARY APPROACH, AND THE WOUND PREPARATION
The chronic wounds that are considered for reconstructive microsurgery may occur from various causes such as diabetic foot ulcers with or without ischaemia and infection, pressure sores, radiation wounds, chronic osteomyelitis, unstable scar, and poorly managed complex traumatic wounds. Table 1 shows our experience that needed microsurgical reconstruction in the last 7 years. If the wound is small enough with good regional vascular supply such as pressure sores for ankle region or a small neuropathic diabetic foot ulcers, local flaps may be enough to reconstruct the defect. However, for large and complex wounds, a microsurgical approach can provide an efficient solution. In addition to the wound, the patient has to be ambulating prior to reconstruction, will likely be able to ambulate after reconstruction, have reasonable systemic condition to overcome the challenges of multiple surgeries, psychologically motivated, and have good family support.9
Table 1.
Chronic wounds that underwent microsurgical reconstruction
| Diagnosis | N | % |
|---|---|---|
| Burger's disease | 3 | 0.69 |
| COM | 125 | 28.60 |
| Diabetic foot | 214 | 48.97 |
| Exposed femoral artery graft | 1 | 0.23 |
| Foreign body leg Rt | 1 | 0.23 |
| Pressure sore | 3 | 0.69 |
| Post traumatic/burn scar contracture | 18 | 4.12 |
| Pyoderma gangrenosum | 1 | 0.23 |
| Radiation ulcer | 5 | 1.14 |
| Unstable scar | 66 | 15.10 |
| Total | 437 | 100.00 |
Abbreviation: COM, chronic osteomyeltis.
When considering these patients for microsurgical reconstruction, a holistic/multidisciplinary approach for the patient must commence concurrently with wound management.6, 10, 11 Without controlling the underlying factors involved in the pathology of the ulcer, it will have higher chance for complications. For example, diabetic patients will need to address the issues to control their hyperglycaemia, renal insufficiency, nutrition, and other associated medical comorbidities that may adversely affect the healing requiring close collaboration with endocrinologist.12, 13 Vascular interventionist or vascular surgeons needs to be involved to evaluate and improve the vascular status. One must maximise the circulation of the leg for reconstruction.6, 14, 15 The exact roles of endovascular and open bypass procedures are still evolving, but are primarily determined by arterial anatomy, wound severity, and patient comorbidities.15, 16 Whatever the method, it is imperative to restore as much blood flow as possible to the foot so it can be adequately used as a recipient vessel.17, 18 The orthopaedic surgeons or podiatrists need to be involved to evaluate the skeletal status of the lower leg or foot when indicated. With multiple departments involving, the clinical nurse specialist plays a central role in maintaining clear communication and efficient treatment solution in the front line of management. An algorithm to consider wounds for the microsurgical approach is shown in Figure 2.
Figure 2.
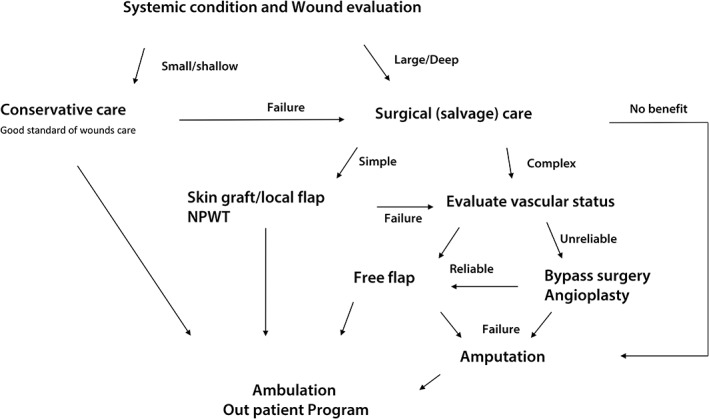
Algorithm for reconstruction is presented
Controlling infection is also an important factor to address. Poorly controlled infection may cause late stage flap failures often leading to amputations.19, 20, 21 When skin tissue is not clearly demarcated, the use of hyperbaric oxygen therapy can be helpful to achieve demarcation of the necrotic and viable tissue. In cases where bone infection is suspected, complete excision of the bone at the time of coverage is essential followed by antibiotic use.22, 23 Bone gaps can be filled by temporary cement mixed with antibiotics to occupy the space and the flap coverage performed. After the eradication of the infected bone, the cement can be removed during the second stage surgery replacing it with bone grafts or flaps. When considered for microsurgical reconstruction, the wound preparation process may easily be overlooked. However, preparing the wound adequately addressing vascularity, infection, dead space, and stability of the skeletal structure will lead to a better outcome.24, 25
3. SURGICAL TECHNIQUES
The first surgical step of treatment for chronic wound is to evaluate, debride, and treat infection.26 Optimal management of chronic wound and especially diabetic foot infection can potentially reduce incidence of major limb amputations and other related morbidities. All non‐viable and infected soft tissue and bone should be excised during debridement. Milking along the proximal tendon can be helpful to identify and limit ascending infection especially for diabetic foot wounds. Tissue culture should be sent and antibiotics used accordingly. Sufficient irrigation should follow after debridement to reduce bacterial count.27 The use of a hydrosurgery system may allow us to efficiently debride large extensive wounds by preserving viable tissues and irrigating simultaneously.28 The understanding of vascular distribution of the foot, angiosome, helps to plan not only reconstruction but debridement especially in legs with limited vascularity.29 Performing debridement according to the angiosome territory, one may enhance flap survival by increasing the chance for marginal vascularisation from healthy surrounding angiosome territory.18 Repetitive debridement should be performed as part of wound preparation for reconstruction while monitoring c‐reactive protein for possible hidden infections and using it as an index for possible infection after reconstruction. In chronic wounds, thorough debridement may lead to what it seems like an irreparable wound that may warrant amputation. Microsurgical procedures, including soft tissue and bone flaps, and vessel and nerve grafting, can be used to reconsider problems such as defects with replaceable parts.
Once an adequate debridement and reasonable vascular perfusion is achieved, for extensive and complex defects, microsurgical reconstruction is considered. The biggest challenge in reconstructive microsurgery for chronic wounds especially diabetic foot is finding the recipient vessel. Even with an adequate flow to the foot, atherosclerosis of the artery may make anastomosis very difficult. If a named artery will be used as recipient, one must try to find a small segment spared from calcification.6 One must remember, especially for the ischaemic limb, that it was the initial poor vascular supply that caused the wound formation and thus all efforts should be made to preserve the distal flow to the foot. Microsurgical techniques such as end‐to‐side anastomosis, T‐style flow through or end‐to‐end on a branch of a major artery will minimise the steal phenomenon where flow may be diverted to the low‐resistance vascular bed of the new flap.30, 31 Another challenge for chronic conditions with inflammation like chronic osteomyelitis or radiation wounds is the scarring of the tissues. It can make the dissection for the recipient vessels very difficult. Thus, searching the recipient vessel out of the zone of injury or inflammation may make the search easier and reliable.
After debridement and recipient vessels secured, one can estimate the flap pedicle length and proceed to flap selection. The flap for reconstruction of chronic wounds has to provide a well‐vascularised tissue to control infection, allow adequate contour for footwear, be durable, and provide solid anchorage to resist shearing forces. In cases with large dead spaces, a flap should be selected to provide obliteration of the dead space as well. Controversy still remains that flap, whether muscle flaps with skin grafts, fasciocutanous flaps, and recently added perforator flaps, offers the optimal solution to reconstruct the wound especially the weight‐bearing foot. However, as long as the large defect is covered with any well‐vascularised tissue, it will provide an independent and well‐nourished vascular supply to eradicate infection, increase local oxygen tension, enhancing antibiotics activity, and neovascularisation to the adjacent ischaemic tissue.6, 32, 33 One of the basic elements of plastic surgery is to replace like with like. Thus for defects with skin defects, we are shifting towards using perforator flaps such as anterolateral thigh (ALT) perforator flap, thoracodarsal artery perforator (TDAP) flap, and superficial circumflex iliac perforator (SCIP) flap as it provides, a thin flap to minimise shearing, can take only the superficial fat to imitate the fibrous septa of the sole to adhere tightly, enhance neovascularisation of the subdermal plexus with adjacent tissue, and provide adequate blood supply to fight infection.5, 6, 17, 18, 24, 34 The elevation technique of each individual flap is described in detail in the referenced articles.
After the flap is elevated, the small artery and vein(s) are anastomosed under a microscope or a high loupe magnification. Nylon 9‐0 or 10‐0 sutures can be used to anastomose vessels of 1 to 2 mm diameters. Recently, a new technique called supermicrosurgery is being used to anastomose vessels at a perforator level.17, 18, 35, 36, 37, 38 The concept of supermicrosurgery introduced by Koshima et al has increased the popularity of perforator flaps and lymphatic surgery anastomosing vessels ranging from 0.3 to 0.8 mm in diameter.37, 38 The value of supermicrosurgery especially in diabetic foot reconstruction is further increased by allowing anastomosis in collateral vessels. The collateral vessels usually develop over the ischaemic transition period allowing alternative circulation of the skin of the distal leg and foot.39 These collateral vessels will often originate from the adjacent angiosome territory and when this formation of collateral is not enough, the skin will start to deteriorate as oxygen supply slowly diminishes.18 The reconstruction by perforator flap using the supermicrosurgery approach provides well‐vascularised tissue that covers diabetic foot defect without being dependent on major vessels.
Vigilant postoperative care is needed after microsurgical reconstruction as flows to the flap can be suddenly impaired because of multiple reasons including mechanical compression to the pedicle, faulty anastomosis, and low systolic blood pressure to name a few. However, usually after 2 days of uneventful monitoring, one can expect a relatively good outcome as most of thrombosis occurs within the first 2 days.40, 41
3.1. Case examples
3.1.1. Case 1
A 56‐year‐old male diabetic patient visited the clinic with chronic osteomyelitis of his right foot. The third and the fourth toes were previously amputated and healed but a small diabetic ulcer recurred, which led to osteomyelitis of the fourth metatarsal bone (Figure 3A). The pulses were weak on the dorsalis pedis artery and angioplasty was carried out opening the narrow femoral artery segment improving the flow to the leg (Figure 3B). The blood sugar was stable prior to surgery and antibiotics started accordingly. After wide debridement of the bone and soft tissue, recipient vessels were dissected and showed adequate pulse and flow (Figure 3C). An ALT perforator flap was elevated and then the pedicle was anastomosed to the dorsalis artery (end to side) and vein (end to end) (Figure 3D,E). The follow‐up at 2 years shows good contour and the patient with good gait (Figure 3F‐H).
Figure 3.
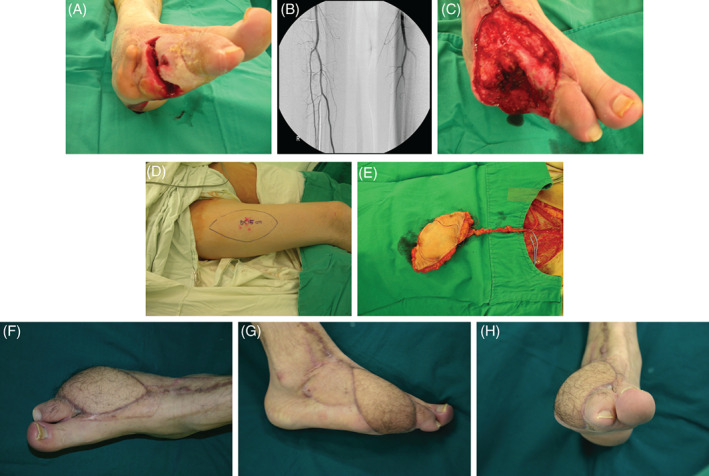
A 56‐year old male diabetic is shown with chronic osteomyelitis of his right foot (A). The pulses were weak on the dorsalis pedis artery and angioplasty was carried out opening the narrow femoral artery segment improving the flow to the leg (B). After wide debridement of the bone and soft tissue, recipient vessels were dissected and showed adequate pulse and flow (C). An anterolateral thigh (ALT) perforator flap was elevated and then the pedicle was anastomosed to the dorsalis artery (end to side) and vein (end to end) (D,E). The follow up at 2 years shows good contour and the patient with good gait (F‐H)
3.1.2. Case 2
A 53‐year old female patient is shown with an unstable scar with chronic ulceration on the distal end of the right foot. After trauma, the patient underwent skin graft that led to bone to skin coverage (Figure 4A,B). Severe pain and recurrent ulcers were noted and thus warranted microsurgical reconstruction using an SCIP flap. After removal of the scar tissues of the distal foot, it was reconstructed with the 15 × 6 cm flap (Figure 4C,D). At postoperative 12 months, the symptoms were alleviated without recurrence of ulcers (Figure 4E,F).
Figure 4.
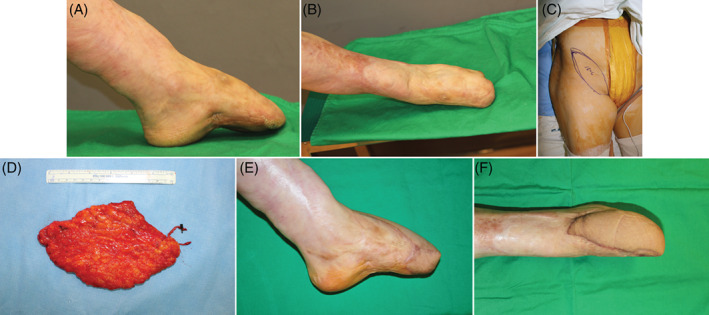
A 53 year old female patient is shown with an unstable scar with chronic ulceration on the distal end of the right foot. After trauma the patient underwent skin graft which led to bone to skin coverage (A,B). Severe pain and recurrent ulcers were noted and thus warranted microsurgical reconstruction using an superficial circumflex iliac perforator (SCIP) flap. After removal of the scar tissues of the distal foot it was reconstructed with the 15 × 6 cm flap (C,D). At postoperative 12 months, the symptoms were alleviated without recurrence of ulcers (E,F)
3.2. Outcomes
The spectrum of treatment for chronic wounds can be wide: Addressing systemic issues like blood sugar control and nutrition, family support, good standard of care, providing advanced care such as negative pressure wound therapy, hyperbaric oxygen, and cell therapy, to surgical options. Without the ability to have reconstruction in the treatment options, the spectrum of care is not optimal. Conversely, without a team with multidisciplinary offerings, the care would not be complete. No services can provide the care that is needed, which are all interconnected. With the introduction of the multidisciplinary approach, the goal and trend of management has shifted away from major amputation towards limb salvage for complex chronic wounds.11 Addressing the issues of perfusion, infection, wound treatment, skeletal stability, and biomechanics, now we are able to increase the salvage rate. Examples of such multidisciplinary approaches have shown to reduce major amputation at 3% to 4% in diabetic foot as we have seen at our centre.42, 43 We must have good clinical judgement whether to amputate or not weighing against clinical situations with systemic sepsis, major tissue loss, significant comorbid factors, poor patient compliance, and non‐reconstructable peripheral vascular disease. A non‐healing ulcer itself should not be considered an indication for amputation but be systemically approached by various disciplines of medicine.44, 45 The majority of reconstruction that needs microsurgical reconstruction are complex defects from diabetic foot, unstable scars, radiation ulcers, and chronic osteomyelitis as shown in Table 1.
The general success rate for these patients was the same as that for the patients with other chronic wounds whereas the diabetic foot had a slightly lower success rate. However, limb salvage from diabetic foot using the microsurgical approach showed success comparable to non‐diabetic patients.9, 34, 46, 47, 48, 49 Meta‐analysis of a systematic review of free tissue transfer in 528 diabetes patients in 18 studies showed that flap survival was 92% and the limb salvage rate was 83.4% over a 28 months average follow‐up period. This study indicates that free tissue transfer in the management of non‐traumatic lower‐extremity wounds in patients with diabetes may avoid amputations.9 In our previous study, we showed similar findings using microsurgery, which achieved an overall flap survival rate of 91.7%, a limb salvage rate of 84.9%, and 5‐year‐survival of 86.8%.5 Now with the introduction of supermicrosurgery, we are able to use small vessels to perform reconstruction even on the patients with poor vascular status. In our recent publication of 95 cases that used the supermicrosurgery approach, we noted 9 total loss and 12 cases of minor complication.18 Thirty‐four patients had one or less major artery after intervention but only had four cases of total failure. The lack of major vessels was not a significant risk for failure thus supporting our approach of using collateral vessels for recipients. Overall in this series, the flap survival rate was 90.5% and the overall limb salvage rate was 93.7%.18 This approach extends the possibility for reconstruction in patients with severe ischaemic diabetic foot.
In chronic osteomyelitis, our experience of microsurgical reconstruction using perforator flaps showed a flap survival of 95.8%.24 The treatment has similar principles that require aggressive surgical debridement removing all fibrotic and ischaemic bone and soft tissue surrounding the wound that impedes antibiotic delivery followed by definitive reconstruction with the objective of restoring ambulatory function.26 In the last three decades, major surgical advancements to provide vascularised coverage to infected bone had brought recurrence rates in chronic osteomyelitis down from 30% to 10%‐15%.50, 51 Reconstruction can be complex applying combine flaps to obliterate the dead space, reconstruct the bone defect, and resurface the skin defect. With a multidisciplinary approach using proper antibiotics and a surgical approach, the recurrence rate after reconstruction was 8.3%, the primary remission rate was 91.6%, the secondary remission rate was 98.3%, and the amputation rate was 1% in our series.24 Significant predictors of recurrence were peripheral vascular disease and major vessel compromise, which had 5.1 times higher odds of recurrence.24
Unstable scars frequently go through a wax and wane progress of healing for ulcers. It may also cause severe contracture as the scars mature during healing. It hinders the daily activities of the patient as epithelialisation can easily breakdown despite minimal stimuli. This occurs because of the lack of padding and durability of normal cutaneous structure. In the cases of severe contracture, there is an absolute lack of normal skin after release. When there is extensive defect after removal of unstable scar, microsurgical reconstruction is required. The principle of aggressive debridement followed by definitive surgery is applied and this problem can be overcome. The same can be said for radiation‐induced scars. The outcome may be similar to any non‐diabetic microsurgical reconstruction.
4. CONCLUSION
Microsurgery has expanded reconstructive surgery's elements and strategies and is still evolving. Along with the multidisciplinary approach and good principle of wounds care, the repair and restoration strategies using microsurgery have widened the possibilities for limb salvage from complex chronic wounds.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Suh HP, Hong JP. The role of reconstructive microsurgery in treating lower‐extremity chronic wounds. Int Wound J. 2019;16:951–959. 10.1111/iwj.13127
REFERENCES
- 1. Brownrigg JR, Apelqvist J, Bakker K, Schaper NC, Hinchliffe RJ. Evidence‐based management of PAD & the diabetic foot. Eur J Vasc Endovasc Surg. 2013;45(6):673‐681. [DOI] [PubMed] [Google Scholar]
- 2. Richmond NA, Maderal AD, Vivas AC. Evidence‐based management of common chronic lower extremity ulcers. Dermatol Ther. 2013;26(3):187‐196. [DOI] [PubMed] [Google Scholar]
- 3. Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care (New Rochelle). 2015;4(9):560‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nunan R, Harding KG, Martin P. Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis Model Mech. 2014;7(11):1205‐1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oh TS, Lee HS, Hong JP. Diabetic foot reconstruction using free flaps increases 5‐year‐survival rate. J Plast Reconstr Aesthet Surg. 2013;66(2):243‐250. [DOI] [PubMed] [Google Scholar]
- 6. Hong JP, Oh TS. An algorithm for limb salvage for diabetic foot ulcers. Clin Plast Surg. 2012;39(3):341‐352. [DOI] [PubMed] [Google Scholar]
- 7. Gottlieb LJ, Krieger LM. From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg. 1994;93(7):1503‐1504. [DOI] [PubMed] [Google Scholar]
- 8. Janis JE, Kwon RK, Attinger CE. The new reconstructive ladder: modifications to the traditional model. Plast Reconstr Surg. 2011;127(suppl 1):205S‐212S. [DOI] [PubMed] [Google Scholar]
- 9. Fitzgerald O'Connor EJ, Vesely M, Holt PJ, Jones KG, Thompson MM, Hinchliffe RJ. A systematic review of free tissue transfer in the management of non‐traumatic lower extremity wounds in patients with diabetes. Eur J Vasc Endovasc Surg. 2011;41(3):391‐399. [DOI] [PubMed] [Google Scholar]
- 10. Brocco E, Ninkovic S, Marin M, et al. Diabetic foot management: multidisciplinary approach for advanced lesion rescue. J Cardiovasc Surg (Torino). 2018;59(5):670‐684. [DOI] [PubMed] [Google Scholar]
- 11. Wraight PR, Lawrence SM, Campbell DA, Colman PG. Creation of a multidisciplinary, evidence based, clinical guideline for the assessment, investigation and management of acute diabetes related foot complications. Diabet Med. 2005;22(2):127‐136. [DOI] [PubMed] [Google Scholar]
- 12. Endara M, Masden D, Goldstein J, Gondek S, Steinberg J, Attinger C. The role of chronic and perioperative glucose management in high‐risk surgical closures: a case for tighter glycemic control. Plast Reconstr Surg. 2013;132(4):996‐1004. [DOI] [PubMed] [Google Scholar]
- 13. Patel GK. The role of nutrition in the management of lower extremity wounds. Int J Low Extrem Wounds. 2005;4(1):12‐22. [DOI] [PubMed] [Google Scholar]
- 14. Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95(8):875‐883. [DOI] [PubMed] [Google Scholar]
- 15. Darling JD, McCallum JC, Soden PA, et al. Results for primary bypass versus primary angioplasty/stent for lower extremity chronic limb‐threatening ischemia. J Vasc Surg. 2017;66(2):466‐475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bradbury AW, Adam DJ, Bell J, et al. Multicentre randomised controlled trial of the clinical and cost‐effectiveness of a bypass‐surgery‐first versus a balloon‐angioplasty‐first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The bypass versus angioplasty in severe Ischaemia of the leg (BASIL) trial. Health Technol Assess. 2010;14(14):1‐210. iii‐iv. [DOI] [PubMed] [Google Scholar]
- 17. Suh HS, Oh TS, Hong JP. Innovations in diabetic foot reconstruction using supermicrosurgery. Diabetes Metab Res Rev. 2016;32(suppl 1):275‐280. [DOI] [PubMed] [Google Scholar]
- 18. Suh HS, Oh TS, Lee HS, et al. A new approach for reconstruction of diabetic foot wounds using the Angiosome and Supermicrosurgery concept. Plast Reconstr Surg. 2016;138(4):702e‐709e. [DOI] [PubMed] [Google Scholar]
- 19. Wax MK, Rosenthal E. Etiology of late free flap failures occurring after hospital discharge. Laryngoscope. 2007;117(11):1961‐1963. [DOI] [PubMed] [Google Scholar]
- 20. Bild DE, Selby JV, Sinnock P, Browner WS, Braveman P, Showstack JA. Lower‐extremity amputation in people with diabetes. Epidemiology and prevention. Diabetes Care. 1989;12(1):24‐31. [DOI] [PubMed] [Google Scholar]
- 21. Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care. 1998;21(5):855‐859. [DOI] [PubMed] [Google Scholar]
- 22. Aragon‐Sanchez J, Lipsky BA. Modern management of diabetic foot osteomyelitis. The when, how and why of conservative approaches. Expert Rev Anti Infect Ther. 2018;16(1):35‐50. [DOI] [PubMed] [Google Scholar]
- 23. Allahabadi S, Haroun KB, Musher DM, Lipsky BA, Barshes NR. Consensus on surgical aspects of managing osteomyelitis in the diabetic foot. Diabet Foot Ankle. 2016;7:30079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hong JPJ, Goh TLH, Choi DH, Kim JJ, Suh HS. The efficacy of perforator flaps in the treatment of chronic osteomyelitis. Plast Reconstr Surg. 2017;140(1):179‐188. [DOI] [PubMed] [Google Scholar]
- 25. Knox KR, Datiashvili RO, Granick MS. Surgical wound bed preparation of chronic and acute wounds. Clin Plast Surg. 2007;34(4):633‐641. [DOI] [PubMed] [Google Scholar]
- 26. Attinger CE, Bulan EJ. Debridement. The key initial first step in wound healing. Foot Ankle Clin. 2001;6(4):627‐660. [DOI] [PubMed] [Google Scholar]
- 27. Badia JM, Torres JM, Tur C, Sitges‐Serra A. Saline wound irrigation reduces the postoperative infection rate in Guinea pigs. J Surg Res. 1996;63(2):457‐459. [DOI] [PubMed] [Google Scholar]
- 28. Granick M, Boykin J, Gamelli R, Schultz G, Tenenhaus M. Toward a common language: surgical wound bed preparation and debridement. Wound Repair Regen. 2006;14(suppl 1):S1‐S10. [DOI] [PubMed] [Google Scholar]
- 29. Clemens MW, Attinger CE. Angiosomes and wound care in the diabetic foot. Foot Ankle Clin. 2010;15(3):439‐464. [DOI] [PubMed] [Google Scholar]
- 30. Rainer C, Schwabegger AH, Meirer R, Perkmann R, Ninkovic M. Microsurgical management of the diabetic foot. J Reconstr Microsurg. 2003;19(8):543‐553. [DOI] [PubMed] [Google Scholar]
- 31. Sonntag BV, Murphy RX Jr, Chernofsky MA, Chowdary RP. Microvascular steal phenomenon in lower extremity reconstruction. Ann Plast Surg. 1995;34(3):336‐339. discussion 9‐40. [DOI] [PubMed] [Google Scholar]
- 32. Shestak KC, Hendricks DL, Webster MW. Indirect revascularization of the lower extremity by means of microvascular free‐muscle flap‐‐a preliminary report. J Vasc Surg. 1990;12(5):581‐585. [DOI] [PubMed] [Google Scholar]
- 33. Chang N, Mathes SJ. Comparison of the effect of bacterial inoculation in musculocutaneous and random‐pattern flaps. Plast Reconstr Surg. 1982;70(1):1‐10. [DOI] [PubMed] [Google Scholar]
- 34. Hong JP. Reconstruction of the diabetic foot using the anterolateral thigh perforator flap. Plast Reconstr Surg. 2006;117(5):1599‐1608. [DOI] [PubMed] [Google Scholar]
- 35. Hong JP. The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009;123(1):230‐235. [DOI] [PubMed] [Google Scholar]
- 36. Hong JP, Koshima I. Using perforators as recipient vessels (supermicrosurgery) for free flap reconstruction of the knee region. Ann Plast Surg. 2010;64(3):291‐293. [DOI] [PubMed] [Google Scholar]
- 37. Koshima I, Yamamoto T, Narushima M, Mihara M, Iida T. Perforator flaps and supermicrosurgery. Clin Plast Surg. 2010;37(4):683‐689. vii‐iii. [DOI] [PubMed] [Google Scholar]
- 38. Masia J, Olivares L, Koshima I, et al. Barcelona consensus on supermicrosurgery. J Reconstr Microsurg. 2014;30(1):53‐58. [DOI] [PubMed] [Google Scholar]
- 39. Suh HP, Kim Y, Suh Y, Hong J. Multidetector computed tomography (CT) analysis of 168 cases in diabetic patients with Total superficial femoral artery occlusion: is it safe to use an anterolateral thigh flap without CT angiography in diabetic patients? J Reconstr Microsurg. 2018;34(1):65‐70. [DOI] [PubMed] [Google Scholar]
- 40. Kroll SS, Schusterman MA, Reece GP, et al. Timing of pedicle thrombosis and flap loss after free‐tissue transfer. Plast Reconstr Surg. 1996;98(7):1230‐1233. [DOI] [PubMed] [Google Scholar]
- 41. Chen KT, Mardini S, Chuang DC, et al. Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast Reconstr Surg. 2007;120(1):187‐195. [DOI] [PubMed] [Google Scholar]
- 42. Krishnan N, Becker DF. Characterization of a bifunctional PutA homologue from Bradyrhizobium japonicum and identification of an active site residue that modulates proline reduction of the flavin adenine dinucleotide cofactor. Biochemistry. 2005;44(25):9130‐9139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Holstein P, Ellitsgaard N, Olsen BB, Ellitsgaard V. Decreasing incidence of major amputations in people with diabetes. Diabetologia. 2000;43(7):844‐847. [DOI] [PubMed] [Google Scholar]
- 44. Apelqvist J. Wound healing in diabetes. Outcome and costs. Clin Podiatr Med Surg. 1998;15(1):21‐39. [PubMed] [Google Scholar]
- 45. Cavanagh PR, Ulbrecht JS, Caputo GM. The non‐healing diabetic foot wound: fact or fiction? Ostomy Wound Manage. 1998;44(3A suppl):6S‐12S. discussion 3S. [PubMed] [Google Scholar]
- 46. Colen LB. Limb salvage in the patient with severe peripheral vascular disease: the role of microsurgical free‐tissue transfer. Plast Reconstr Surg. 1987;79(3):389‐395. [DOI] [PubMed] [Google Scholar]
- 47. Searles JM Jr, Colen LB. Foot reconstruction in diabetes mellitus and peripheral vascular insufficiency. Clin Plast Surg. 1991;18(3):467‐483. [PubMed] [Google Scholar]
- 48. Shenaq SM, Dinh TA. Foot salvage in arteriolosclerotic and diabetic patients by free flaps after vascular bypass: report of two cases. Microsurgery. 1989;10(4):310‐314. [DOI] [PubMed] [Google Scholar]
- 49. Oishi SN, Levin LS, Pederson WC. Microsurgical management of extremity wounds in diabetics with peripheral vascular disease. Plast Reconstr Surg. 1993;92(3):485‐492. [DOI] [PubMed] [Google Scholar]
- 50. Shannon JG, Woolhouse FM, Eisinger PJ. The treatment of chronic osteomyelitis by saucerization and immediate skin grafting. Clin Orthop Relat Res. 1973;96:98‐107. [PubMed] [Google Scholar]
- 51. Anthony JP, Mathes SJ, Alpert BS. The muscle flap in the treatment of chronic lower extremity osteomyelitis: results in patients over 5 years after treatment. Plast Reconstr Surg. 1991;88(2):311‐318. [DOI] [PubMed] [Google Scholar]


