Abstract
The burdens caused by chronic wounds on the affected persons themselves and also on the health care system are well recognised. The aim of this study was to investigate the prevalence and risk factors of chronic wounds in German nursing homes. An annual cross‐sectional study was conducted in nursing home residents from 2012 to 2018. The proportion of men affected by chronic wounds was to some extent higher than that of women, 9.0% males vs 7.5% females. In total, 7.8% of all residents were affected by chronic wounds. Of all residents with a chronic wound, 50.5% were affected by pressure ulcer. Male residents were twice as often affected by diabetic foot ulcer than female residents (18.0% vs 8.9%; P = 0.002). Bivariate analysis showed that chronic wounds were highly associated with poor nutrition, urinary incontinence, stool incontinence, diabetes mellitus, and limited mobility (P = 0.000). According to multivariate analysis, the strongest predictors for chronic wounds were limited mobility and diabetes mellitus. The highest prevalence of chronic wounds was in residents who were not restricted in their mobility, had diabetes, were male, and lived in a metropolitan region (23.7%). This study identified the prevalence and risk factors of chronic wounds in nursing home residents. Further research is needed to identify causal factors of the gender difference in the prevalence of chronic wounds. This may have an impact on the choice of prophylactic and therapeutic measures.
Keywords: chronic wounds, diabetes mellitus, limited mobility, nursing homes, pressure ulcer
1. INTRODUCTION
Chronic wounds are a serious, protracted, and costly health problem and occur in all health care settings. 1 Every chronic wound affects the quality of life of the persons affected in physical, emotional, social, and functional terms. 2
An often‐cited definition of chronic wounds is from Lazarus, Cooper 3 : “Chronic wounds have failed to proceed through an orderly and timely process to produce anatomic and functional integrity, or proceeded through the repair process without establishing a sustained anatomic and functional result”. 4 , 5 , 6 The two most commonly used definitions in Germany are: Wounds are defined as chronic if they “show no signs of healing within 4–12 weeks of the wound developing under professional therapy.” 7 or according to the Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. ‐ German Working Group of the Scientific Medical Societies (AWMF) S3 guideline “as loss of integrity of the skin and one or more underlying structures with a lack of healing within eight weeks”. 8 Various wound types that often count as chronic wounds are pressure ulcer (PU), lower leg ulcer (LLU), wounds caused by peripheral arterial occlusive disease (PAOD), and diabetic foot ulcer (DFU).
The causes of impaired wound healing are often multifactorial. 9 Local and systemic factors can contribute to the appearance of a wound and make it chronic. 10 , 11 Local factors (directly in the wound area) are a lack of oxygen supply to the skin (disturbance of blood circulation) and wound infections. Systemic (concerning the organism) factors are among others overweight, smoking, malnutrition, impaired mobility, diabetes, and sex. 10 , 11 , 12 , 13 Gender‐specific hormones have a special effect on wound healing. For example, oestrogens have a positive and testosterone rather a negative influence on wound healing. 14 , 15 , 16 Diabetes is highly associated with chronic wounds and impairs wound healing at all phases. 17 , 18 It interferes with the restoration of the vascular system and the regeneration of new tissue. 17 Insufficient nutrition is also associated with chronic wounds. The need for energy and nutrients is essential for the formation of new tissue. 19 Renner, Garibaldi 20 discovered that people with LLU are often obese but frequently malnourished. Significantly higher vitamin D deficiency is explained by reduced mobility. 20 Mobility is another factor associated with chronic wounds, particularly PU. 21 Multiple studies have classified immobility as one of the most common risk factors for geriatric syndromes such as pressure injuries, falls, and urinary incontinence. 22 , 23 Persons who are few physically active have a 1.5 to 2.3 times higher risk of a non‐healing wound. 24 Limited mobility can be the cause 24 or consequence 1 of chronic wounds. Furthermore, patients with cardiovascular and/or neurological diseases are more susceptible to impaired wound healing. 11 , 25
Meaningful data regarding the prevalence of chronic wounds in long‐term care are currently available to a limited extent only. Rondas, Schols 6 found a prevalence of 4.2% in 21 Dutch nursing homes. A study carried out in France reported a prevalence of 8.3%. 26
In Germany, 24% (818.000) of all care‐dependent people live in nursing homes. The total number has increased by 4.5% compared to 2015. 27 For this population, there is no current information available on prevalence and risk factors. Although there are some data available on prevalence from the German Medical Advisory Service of the National Association of Statutory Health Insurance Funds (“MDK”), 28 these data are collected for quality assurance purpose only. However, these data do not comprise any information about the distribution of relevant risk factors in German nursing homes.
Therefore, the aim of this study was to determine the prevalence and risk factors of chronic wounds in German nursing homes.
2. MATERIALS AND METHODS
A secondary analysis of the data from seven consecutive annual cross‐sectional studies in German nursing homes was carried out. Residents who were ≥60 years old were included. These originally individual studies were conducted from 2012 to 2018. The annual prevalence studies, which focus on different nursing problems, have been conducted since 2001. From 2012 onwards, the topic of chronic wounds and their different types was included in the survey. Nursing homes throughout Germany were invited to participate in the surveys in the respective years. If an institution decided to participate, it received all necessary material (information sheets, training material, and questionnaires) and a guide, in which all variables were defined and explained. On the day of the survey, nurses trained by a site coordinator performed a physical examination of residents after the participant or a proxy provided informed consent. All residents who were present in the participating nursing homes on the day of the survey were potentially eligible for study participation; patients 18 years or younger were excluded from participation. Trained nursing staff completed the questionnaire. Data collection was organised and carried out by the institutions themselves. Since higher prevalence of certain nursing problems (e.g. PU) is generally considered to be a lack of nursing quality, the survey was conducted anonymously. This was intended to counteract possible distortions caused by under‐reporting. Study procedures were reviewed and approved by the Ethical Medical Committee of Berlin (consent no: Eth837‐262/00).
Chronic wounds were defined as all wounds “… which do not show any healing tendencies within 4 ‐ 12 weeks after wound formation under professional therapy”. 7 Wounds that largely meet the above criteria are LLUs, PU, wounds caused by PAOD, and DFU. All other chronic wounds were categorised under “others”. Pressure ulcer was defined, following the European Pressure Ulcer Advisory Panel (EPUAP) definition, as “… localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear”. 29 Two nurses should carry out the assessment of the PU. This procedure reduces the risk of incorrect assessments. The socio‐demographic data comprised age, sex, weight, height, region, and sponsorship of the nursing home. Regions were divided into metropolitan (>100.000 residents), urban (20.000‐100.000 residents), and rural (<20.000 residents). The Body‐Mass‐Index (BMI) was calculated from height and weight and used for the variables obese (BMI > 30) and poor nutrition (BMI < 20). The Care Dependency Scale (CDS) item mobility was used to calculate the variable limited mobility. Mobile residents were categorised in three groups of people, who were partially dependent, almost independent, and completely independent. Residents with limited mobility were those who were completely or almost dependent. The main diagnosis (diabetes mellitus, heart/vascular disease), urinary incontinence, and stool incontinence were recorded.
Data analysis was conducted using the statistics programmes SPSS 24. The Descriptive evaluation was carried out in absolute and relative frequencies. Mean values (mean) and standard deviations (SD) were calculated for metric data. Statistically significant differences were presented using Chi‐square according to Pearson. For all statistical tests, an α = 0.05 two‐sided was considered to be statistically significant. The Wilson method was used to calculate the 95% confidence interval (CI). 30 , 31
For the multivariate analysis of the data, we used the Classification and Regression Trees modelling procedure (CRT). The CRT algorithm determines for each node the specific variable from the total of all included independent variables with the strongest difference regarding the prevalence of the outcome variable, which is in our study the prevalence of chronic wounds. The following nodes must be statistically significantly better than the node before.
This calculation method can be used to describe possible risk groups.
3. RESULTS
3.1. Prevalence of chronic wounds
Between 2012 and 2018 a total of 7662 residents were included in the study. The mean age was 85 years; women were on average 5 years older than men (86.4 years vs 80.9 years). 75% of the participating residents were female. 25% of the residents were suffering from diabetes.
The prevalence of chronic wounds was 7.8% (Table 1). The most common type was PU (4.0%).
TABLE 1.
Frequency of chronic wounds and their various types
| n (%; CI) | |
|---|---|
| Chronic wounds | 588 (7.8%; 7.2% to 8.4%) |
| PU | 303 (4.0%; 3.5% to 4.4%) |
| LLU | 71 (0.9%; 0.7% to 1.2%) |
| DFU | 45 (0.6%; 0.4% to 0.8%) |
| PAOD | 74 (1.0%; 0.8% to 1.2%) |
| Other | 129 (1.7%; 1.4% to 2.0%) |
Abbreviations: DFU, diabetic foot ulcer; LLU, lower leg ulcer; PAOD, peripheral arterial occlusive disease; PU, pressure ulcer.
3.2. Bivariate analysis on influencing factors of chronic wounds
Bivariate associations of factors influencing the occurrence of chronic wounds are shown in Table 2. Significant differences were found with regard to poor nutrition (7.2% vs 10.8%), urinary incontinence (4.9% vs 8.8%), stool incontinence (5.7% vs 11.1%), diabetes mellitus (6.6% vs 11.6%), and limited mobility (5.0% vs 12.3%).
TABLE 2.
Influencing factors of chronic wounds
| Chronic Wounds n (%; CI) | (Chi2 to Pearson) | ||
|---|---|---|---|
| Sponsorship | Public | 444 (7.6%; 6.9% to 8.3%) | P = 0.171 |
| Private | 144 (8.6%; 7.3% to 10.0%) | ||
| Region | Metropolitan | 143 (7.2%; 6.2% to 8.5%) | P = 0.416 |
| Urban | 197 (7.7%; 6.7% to 8.7%) | ||
| Rural | 248 (8.2%; 7.3% to 9.3%) | ||
| Sex | Female | 413 (7.4%; 6.8% to 8.2%) | P = 0.041 |
| Male | 165 (8.9%; 7.7% to 10.3%) | ||
| Poor nutrition (BMI < 20) | No | 472 (7.2%; 6.6% to 7.9%) | P = 0.000 |
| Yes | 93 (10.8%; 8.9% to 13.0%) | ||
| Obese (BMI > 30) | No | 465 (7.6%; 7.0% to 8.3%) | P = 0.900 |
| Yes | 100 (7.7%; 6.4% to 9.3%) | ||
| Urinary incontinence | No | 113 (4.9%; 4.1% to 5.9%) | P = 0.000 |
| Yes | 435 (8.8%; 8.1% to 9.7%) | ||
| Stool incontinence | No | 269 (5.7%; 5.1% to 6.4%) | P = 0.000 |
| Yes | 304 (11.1%; 10.0% to 12.3%) | ||
| Diabetes mellitus | No | 375 (6.6%; 5.9% to 7.2%) | P = 0.000 |
| Yes | 213 (11.6%; 10.2% to 13.2%) | ||
| Limited mobility | No | 232 (5.0%; 4.4% to 5.7%) | P = 0.000 |
| Yes | 350 (12.3%; 11.1% to 13.5%) | ||
| Heart/vascular disease | No | 65 (6.4%; 5.1% to 8.1%) | P = 0.045 |
| Yes | 181 (8.5%; 7.4% to 9.8%) | ||
3.3. Multivariate analysis regarding chronic wounds
Figure 1 shows the relationship between the independent variables and the dependent variable “chronic wound” and describes different risk groups. The strongest predictor in this analysis was limited mobility followed by diabetes mellitus.
FIGURE 1.
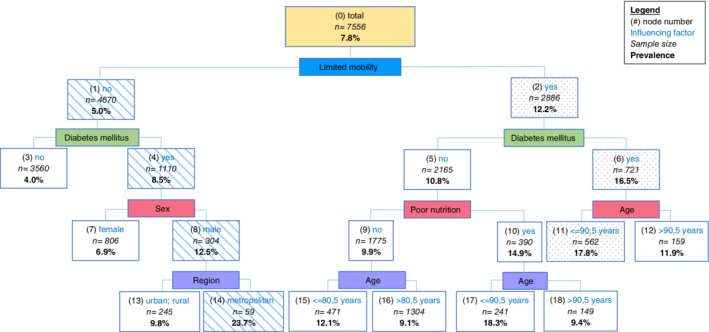
Multivariate analysis on influencing factors of chronic wounds and possible risk groups
In the group of residents with limited mobility, diabetics, and aged under 90.5 years (nodes 2, 6, 11 ➔ speckled) 17.8% had a chronic wound. 23.7% of all residents who were not restricted in their mobility, had diabetes, were male, and lived in a metropolitan region (nodes 1, 4, 8, 14 ➔ striped) had a chronic wound.
4. DISCUSSION
The present study investigated the prevalence and risk factors of chronic wounds in nursing homes in Germany. 7.8% of all residents had at least one chronic wound. Similar results were also found in other studies.
The proportion of men affected by chronic wounds was to some extent higher than that of women, 9.0% males vs 7.5% females. However, as the minimum age of the population studied was 60 years, these effects 15 were not relevant in this study. Moreover, male residents were twice as often affected by DFU than female residents. The male gender was confirmed as a risk factor in the meta‐analyses of Zhang, Lu 32 and Huang, Li. 33 In the study by Engberg, Kirketerp‐Moller, 34 men also had a significantly higher risk of DFU. Different psychological and physiological states and anatomical structures, health behaviour, environmental experiences, reactions to stress events, and differences in risk behaviour can cause these differences. 35 , 36
More than half of all chronic wounds found in this study were PU. In the study by Rondas, Schols, 6 which was also conducted in nursing homes, PU was found to be the most common (46%) chronic wound. Furthermore, studies in other settings also resulted in PU as one of the most frequent chronic wounds. 37 , 38
The influencing factors highlighted in other studies 10 , 11 , 12 , 13 , 17 , 18 were also found to be significant in the present study. Bivariate analysis showed that chronic wounds were highly associated with poor nutrition, urinary incontinence, stool incontinence, diabetes mellitus, and limited mobility.
According to multivariate analysis, the strongest predictors for chronic wounds were limited mobility and diabetes mellitus. Residents with limited mobility and diabetes were about twice as often affected by chronic wounds compared to residents with diabetes alone. Special focus should be placed on these groups of people and the nursing staff should be specially trained on these phenomena.
The highest prevalence of chronic wounds was in residents who were not restricted in their mobility, had diabetes, were male, and lived in a metropolitan region. It is remarkable that the highest prevalence of diabetics without mobility limitations was more than twice as high among men living in a large city compared to male diabetics without mobility limitations living in a rural area. These findings raise the question, if living in a rather anonymous environment might favour the occurrence of diabetes. Furthermore, the group with the highest prevalence of chronic wounds (residents who were not restricted in their mobility) is also the group with the lowest n by far, compared to all other nodes on this level. Even though only one (diabetes mellitus) of the highly associated factors from the bivariate analysis is true for this group, it reveals to be the one with the highest prevalence. Due to the small n, this group does not occur in bivariate analysis indicating the necessity to run a multivariate analysis in order to reveal the group's importance.
Our sample of 7405 residents drawn from nursing homes throughout Germany reflects a robust variety of settings within the German republic. Selection bias may have occurred due to the voluntary participation for institutions. However, in the survey by the Medical Advisory Service of the National Association of Statutory Health Insurance Funds, a prevalence of 7.3% was found in German nursing homes, 28 which is comparable to our study result. In addition, the cross‐sectional study design did not allow us to reach conclusions about causal relationships between chronic wounds and gender‐related differences. As is often the case in secondary data analyses, not all relevant risk factors, such as specific chronic conditions that compromise the immune system or lifestyle habits, (i.e. smoking) could be included in the model.
This study identified the prevalence and risk factors of chronic wounds in nursing home residents. Further research is needed to identify causal factors of the gender difference in the prevalence of chronic wounds. This may have an impact on the choice of prophylactic and therapeutic measures.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this paper.
ACKNOWLEDGEMENTS
The authors would like to express their gratefulness to the participating home care services who supported this study. Open access funding enabled and organized by Projekt DEAL. [Correction added on 24 December 2020, after first online publication: Projekt Deal funding statement has been added.]
Raeder K, Jachan DE, Müller‐Werdan U, Lahmann NA. Prevalence and risk factors of chronic wounds in nursing homes in Germany. Int Wound J. 2020;17:1128–1134. 10.1111/iwj.13486
Funding information This study was supported by the Department of Geriatric Medicine at the Charité‐Universitätsmedizin Berlin and financed by the Federal Ministry of Education and Research (BMBF), Grant/Award Number: 01GL1717
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Olsson M, Jarbrink K, Divakar U, et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 2019;27(1):114‐125. [DOI] [PubMed] [Google Scholar]
- 2. Kapp S, Miller C, Santamaria N. The quality of life of people who have chronic wounds and who self‐treat. J Clin Nurs. 2018;27(1‐2):182‐192. [DOI] [PubMed] [Google Scholar]
- 3. Lazarus GS, Cooper DM, Knighton DR, Percoraro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2(3):165‐170. [DOI] [PubMed] [Google Scholar]
- 4. Ennis WJ, Meneses P. Wound healing at the local level: the stunned wound. Ostomy/Wound Manage. 2000;46(1A Suppl):39S‐48S. quiz 9S‐50S. [PubMed] [Google Scholar]
- 5. Paul J. Characteristics of chronic wounds that itch. Adv Skin Wound Care. 2013;26(7):320‐332. quiz 33‐34. [DOI] [PubMed] [Google Scholar]
- 6. Rondas AA, Schols JM, Stobberingh EE, Halfens RJ. Prevalence of chronic wounds and structural quality indicators of chronic wound care in Dutch nursing homes. Int Wound J. 2013;12(6):630‐635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deutsches Netzwerk für Qualitätsentwicklung in der Pflege (DNQP) . Expertenstandard Pflege von Menschen mit chronischen Wunden. 1. Aktualiosierung 2015. Osnabrück: Deutsches Netzwerk für Qualitätsentwicklung in der Pflege (DNQP; 2015. [Google Scholar]
- 8. Deutsche Gesellschaft für Wundheilung und Wundbehandlung e.V . Lokaltherapie chronischer Wunden bei Patienten mit den Risiken periphere arterielle Verschlusskrankheit, Diabetes mellitus, chronische venöse Insuffizienz; AWMF‐Leitlinien‐Register Nr. 091/001, Klasse: S3.: AWMF online; 2012.
- 9. Armstrong DG, Meyr AJ. Risk factors for impaired wound healing and wound complications. In: Collins KA, ed. UpToDate. Waltham, MA: UpToDate Inc.; 2019. [Google Scholar]
- 10. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morton LM, Phillips TJ. Wound healing and treating wounds: differential diagnosis and evaluation of chronic wounds. J Am Acad Dermatol. 2016;74(4):589‐605. quiz 606. [DOI] [PubMed] [Google Scholar]
- 12. Panfil E‐M, Schröder G. Pflege von Menschen mit chronischen Wunden. Lehrbuch für Pflegende und Wundexperten. Pflegepraxis. 2., korrigierte und erg. Aufl. ed. Bern: Huber; 2010:607 S. [Google Scholar]
- 13. Agale S. Chronic leg ulcers: epidemiology, aetiopathogenesis, and management. Ulcers. 2013;2013:1‐9. [Google Scholar]
- 14. Ashcroft GS, Mills SJ. Androgen receptor‐mediated inhibition of cutaneous wound healing. J Clin Invest. 2002;110(5):615‐624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cooper RL, Segal RA, Diegelmann RF, Reynolds AM. Modeling the effects of systemic mediators on the inflammatory phase of wound healing. J Theor Biol. 2015;367:86‐99. [DOI] [PubMed] [Google Scholar]
- 16. Gilliver SC, Wu F, Ashcroft GS. Regulatory roles of androgens in cutaneous wound healing. Thromb Haemost. 2003;90(6):978‐985. [DOI] [PubMed] [Google Scholar]
- 17. Okonkwo UA, DiPietro LA. Diabetes and wound angiogenesis. Int J Mol Sci. 2017;18(7):1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Salazar JJ, Ennis WJ, Koh TJ. Diabetes medications: impact on inflammation and wound healing. J Diabetes Complications. 2016;30(4):746‐752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Haughey L, Barbul A. Nutrition and lower extremity ulcers: causality and/or treatment. Int J Low Extrem Wounds. 2017;16(4):238‐243. [DOI] [PubMed] [Google Scholar]
- 20. Renner R, Garibaldi MDS, Benson S, Ronicke M, Erfurt‐Berge C. Nutrition status in patients with wounds: a cross‐sectional analysis of 50 patients with chronic leg ulcers or acute wounds. Eur J Dermatol. 2019;29(6):619‐626. [DOI] [PubMed] [Google Scholar]
- 21. Lahmann NA, Tannen A, Kuntz S, et al. Mobility is the key! Trends and associations of common care problems in German long‐term care facilities from 2008 to 2012. Int J Nurs Stud. 2015;52(1):167‐174. [DOI] [PubMed] [Google Scholar]
- 22. Jachan DE, Muller‐Werdan U, Lahmann NA. Impaired mobility and urinary incontinence in nursing home residents: a multicenter study. J Wound Ostomy Continence Nurs. 2019;46(6):524‐529. [DOI] [PubMed] [Google Scholar]
- 23. Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780‐791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vieira CPB, Araujo TME. Prevalence and factors associated with chronic wounds in older adults in primary care. Rev Esc Enferm USP. 2018;52:e03415. [DOI] [PubMed] [Google Scholar]
- 25. Martinez‐Zapata MJ, Marti‐Carvajal AJ, Sola I, et al. Autologous platelet‐rich plasma for treating chronic wounds. Cochrane Database Syst Rev. 2016;(5):CD00689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Caron‐Mazet J, Roth B, Guillaume JC. Prevalence and management of chronic wounds in 14 geriatric institutions of the haut‐Rhin. Ann Dermatol Venereol. 2007;134(8–9):645‐651. [DOI] [PubMed] [Google Scholar]
- 27. Statistisches Bundesamt (Destatis) . Pflegestatistik 2017. Pflege im Rahmen der Pflegeversicherung. Deutschlandergebnisse. Statistisches Bundesamt (Destatis); 2018.
- 28. Medizinischer Dienst des Spitzenverbandes Bund der Krankenkassen e.V . (MDS) (Hrsg.). 3. Bericht des MDS nach § 114a Abs. 6 SGB XI. Qualität in der ambulanten und stationären Pflege. Essen; 2012.
- 29. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance . Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Osborn Park, Australia: Cambridge Media; 2014. [Google Scholar]
- 30. Newcombe RG, Altman DG. Proportions and their differences. In: Altman D, Machin D, Bryant T, Gardner M, eds. Statistics with Confidence: Confidence Intervals and Statistical Guidelines. London: BMJ Books; 2000. [Google Scholar]
- 31. Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22(158):209‐2012. [Google Scholar]
- 32. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta‐analysis (dagger). Ann Med. 2017;49(2):106‐116. [DOI] [PubMed] [Google Scholar]
- 33. Huang ZH, Li SQ, Kou Y, Huang L, Yu T, Hu A. Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: a meta‐analysis. Int Wound J. 2019;16(6):1373‐1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Engberg S, Kirketerp‐Moller K, Ullits Andersen H, Rasmussen A. Incidence and predictors of recurrent and other new diabetic foot ulcers: a retrospective cohort study. Diabet Med. 2019;36(11):1417‐1423. [DOI] [PubMed] [Google Scholar]
- 35. Hamberg K. Gender bias in medicine. Womens Health. 2008;4(3):237‐243. [DOI] [PubMed] [Google Scholar]
- 36. Wattenberg I, Lätzsch R, Hornberg C. Gesundheit, Krankheit und Geschlecht: ein gesundheitswissenschaftlicher Zugang zu Einflussfaktoren und Versorgungssystem. In: Kortendiek B, Riegraf B, Sabisch K, eds. Handbuch Interdisziplinäre Geschlechterforschung. Wiesbaden: Springer Fachmedien Wiesbaden; 2019:1193‐1202. [Google Scholar]
- 37. Lichterfeld‐Kottner A, Lahmann N, Blume‐Peytavi U, Mueller‐Werdan U, Kottner J. Dry skin in home care: a representative prevalence study. J Tissue Viability. 2018;27:226‐231. [DOI] [PubMed] [Google Scholar]
- 38. Raeder K, Strube‐Lahmann S, Muller‐Werdan U, Kottner J, Lahmann NA, Suhr R. Prevalence and influencing factors of chronic wounds among clients of home care services in Germany. Z Evid Fortbild Qual Gesundhwes. 2019;140:14‐21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


