Abstract
In the past decades, numerous surgical techniques and conservative treatments for pilonidal sinus disease (PSD) had been discussed and published. There is still no consensus yet of the best techniques because of high recurrence rates and prolonged wound healing. In the case of complicated discharging sinus or recurrent PSD resistant to treatment with antibiotics, we recommend radical excision followed by a regional flap, which can obliterate the dead space with well‐vascularised tissue. In this article, we presented the technique of snug suture fixation between the dermis and periosteum using a superior gluteal artery perforator (SGAP) flap. The study demonstrates a few key concepts on the prevention of PSD recurrence, an off‐midline, well‐perfused flap that allows flattened natal cleft and obliteration of gluteal cleft and eventually showed good aesthetic results. We aim to demonstrate a reliable surgical technique for wound closure of recurrent pilonidal sinus after radical excision followed by reconstruction with an SGAP flap. The history, surgery, and images are described, and the literature is reviewed. The pitfalls of disease recurrence will be discussed in this literature. Keys to successful treatment will be elaborated. An 18‐year‐old female with recurrent pilonidal sinus disease over right medial gluteal region presented with sacral pain and infection. She developed progressive swelling and burst of abscess from several sinus tracts and did not respond to the treatment with antibiotics alone. After radical excision of the entire pilonidal sinus and adjacent fibrotic tissue, a deep and large defect was measured. A superior gluteal perforator flap was designed based on three perforators from the superior gluteal artery. A medial 3 cm of the SGAP flap was de‐epithelised to provide soft tissue bulk to obliterate the deep cavity. Strong sutures were applied to secure the flap to the periosteum. There was no recurrence at 3 years of follow up. The patient stood the operation well and had prompt recovery.
1. INTRODUCTION
Pilonidal is from the Latin words (Latin: pilus = hair and nidus = nest), and pilonidal sinus disease indicates a disease consisting of hair‐containing sinus in the sacrococcygeal area. This is an old disease, first described by Hodges in 1880.1 Pilonidal sinus disease mainly affects young and active people of working age. It occurs in approximately 0.7% of the population, with peak age of incidence at 16–25 years, exceptionally before puberty or after 60 years. 2, 3 The predisposing factors include hairy body, thick skin, overweight, a deep gluteal cleft, poor hygiene, long seated hours, repeated chafing, and family history of this disease.4 The physiopathology of PSD is much debated, based on two principle theories, the “congenital” and “acquired” theories. Congenital theory suggests that a pit presents at birth resulting from the absence of coalescence of the primitive ectoderm. Acquired theory was proposed in the middle of the 20th century based on the primodial role of the hair follicle, resulting from repeated microtraumatism, rubbing, and/or crushing. Friction in‐between the gluteal cleft causes ingrowth of hair via the enlarged pits.5 Sex hormones increase the hair growth, which somehow explains the post‐puberty onset of PSD.6
The goals of the treatments are simple: cure infection, obtain healing as rapidly as possible, and prevent recurrence. Most surgeons will come across this disease in their career because of its high prevalence, but there is still no consensus on the “ideal treatment”. Debates over the best treatment have been published throughout the years. A Cochrane review on randomised controlled trials (RCTs) evaluating open versus closed surgical treatment for pilonidal sinus concluded that there was no clear benefit between surgical management by primary closure or open healing by secondary intention. However, recurrence rates of 1.4% (3/209) for off‐midline closure compared with 10.3% (21/204) after midline closure indicate a clear advantage for off‐midline procedures when considering recurrence rates. 7 The off‐midline method should be the standard treatment of infected PSD if primary closure is desired. Different surgical techniques were used and compared. The common surgical managements are primary closure, lay open, local flaps, and perforator flap. These different procedures were compared, and despite the increasing volume of data on the treatment experience of PSD, optimal treatment has yet to be established as there is no 100% cure rate reported.8 Knowledge about perforator flap in the reconstruction of pilonidal sinus is limited. Therefore, we aim to demonstrate a reliable surgical technique for wound closure of recurrent pilonidal sinus after radical excision using a superior gluteal artery perforator (SGAP) flap.
2. CASE PRESENTATION
An 18‐year‐old female with recurrent pilonidal sinus disease over right medial gluteal region presented with sacral pain and repeated infection. Soft‐tissue sonography was performed and was compatible with residual sinus in the subcutaneous region of buttock. (Figure 1) She developed progressive swelling and burst of abscess from several sinus tracts despites treatment courses under antibiotics. We decided to perform radical excision and primary reconstruction with a regional flap for her recurrent pilonidal disease over the right medial gluteal region (Figure 2).
Figure 1.
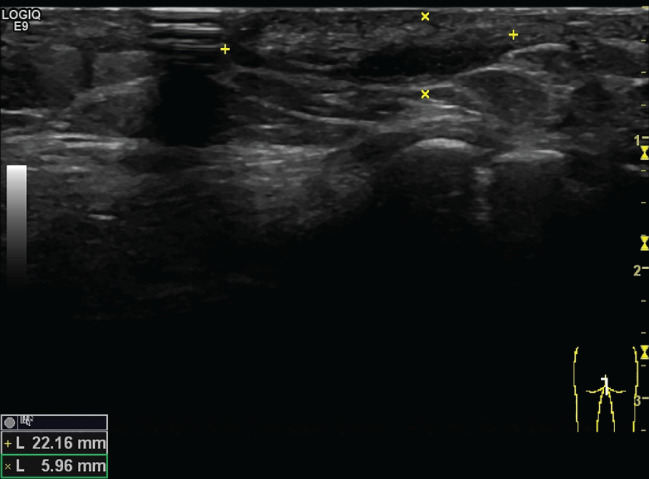
Soft‐tissue sonography showing residual sinus in the subcutaneous region of the buttock [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.

Radical excision of the pilonidal sinus and deep defect over the middle gluteal region [Colour figure can be viewed at wileyonlinelibrary.com]
3. SURGICAL TECHNIQUE
The patient was placed in the prone position, and the gluteal cheeks and sacrococcygeal area were shaved, cleaned with povidone iodine, and draped in a sterile manner. The right SGAPs were identified by Doppler. A fasciocutaneous transpositional flap was designed from the right buttock in a V‐Y fashion. It was based on three perforators from the superior gluteal artery. The skin incision was made accordingly, and the perforators were identified with careful dissection. (Figure 3) The flap was raised and was mobilised. A medial 3 cm of the flap was de‐epithelised to provide soft tissue filling into the deep cavity following removal of the lesion. (Figure 4) Using 3–0 and 2–0 prolene sutures the flap was mobilized and dermis was sucured to periosteum to a proper position. (Figure 5) The remaining defects at right gluteal area was closed with advancement of the tissue above and below the flap. The wounds were closed with 3–O Vicryl and PDS, then 4–O nylon sutures. (Figure 6) Soft bulky dressing was applied. The patient stood the operation well and has prompt recovery without recurrence at three years of follow up.
Figure 3.

A fasciocutaneous rotation flap was designed from the right buttock in a V‐Y fashion. The skin incision was made accordingly, and the perforators were identified with careful dissection [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 4.
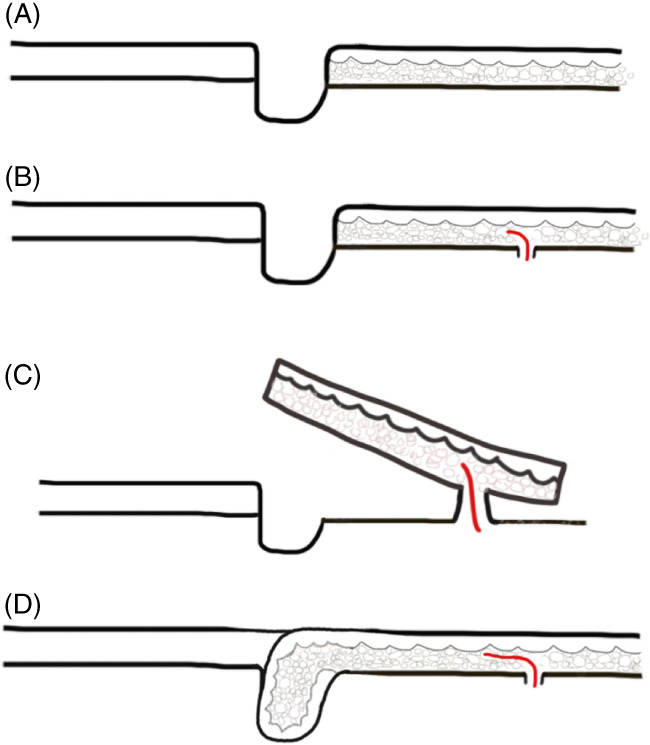
A, Deep cavity after radicle excision. B, Perforator was identified with Doppler. C, Fasciocutaneous flap was elevated. D, De‐epithelised to form soft tissue filling into the cavity [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 5.
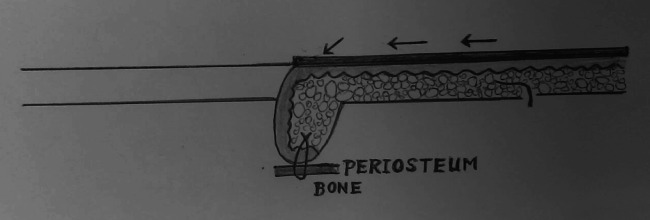
Snug suture fixation was applied using 3–0 and 2–0 PROLENE. The dead space is obliterated. Secure fixation of the dermis to the periosteum prevents disease recurrence
Figure 6.

The medial 3 cm skin was de‐epithelised. The remaining defects in the right gluteal area were closed with advancement of the tissue above and below the flap [Colour figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
We propose a few key points to prevent the pitfalls. The first key to treat complicated PSD is adequate excision. Surgeons must have the confidence to perform radical excision with margins of assurance in order to excise involved and disease‐prone tissue without the fear of creating a defect that cannot be closed. Secondly, midline closure should be avoided. Shearing and friction movements in between buttocks can lead to wound dehiscence and enhance the disease recurrence, caused by repeated penetration of the hair shafts.
In comparison with the random flap, the perforator flap is more reliable in vascularity; it can close a larger and deeper defect and has more freedom in transposition. In addition, with careful preoperative planning, a propeller flap can also be designed. Finally, an SGAP flap can be an ideal choice for reconstruction of deep gluteal defects. It provides an off‐midline, durable coverage that completely obliterates the dead space and elevates the natal cleft for such a complicated pilonidal case, with good aesthetic results.
5. SUMMARY
The superior gluteal artery flap is a good option for the management of recurrent pilonidal sinus. The advantages are: (1) multiple large perforators can always be found to provide good blood supply for this flap, which is very reliable in terms of tissue perfusion; (2) it does not sacrifice muscle; (3) the suture line is not in the midline; (4) its de‐epithelised part can obliterate the deep cavity after debridement; (5) the de‐epithelized part is resistant to pressure, and there is no residual space inside the wound, and therefore, no more recurrence is found; and (6) the donor site can always be closed primarily. Point number five has never been mention in the literature. The de‐epithelised part is equivalent to an augmented padding that is more resistant to pressure when the patient is sitting or sleeping. Secure fixation of the dermis to the periosteum is important for the prevention of recurrence (Figure 7).
Figure 7.

Two weeks after the surgery, patient had stiches removed [Colour figure can be viewed at wileyonlinelibrary.com]
Liao L‐Y, Li T‐S, Chen HC. Idea and innovation: Secure fixation between dermis and periosteum using perforator flap to prevent recurrence of pilonidal sinus disease. Int Wound J. 2019;16:862–865. 10.1111/iwj.12981
REFERENCES
- 1. Corman ML. Classic articles in colonic and rectal surgery, pilonidal sinus. Dis Colon Rectum. 1981;24:324‐326. [PubMed] [Google Scholar]
- 2. Shabbir J, Chaudhary BN, Britton DC. Management of sacrococcygeal pilonidal sinus disease: a snapshot of current practice. Int J Colorectal Dis. 2011;26:1619‐1620. [DOI] [PubMed] [Google Scholar]
- 3. Doll D, Friederichs J, Dettmann H, Boulesteix A‐L, Duesel W, Petersen S. Time and rate of sinus formation in pilonidal sinus disease. Int J Colorectal Dis. 2008;23:359‐364. [DOI] [PubMed] [Google Scholar]
- 4. Doll D, Matevossian E, Wietelmann K, Evers T, Kriner M, Petersen S. Family history of pilonidal sinus predisposes to earlier onset of disease and a 50% long‐term recurrence rate. Dis Colon Rectum. 2009;52:1610‐1615. [DOI] [PubMed] [Google Scholar]
- 5. de Parades V, Bouchard D, Janier M, Berger A. Pilonidal sinus disease. J Visc Surg. 2013;150:237‐247. [DOI] [PubMed] [Google Scholar]
- 6. von Laffert M, Stadie V, Ulrich J, Marsch WC, Wohlrab J. Morphology of pilonidal sinus disease: some evidence of its being a unilocalized type of hidradenitis suppurativa. Dermatology. 2011;223:349‐355. [DOI] [PubMed] [Google Scholar]
- 7. Al‐Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010;20:CD006213. 10.1002/14651858.CD006213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Saylam B, Balli DN, Duzgun AP, Ozer MV, Coskun F. Which surgical procedure offers the best treatment for pilonidal disease? Langenbecks Arch Surg. 2011;396:651‐658. [DOI] [PubMed] [Google Scholar]


