Abstract
A 44-year-old previously well woman presented with features of respiratory sepsis including a productive cough and fevers, with a recent preceding influenza-like illness. She was diagnosed with community-acquired pneumonia on chest radiograph, influenza infection via nasopharyngeal swab and Streptococcus pneumoniae bloodstream infection with associated purulent pericarditis. She was managed with pericardial drainage and concurrent treatment with antibiotics and made an excellent recovery. This case highlights the complications of both influenza and S. pneumoniae infections, and the importance of prevention via vaccination.
Keywords: infectious diseases, pneumonia (infectious disease), pneumonia (respiratory medicine), pericardial disease, immunological products and vaccines
Background
Seasonal influenza is an acute respiratory infection caused by the influenza virus which has four types—A, B, C and D. Human influenza A and B viruses cause seasonal epidemics. The influenza vaccine is updated seasonally/yearly because the virus changes due to antigenic drift and shift, and the vaccine is recommended to those who are at higher risk of complications. The Centres for Disease Control and Prevention (CDC) estimated the burden of influenza illness in the USA during the 2019–2020 season as ‘moderate’, with 38 million people infected with influenza, 18 million visits to healthcare providers, 400 000 hospitalisations for influenza and 22 000 influenza deaths.1 For the 2019/2020 influenza season in Ireland, greater than 11 000 cases of influenza infections, 152 influenza-related ICU (Intensive Care Unit) admissions and 110 influenza-related deaths were reported.2 The National Seasonal Influenza Vaccination Programme has been launched for 2020/2021 in both Ireland and in the UK, and recent studies have demonstrated the effectiveness of the influenza vaccine against influenza A.3 In Ireland and the UK, the influenza vaccine is recommended to those who are at high risk of complications, that is, those over the age of 65 years, those with chronic lung/cardiac/liver/renal disease, and pregnant women. The UK recommends the influenza vaccine for all children between the ages of 2 and 12 (year seven students), and for children outside this age range, that is, from 6 months to 2 years, and from age 12 to 17 who have long-term medical conditions. A new recommendation this year in Ireland includes all children between the ages of 2 and 12. Bacterial coinfection and secondary infection can complicate influenza, leading to increased morbidity and mortality.
Streptococcus pneumoniae is the leading bacterial cause of community-acquired pneumonia, and is also causative in otitis media, meningitis and bloodstream infections. It is the most common bacteria found in viral secondary bacterial infections.4 The incidence of invasive pneumococcal disease (IPD) has significantly reduced since the introduction of the pneumococcal vaccine. S. pneumoniae pericarditis is a rare but significant complication of IPD.
This case highlights the importance of two vaccine-preventable infections.
Case presentation
A 44-year-old woman presented to a tertiary hospital on 31 December 2019 with a 2-day history of fevers, chest pain, productive cough and a 2-week history of influenza-like symptoms. She had no significant medical history, she was not on any regular medications and had no history of immunosuppression. Initial investigations revealed a lymphopenia at 0.4×109/L (normal range 1.5–4.5×109/L) and C-reactive protein of 460 mg/L (normal range 0–5 mg/L). A chest radiograph revealed a right midzone infiltrate. She was empirically commenced on piperacillin-tazobactam, clarithromycin and oseltamivir pending microbiological investigations.
Investigations
A nasopharyngeal swab detected influenza A. Peripheral blood cultures, both aerobic and anaerobic bottles, grew S. pneumoniae with a penicillin MIC (minimum inhibitory concentration) of 0.012 confirming susceptibility. This blood culture isolate was referred to the Irish Meningitis and Sepsis Reference Lab, which identified as Streptococcus pneumoniae serotype 8.
A CT-thorax (figure 1) revealed extensive bilateral consolidation and an enhancing pericardium with a large pericardial effusion consistent with pericarditis.
Figure 1.
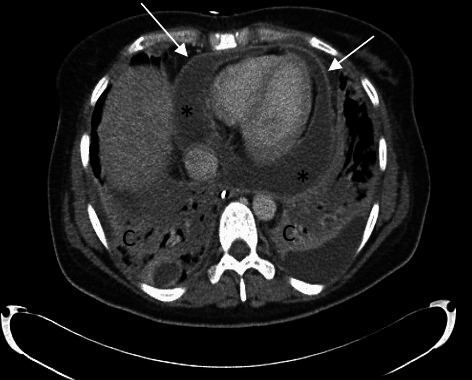
CTthorax: Extensive consolidation (c) in lower lung consistent with bilateral pneumonia. Enhancing pericardium (arrows) with large pericardial effusion (asterisk (*)) in keeping with pericarditis.
Treatment
Six days into admission, the patient became unstable; she was hypotensive and tachycardic, and an echocardiogram revealed a 3 cm circumferential pericardial effusion with right ventricular impairment. Her deterioration prompted transfer to a specialised cardiology and cardiothoracic centre for further management. Pericardiocentesis was performed, 300 mL of purulent fluid drained immediately and the pericardial drain remained in situ. The pericardial fluid had >20 white cell count/high power field, no organisms were seen on the Gram stain and there was no growth on bacterial culture. The pericardial fluid was also tested, as routine, for mycobacterium; acid-fast bacilli were not seen on microscopy and mycobacterium species was not isolated on culture. Molecular testing detected S. pneumoniae DNA and PBP2B (Penicillin-Binding-Protein) which infers penicillin susceptibility. Serial chest X-rays were performed and figure 2 captures satisfactory position of the pericardial drain and bilateral consolidation. Repeat imaging with a CT-thorax (figure 3) confirmed a large pericardial effusion with overlying left lower lobe consolidation, and it also demonstrated the tip of the pericardial drain located postero-inferior to the left ventricle.
Figure 2.
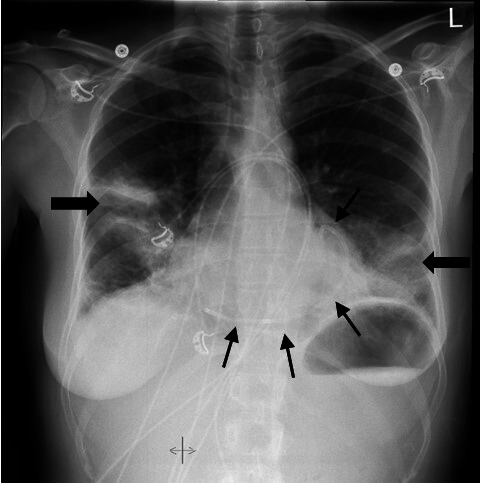
Chest X-ray: Persistent consolidation (block arrows) in the right midzone and left lower zone. Pericardial drain in place (thin arrows).
Figure 3.
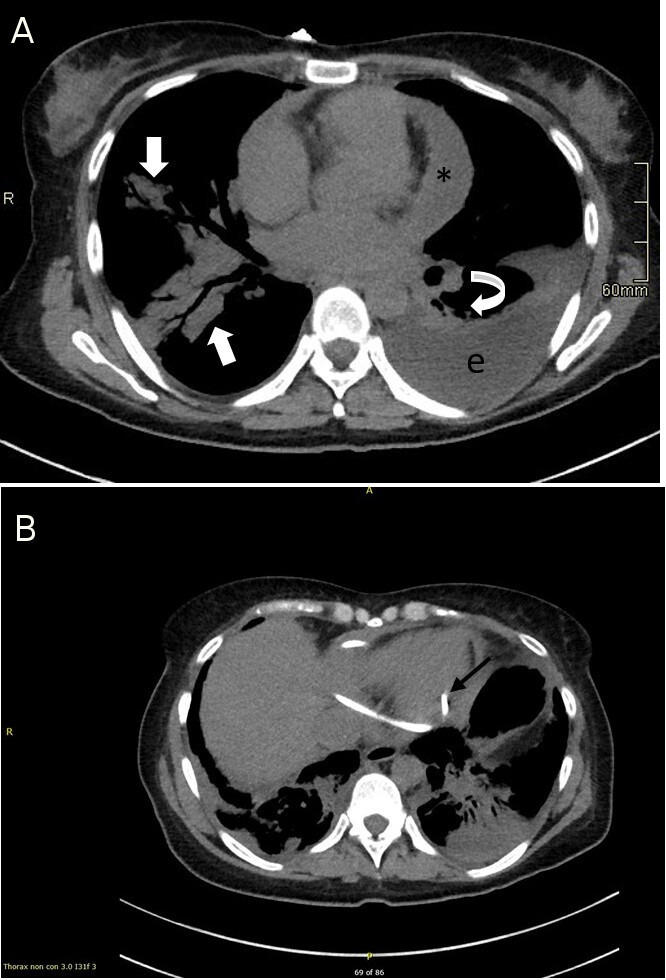
(A) CT of thorax: Large pericardial effusion (asterisk (*)). Large left-sided loculated pleural effusion (e) with overlying consolidation in the left lower lobe (curved block arrow). Small right-sided pleural effusion, with patchy peribronchial consolidation (block arrows) involving the right middle and lower lobes. (B) CT of thorax: Image demonstrates pericardial drain in situ with the tip (arrow) sited postero-inferior to the left ventricle.
Two weeks into admission, the cardiothoracic team performed a VATS (video-assisted thoracic surgery) procedure with pericardial washout and stripping. She was treated with intravenous ceftriaxone and had serial echocardiograms to monitor for pericardial fluid reaccumulation.
Outcome and follow-up
The patient improved, completed a 5-week course of ceftriaxone and was discharged home after a 6-week in-hospital stay. She required input from the multidisciplinary team for rehabilitation prior to discharge. The patient was counselled on the risk of developing constrictive pericarditis. She has been seen regularly in the cardiology outpatient department with serial echocardiograms.
Discussion
Bacterial pericarditis is rare and has a reported incidence of 1/18 000.5 Even with appropriate treatment, the mortality rate has been reported as up to 40% because of associated complications including sepsis, cardiac tamponade and constrictive pericarditis.5 Most often, the pericardium is infected by extension from the lung, that is, from pneumonia or empyema, but other causes include direct spread from a mediastinitis or via haematogenous spread.6
S. pneumoniae is the leading bacterial cause of community-acquired pneumonia and is also causative in otitis media, meningitis and bloodstream infections.
Since 1980, fewer than 20 cases of S. pneumoniae pericarditis have been described, 10 of which were in children.6 Mortality rates are reported as up to 30%.7
The case definition of IPD is an S. pneumoniae infection of the blood, cerebrospinal fluid or other normally sterile site.8 Risk factors include extremes of age, asplenia, HIV infection and chronic pulmonary/renal/cardiac/liver diseases,9 of which our patient had none. The incidence of IPD in Ireland in 2018 was 10.7 per 100 000, and 14% of the 510 cases (n=73) were reported as IPD-related deaths.8 European data report 6.2 cases of IPD per 100 000 in 2017.9
There are two pneumococcal vaccines in use in Ireland and the UK; the pneumococcal polysaccharide vaccine (PPV) and the pneumococcal conjugate vaccine (PCV).
In both Ireland and in the UK, the PCV-13 vaccine is recommended as part of the infant immunisation schedule to children under 2 years of age. In Ireland, the national uptake of the vaccine in 2017 was 91%,8 and there was a 70% decline in the IPD incidence in 2018 in the <2 age group compared with 2008 (n=20 vs n=52), reflecting the positive impact of the introduction of PCV-7 and PCV-13 in 2008 and 2010, respectively.8
The pneumococcal isolate in this case was S. pneumoniae serotype 8 which is included in the PPV-23 vaccine. In Ireland and the UK, the PPV-23 vaccine is recommended to people aged 65 years and older, and those >2 years with a risk of IPD including diabetes, chronic lung/liver/heart/kidney disease, asplenia and so on. The patient presented in the case report did not meet the criteria to receive the PPV-23 vaccine. The PPV-23 vaccine and the annual influenza vaccine should be recommended to this patient going forward.
We hope that this case report will promote awareness to medical professionals on the role of both the annual influenza and the 5-yearly PPV-23 vaccinations in at-risk patient cohorts.
Patient’s perspective.
Up to the point of my illness, I had experienced excellent physical health. I am a lifelong non-smoker and I have been proactive in looking after my general health and wellbeing, with good nutrition and daily exercise. I had, however, been suffering the effects of chronic stress for five years. I visited my GP and was being treated with medication for ongoing stress.
Becoming so ill from Influenza A and its subsequent complications was completely unforeseen for me. I had not requested a flu vaccine from my GP in advance of the 2019 flu season as I did not consider myself to be in the high-risk category. When I was admitted to the hospital on 31st of December, I would have been deemed immunocompetent, presumably, by my age and medical history, and treated accordingly. Within a few days, the severity of my condition became apparent, when I made no signs of recovery.
My medical management included a range of questions about my general health, specific questions relating to my levels of immunity, social history, and some pertaining to a potential history of sexually transmitted diseases. At the time I was confused at such questioning, but on reflection, I understand the importance of the inquiries.
Early in my hospital admission, I felt a sense of doom. I remember crying and begging the nurse to get help. Thankfully, I was heard and was admitted to ICU, where it was discovered that I had pericarditis. Shortly thereafter, I was transferred to a specialist hospital where I was treated successfully over a period of five weeks. My inpatient stay proved a challenging journey. I had never been sick in my life before. I was acutely aware of what was happening to and around me and I was frightened of the outcome.
On reflection, a key element to my recovery, apart from the medical professionalism and expertise, was the level of genuine patient-centred care that I was afforded. I felt that I could take ownership of my recovery with the support of the medical teams around me. Some days it was just the little things that got me through the day, a smile, a joke, a calm voice, in between the tests and procedures. These were the things that made me feel safe when so much was out of my control. Being seen, heard and included as an integral element in my own medical recovery, gave me a huge sense of purpose in the weeks spent in hospital and the months since I have been discharged. ‘Nothing about me without me’ has seen me combat my illness and go from strength to strength since. I am so very grateful for the entire team of medical professionals who cared for me.
Learning points.
Seasonal influenza infection is associated with secondary bacterial infection with Streptococcus pneumoniae which can cause significant morbidity and mortality, and has a notable impact on primary and tertiary care facilities.
Bacterial pericarditis secondary to S. pneumoniae infection is rare, and bacterial pericarditis carries a mortality rate of 40%.
Those in at-risk groups should be advised regarding both seasonal influenza vaccination and pneumococcal vaccination, as this case highlights severe complications from two vaccine-preventable infections.
Footnotes
Contributors: EH collected information and wrote the case report. RM advised on the presentation and reporting of the radiology. RW and RM contributed to revising the manuscript and provided final approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.CDC (Centers for Disease Control and Prevention) . Seasonal influenza burden index, surveillance report, 2020. Available: https://www.cdc.gov/flu/about/burden/2019-2020.html#:~:text=CDC%20estimates%20that%20the%20burden,flu%20deaths%20(Table%201) [Accessed 1 Oct 2020].
- 2.HPSC (Health Protection Surveillance Centre) . Influenza surveillance in Ireland. influenza surveillance report, 2020. Available: https://www.hpsc.ie/a-z/respiratory/influenza/seasonalinfluenza/surveillance/influenzasurveillancereports/previousinfluenzaseasonssurveillancereports/20192020season/Influenza_Surveillance_Report_Week_39.pdf
- 3.Kissling E, Pozo F, Buda S, et al. Effectiveness of influenza vaccine against influenza A in Europe in seasons of different A(H1N1)pdm09 and the same A(H3N2) vaccine components (2016-17 and 2017-18). Vaccine X 2019;3:100042. 10.1016/j.jvacx.2019.100042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol 2017;8:1041. 10.3389/fmicb.2017.01041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel H, Patel C, Soni M, et al. Acute primary pneumococcal purulent pericarditis with cardiac tamponade: a case report and literature review. Medicine 2015;94:e1709. 10.1097/MD.0000000000001709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koster N, Narmi A, Anand K. Bacterial pericarditis. Am J Med 2009;122:e1–2. 10.1016/j.amjmed.2008.11.012 [DOI] [PubMed] [Google Scholar]
- 7.Feinstein Y, Falup-Pecurariu O, Mitrică M, et al. Acute pericarditis caused by Streptococcus pneumoniae in young infants and children: three case reports and a literature review. Int J Infect Dis 2010;14:e175–8. 10.1016/j.ijid.2009.03.033 [DOI] [PubMed] [Google Scholar]
- 8.HPSC (Health Protection Surveillance Centre) . Annual epidemiological report of Streptococcus pneumoniae (invasive) in Ireland in 2018, 2020. Available: https://www.hpsc.ie/a-z/vaccinepreventable/pneumococcaldisease/publications/annualreportsoninvasivepneumococcaldisease/Streptococcus%20pneumoniae%20invasive%20in%20Ireland%202018.pdf
- 9.ECDC (European Centre for Disease Prevention and Control) . Invasive pneumococcal disease – annual epidemiological report for 2017, 2020. Available: https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2017-invasive-pneumococcal-disease.pdf


