Abstract
The aims of the study were to describe and analyse the temporal trend of the prevalence and incidence of venous leg ulcers (VLU) over the years 2010 to 2014, to determine healing times and temporal trends in the study period, and to evaluate related aspects such as the use of the Ankle‐Brachial Pressure Index (ABPI) in a primary care health centre. This was a retrospective study based on a time series (years 2010‐2014) of the prevalence and incidence of VLUs in people aged over 40 years in a primary care centre in Barcelona City. We reviewed 3920 electronic health records selecting patients, per year (2010‐2014), with VLUs based on the ICD‐10 diagnoses. For prevalence, we took into account any patient with an active VLU in the year of study. For incidence, we took into account patients with a new VLU in the year of study. A descriptive analysis was carried out based on each of the collected variables. The variables were examined according to the years of study (time series) by one‐factor analysis of variance (anova) or Kruskal–Wallis non‐parametric test, as appropriate. A survival analysis by Kaplan–Meier curves and log‐rank test was also performed. A total of 139 patients met the VLU criteria. Among them, only 79.2% were classified as having a VLU and had a correct ICD diagnosis. The prevalence and incidence increased over the years, doubling in patients aged over 65 years. Incidence increased from 0.5 new cases per 1000 people/year in 2010 to 1 new case for every 1000 people/year in 2014. Moreover, the prevalence ranged between 0.8 and 2.2 patients with VLU for every 1000 people/year. During the study period, a total of 84.2% of the VLUs healed (117/139 VLU). Regarding average annual time to healing, the trend indicates that lesions took less time to heal (Kruskal–Wallis test, P = 0.004), ranging between 453,9 weeks in 2005 to 19 weeks in 2014. The use of ABPI also evolved and was found to be increasingly performed prior to the appearance of the lesion. The epidemiological profile of people affected by VLUs continues to be, mainly, that of women of an advanced age, over 70 years. The frequency of VLU occurrence rose continually over the years, but healing took less time, and use of ABPI improved. Assigning a reference nurse in the wounds unit and the organisational structure around this problem may have an influence on improving care and the approach to these types of lesions.
Keywords: incidence, nursing, prevalence, primary care health, venous leg ulcers
1. INTRODUCTION
Lower‐extremity wounds (LEWs) represent an important public health problem for patients, the health system, and society in general. The pathology leads to heavy workloads both in terms of dedicated time and costs by increasing nursing consultations, mainly in primary care.1, 2, 3
The prevalence of chronic wounds increases with age, and with the progressive aging of the population, the number of patients with LEWs has risen, leading to growing efforts to address the problem.4, 5 In fact, it has been found that at least 10% of the population will develop a chronic wound during their lifetime, and the mortality rate related to these injuries is 2.5%.6
As mentioned above, LEW are chronic: only 20% heal within less than 3 months, 50% take more than 1 year to heal, 20% take over 2 years, and the remaining 10% never heal.1, 2 This chronicity entails high costs for society and the health system, while patients' quality of life is affected; the problem is thus more than merely economic.7, 8 In Europe, the cost of treating venous leg ulcers (VLUs) represents approximately 1% of the global budget.2 Studies such as those carried out in the UK show that 2% of the annual national health budget is spent on the care of LEWs.9
The LEWs are not a disease in themselves; they always stem from an underlying systemic pathology, of vascular origin in many cases.1, 10 Thus, a VLU is the most serious complication that may arise from the evolution of chronic venous insufficiency (CVI).2, 11 Around 75% to 80% of total LEWs are VLUs. It is estimated that between 40% and 50% remain active between 6 and 12 months, and 10% up to 5 years.3 Data on VLU recurrence rates are variable and scarce, but recent studies estimate that average recurrence time is 42 weeks, with an incidence rate of 22% at 3 months, 39% at 6 months, 57% at 12 months, 73% at 2 years, and 78% over a 3‐year follow up.12
In Spain, prevalence is estimated at 0.5% to 0.8%, doubling in patients aged over 65 years, and with an incidence of 2 to 5 new cases per 1000 people per year.2, 13 Therefore, it is estimated that there are more than 300 000 patients.13, 14
Regarding the affected person's profile, ulcers are more frequent in women (65%‐70%),2 with a ratio of 3:1 in relation to men, with an average age between 70 and 79 years, among whom 50% have already undergone a previous episode, 50% have difficulties with daily life activities, and 25% suffer anxiety or depression.4, 12
Of note, it is important that each patient presenting a LEW be appropriately classified and a correct differential diagnosis be performed, not only through physical examination and pulse palpation but also by taking an Ankle‐Brachial Pressure Index (ABPI) measurement.1, 2 Correct patient diagnosis helps to select subsequent treatment; furthermore, if this treatment is mainly based on compression therapy, healing rates drop significantly.12, 15, 16 A nurse who is a wounds expert or has been specifically trained can also contribute to the evolution. We must not forget either how important it is to adequately organise wound management, which is also directly linked to the healing process.17
In Spain, literature on the frequency of this problem in primary health care is scarce.14, 18 Moreover, methodological problems exist in different national and international studies. Information is also lacking on whether diagnostic tests, such as ABPI, are routinely performed and on lesions' healing rates.
Based on the hypothesis that, despite efforts to improve diagnosis and treatment, incidence and prevalence have increased over time, we set ourselves the objectives of describing and analysing the temporal trends in the prevalence and incidence of VLUs over the years 2010 to 2014, of determining the percentage of healed ulcers and the temporal trend of this percentage during the study period, and evaluating the temporal and average interval between ABPI completion and the diagnosis of VLUs in a primary health care centre.
2. METHODS
2.1. Study design
This was a retrospective time series (years 2010‐2014) study of the prevalence and incidence of VLUs in a primary care health centre in Barcelona City based on information from the SIDIAP (the Catalan Information System for the Development of Research in the Primary Care System) database.
2.2. Population under study
The study population included all people aged 40 years and over presenting to the primary care centre “Pare Claret” from 2010 to 2014, with an estimated average yearly population of more than 56 000 inhabitants.
2.3. Inclusion criteria
Inclusion criteria were: all patients aged 40 years and over, registered in the electronic health history database (e‐CAP), who presented a diagnosis of CVI and VLU according to the 10th International Classification of Diseases (ICD). The patient had to have a diagnosis of CVI (I87.2) and VLU (I83.0). The sample size, therefore, was not calculated as all patients in the database meeting these criteria were included.
2.4. Criteria to determine prevalent and incident cases
To select the cases of VLU and CVI, the electronic health history records (e‐CAP) were filtered, per year, based on the ICD diagnoses. Because of possible limitations in the records, the following codes were also evaluated: lymphoedema (I89.0), alteration in skin integrity (Nanda: I00046), alteration of tissue integrity (Nanda: I00044), and non‐acute wound (T14/T14.1). We therefore considered, for prevalence, any patient presenting an active VLU in the year of study and, for incidence, patients with a new VLU in the year of study. Patients were only included once on the database to avoid statistical issues like collinearity. Then, a patient who developed a VLU was only considered incident the first time; the other cases were considered prevalent cases.
2.5. Variables
In addition to the variables mentioned above, sociodemographic and comorbidity variables, as well as variables relating to the ulcer, were collected. Only variables that could be filtered from SIDIAP database were finally included.
The following variables were tentative and were included in an Excel spreadsheet that was later converted to an SPSS database:
CVI and VLU.
Prevalence and incidence of VLUs during the 2010 to 2014 study period (calculated as the ratio between the number of VLUs diagnosed as prevalent or incidental and the total population attended to during the study period). As previously stated, an incidental case corresponded to any new lesion with a new register date in the e‐CAP. In addition, an incidence and prevalence calculation was made for people over 65 years of age. For that calculation, only population over that age and per year was used as denominator.
Healing time (measured according to the difference between the date of register in e‐CAP and the date of ulcer healing). A healed ulcer was considered to be a lesion with a register date and that figured as terminated both clinically and in the e‐CAP.
Number of recurrences during the study period (new lesions having appeared during the study process: all new lesions appearing in the same limb that had previously healed and were shown as finalised both in the clinical history and electronic record were considered recurrent).
Sociodemographic variables: gender and age of the patient in years (when the VLU started) and location of care (whether the patient was attended to at the health centre or at home).
Value of the ABPI based on diagnostic confirmation.
Time interval between the patient's VLU development and diagnosis through ABPI, measured according to the difference between the date of VLU and the date of ABPI procedure.
2.6. Sources of information
The data were obtained from the ICS electronic health history record (e‐CAP) based on SIDIAP data (Information System for the Development of Research in the Primary Care System).
2.7. Data collection and procedure
An ordered list of computerised medical records was extracted for all patients having ICD code references and was discharged between January 1, 2010 and December 31, 2014. All the information was retrieved from the e‐CAP using year and diagnostic code filters. The data were entered anonymously into a database for statistical analysis. The database was refined according to the criteria to determine VLU cases. In cases of doubt, we proceeded to review the patient's complete clinical history to avoid registry and information biases.
2.8. Ethical considerations
The study was performed in accordance with the Helsinki declaration. The protocol was reviewed and approved by the Clinical Research Ethics Committee of the Jordi Gol Institute of Research in Primary Healthcare (IDIAP). It was not necessary to request the patient's consent as the data were extracted from a computerised registry and treated in a grouped and always confidential manner according to patient data protection and confidentiality law (Organic Law 15/1999 of 13 December on the Protection of Personal Data and its implementation Regulation, Royal Decree 1720/2007 of 21 December).
2.9. Statistic analysis
2.9.1. Data verification
For the quantitative variables, impossible values were detected by searching for out‐of‐range values (by editing the minimum and maximum value of each variable). For the qualitative variables, impossible values were detected by using the frequency tables of each variable.
2.9.2. Descriptive analysis
We proceeded to describe the population under study in relation to each of the variables studied. Absolute numbers and percentages described qualitative variables. Quantitative variables were described based on measures of central tendency (mean and median) and dispersion (standard deviation, maximum and minimum values). The results are also presented in figures.
2.9.3. Inferential analysis
Mainly non‐parametric statistics were used according to the characteristics of the study variables that were time‐dependent. The variables were analysed according to the years of study (time series) by analysing one‐factor analysis of variance (anova) or the non‐parametric Kruskal–Wallis test, as appropriate. A survival analysis was applied to calculate healing likelihood over time. When appropriate, a Log‐Rank test was performed. A 95% confidence interval was considered, and statistical significance was based on α = 0.05.
3. RESULTS
We reviewed 3920 clinical histories from the e‐CAP and found that only 139 patients fulfilled the VLU diagnostic criteria. A total of 67.4% of patients were treated at the centre and 32.6% at home.
Altogether, there were more women (54.8% CI95% = [46.0%‐63.4%]). Distribution of gender per year is shown in Figure 1. As we have patients who developed a VLU before 2010 but remain prevalent in the study period, we represent in Figure 1 the years of the beginning of the VLU. Note that only 10 patients were included before 2010 (mostly women, 70%). Although there were no statistically significant differences (chi‐square test, P = 0.632) and small subgroups before 2010, a percentage of women higher than 50% was found over time, except in year 2011.
Figure 1.
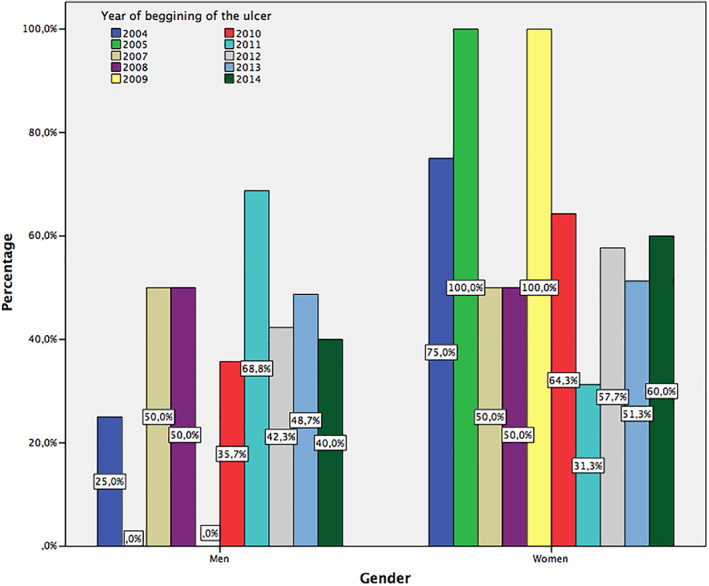
Distribution of gender of patients with venous leg ulcers (VLU). Trend over years
Overall, the patients were aged 79.3 ± 13.7 years, CI95% = [77.0‐81.7] (median = 83 years, minimum: 25 years and maximum: 97 years). Age tendencies are shown in Figure 2; no differences were found per year either (Kruskal–Wallis test, P = 0.357). Of note, some patients may have been included in the analysis over the years until their VLUs healed, and we did not observe any patient who died over the study period or who was moved away to other centre as they were assigned to a unique primary health centre. On the other hand, it was not possible to gather data on recurrences because of the collection method as we had obtained data from a database in a grouped manner, and recurrence is not a variable registered in a specific field.
Figure 2.
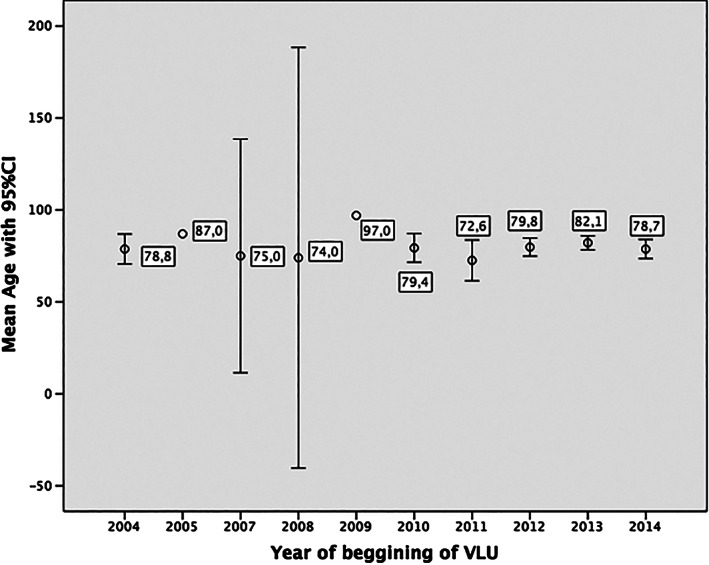
Mean age of patients with venous leg ulcers (VLU). Trend over years
Table 1 shows, in absolute numbers, the population attended to in the health centre per year, as well as new cases and prevalent cases, both in total and regarding the population aged 65 years and over. Visibly, most patients with VLUs were aged 65 years and over.
Table 1.
Population, prevalent, and incident cases studied
| Attended population | Population > 65 | New cases | New cases > 65 | Prevalent cases | Prevalent cases > 65 | |
|---|---|---|---|---|---|---|
| 2010 | 30 653 | 9459 | 14 | 13 | 24 | 23 |
| 2011 | 30 413 | 9392 | 17 | 13 | 34 | 29 |
| 2012 | 30 043 | 9451 | 26 | 24 | 47 | 41 |
| 2013 | 30 388 | 9767 | 41 | 35 | 67 | 56 |
| 2014 | 30 165 | 9428 | 30 | 16 | 64 | 42 |
In relation to prevalence and incidence, both increased over the years (Figures 3 and 4), doubling in patients aged over 65 years. These incidence data show figures ranging from 0.5 new cases for each 1000 people/year in 2010 to 1 new case for every 1000 people/year in 2014. Likewise, the prevalence ranged between 0.8 and 2.2 patients with VLU for each 1000 people/year.
Figure 3.
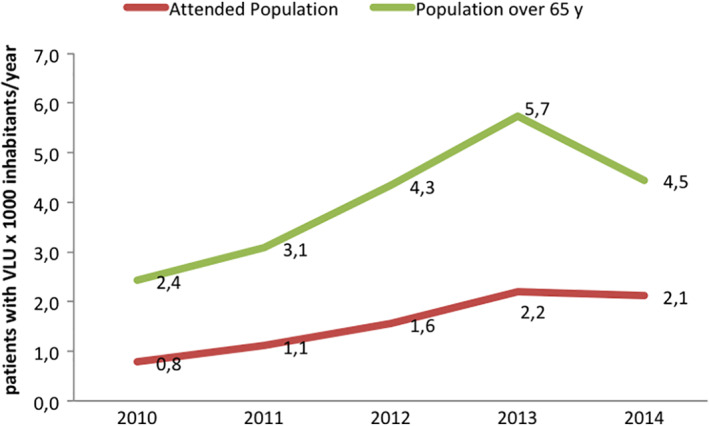
Prevalence trend in the period 2010 to 2014
Figure 4.
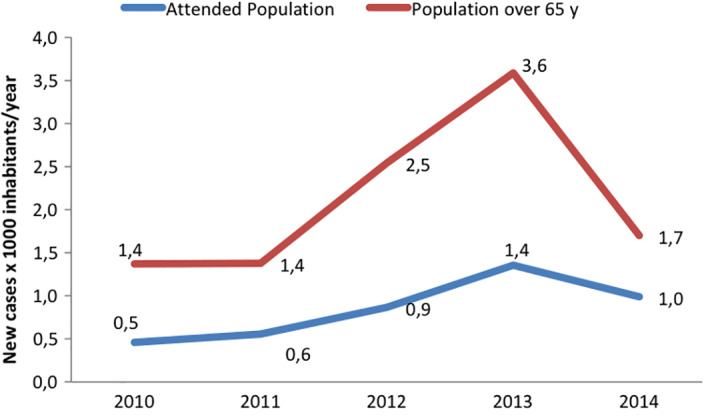
Incidence trend in the period 2010 to 2014
During the study period, 84.2% (CI95% = [77.0%‐89.8%]) of VLUs healed (117 of a total of 139). Figure 5 shows the healing tendency. The line showing “Incident VLU” represents the percentage of VLUs that healed among the new cases each year. The line “Prevalent VLU” indicates the healing of prevalent VLUs each year. As can be observed, healing increased over the years, with values above 50% in 2014. Of 22 unhealed wounds in 2014, 59.1% (13 of 22) were VLU incidents in the same year.
Figure 5.
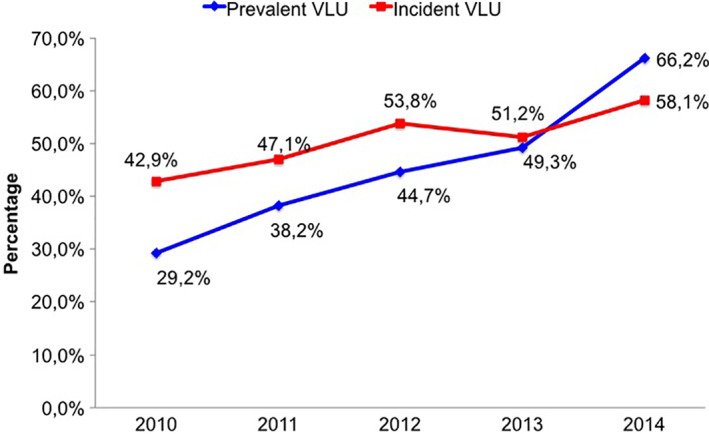
Venous leg ulcer (VLU) healing trend over 2010 to 2014
Regarding healing time, as already mentioned, we calculated the lapse of time between the moment the VLU was registered and the date it appeared as healed in the e‐CAP. Thus, for example, some lesions originating in 2004 healed in one of the years studied. The trend indicates that lesions took less time to heal (Kruskal–Wallis test, P = 0.004), ranging between 453,9 and 19 weeks on average (Figure 6). Consequently, in 2014, healing time figures corresponded to 19.0 ± 12.1 weeks, CI95% = [13.0‐25.0] (median = 14.9 weeks), ranging between 6.3 and 50.0 weeks. Table 2 demonstrates the percentage of VLU healed between those developed in the study period 2010 to 2014 at ≤12, ≤24 or >24 weeks. In addition, when a survival analysis was performed, there was a statistical significant difference between VLU with origin before 2010 and those VLUs that developed during the period 2010 to 2014 (Figure 7), observing that ulcers with origin in the study period had a higher likelihood to heal in less time. Worth noting is that 2010 was the year in which organisational change occurred (a service focused on wound care with a reference nurse). When focussing on usual healing timeframes (12 and 24 weeks), for all cases, the healing likelihood at 12 weeks was 26.2% and was 43.2% at week 24 (Figure 8). There were no differences regarding those likelihoods when they were compared during the 2010 to 2014 period.
Figure 6.
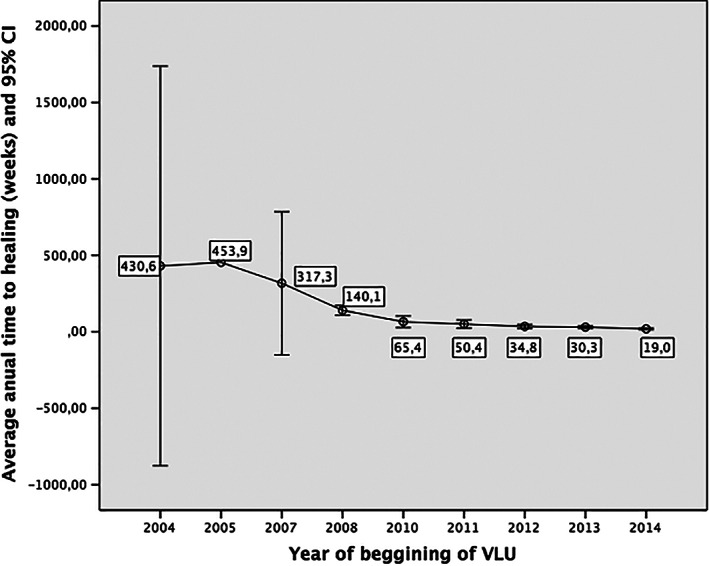
Average annual time to healing
Table 2.
Percentage of venous leg ulcer (VLU) healed at ≤12, ≤24 or >24 weeks for lesions beginning between 2010 and 2014
| ≤12 wk | ≤24 wk | >24 wk | Total | |
|---|---|---|---|---|
| 2010 (n = 14) | 4/14 (28.6%) | 5/14 (35.7%) | 9/14 (64.3%) | 14/14 (100.0%) |
| 2011 (n = 17) | 5/17 (29.4%) | 8/17 (47.1%) | 8/17 (47.1%) | 16/17 (94.1%) |
| 2012 (n = 26) | 6/26 (23.1%) | 14/26 (53.8%) | 12/26 (46.2%) | 26/26 (100.0%) |
| 2013 (n = 41) | 14/41 (34.1%) | 20/41 (48.8%) | 16/41 (39.0%) | 36/41 (87.8%) |
| 2014 (n = 31) | 7/31 (22.6%) | 13/31 (41.9%) | 5/31 (16.1%) | 18/31 (58.1%) |
| Total (n = 129) | 36/129 (27.9%) | 60/129 (46.5%) | 50/129 (38.8)%) | 110/129 (85.3%) |
Figure 7.
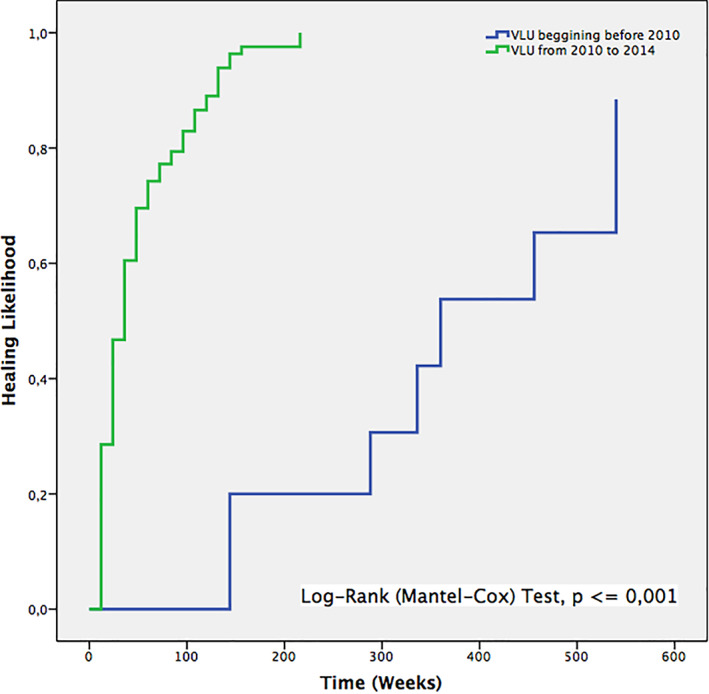
Survival curves of healing, comparing venous leg ulcer (VLU) with origin before 2010 and those VLUs that developed in the period 2010 to 2014
Figure 8.
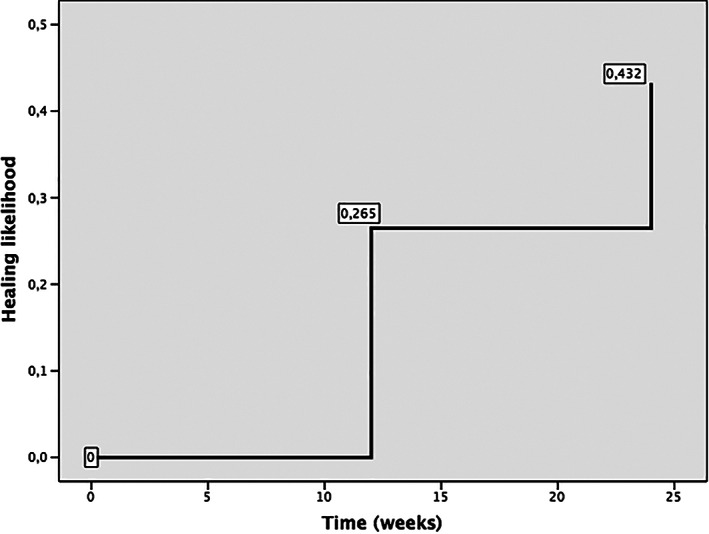
Survival curve of healing (all cases), focusing on healing likelihood at week 12 and 24
As shown in Figure 9, the time interval between the patient's VLU and diagnosis through ABPI decreased, and a clear drop can be observed in the number of days between the patient's VLU and the completion of the ABPI. As of 2013, the ABPI was performed before the VLU episode; therefore, there was progressively more secondary prevention, and/or the patient already had the diagnosis before the lesion appeared.
Figure 9.
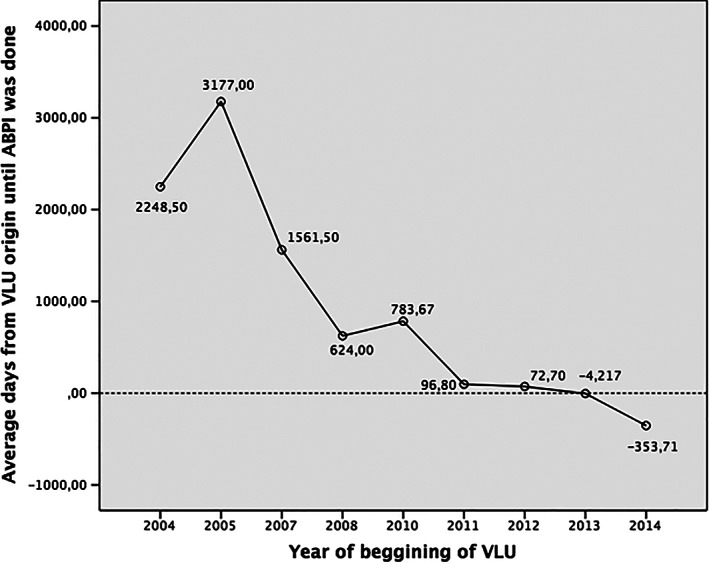
Mean time elapsed between the Ankle‐Brachial Pressure Index (ABPI) test and venous leg ulcer (VLU) diagnostic over time
Of the total number of patients with VLU, only 22.8% had been referred to vascular surgery consultation for some type of complication. Regarding correct diagnosis, 79.2% were classified as VLU with the correct ICD diagnosis, and only 56.6% had an ABPI in the corresponding e‐CAP record. This means that, in many cases, the complete history had to be reviewed to establish whether there really was a VLU.
4. DISCUSSION
VLUs can continue to be considered a major public health problem, affecting a significant amount of people, mainly elderly women, entailing important costs. According to O'meara et al,19 1% of the western population will suffer at some time in their lives from a VLU. In our case, data on prevalence and incidence increased over the years, and in general, the rates we found were lower than those reported in the Spanish National Lower Extremity Ulcer Consensus Conference (CONUEI) document (0.5%‐0.8%)2; they coincided with the study by Spain's National Pressure Ulcer and Chronic wounds Study and Guidance Group (GNEAUPP) on VLUs,18 with that of Harding et al3 and with those mentioned in the Clinical Practice Guideline (CPG) of the Scottish Intercollegiate Nursing Guidelines (SING),20 which reported values between 0.1% and 0.3%. Regarding incidence, references were scarce, and we could only mention the estimates present in some of the documents.2 In our case, incidence was much lower, regardless of the period studied, with figures ranging from 0.5 cases per 1000 people/year to 1 case per 1000 people/year.
However, to compare data with other studies is difficult because of different methods, populations, and prevalence and incidence formulas. For instance, Margolis et al21 reported an annual prevalence rate of 1.69% in elderly population and an overall incidence rate of 1.20 to 1.13 per 100 person‐years when the disease‐free period varied from 3 to 9 months for the UK elderly population. Heyer et al22 refers to an incidence rate in 2012 of 0.16% in Germany, and McCosker et al23 recently performed a systematic review focusing on the epidemiology of chronic wounds in Australia and reporting a wide variation on figures of prevalence between studies and found that no data exist on incidence figures for Australia.
In terms of healing, increasingly higher amounts of VLUs were healed, reaching over 50% of cases. Thus, in 2014, the percentage of healed VLUs was over 60%. These figures are better than those found in other studies, such as that of Brown et al,24 where 45% healed over a period of 6 months, or that of Harrison et al,17 where healed cases accounted for 58.3% of cases in health centres and 56.7% in homes over 3‐month period. Healing times also improved, reaching 19 weeks (4.75 months) in 2014. These healing times are shorter than those published in the most recent studies that provide estimations of 5.9 months.25 Regarding healing at 12 and 24 weeks, survival curves, taking into account all cases, show a healing likelihood of 26.5% and 43.2%, respectively; as given in Table 2, for wounds originating between 2010 and 2014, we found values ranging between 22.6% and 34.1% at 12 weeks. For the 24‐week period, 35.7% to 53.8% healing were achieved. Data were similar to those found by McCosker et al23 in Australia.
VLUs are known to be recurrent, but recurrence rate data for VLUs are varied and scarce. A systematic review by Nelson et al15 on compression to prevent VLU recurrence indicates that the recurrence rate at 12 months varies between 26% and 69%. As mentioned in the introduction, a recent study12 estimated that the average relapse time was 42 weeks, with an incidence of 22% at 3 months, 39% at 6 months, 57% at 12 months, 73% at 2 years, and 78% within a 3‐year follow up. Weller and Evans,26 in a study in Australia, where 2% of the western population has CVI, it was indicated that 1 in 5 patients had a VLU and many recurrent episodes, noting that most nurses did not feel safe using the ABPI, nor were they responsible for the compression therapy. In our study, however, it was not possible to obtain lesion recurrence data because of the methodology used (aggregate data obtained from an electronic record and provided by health technicians who filtered the information).
Regarding possible explanations of the results, and in line with Harrison et al,17 who concluded that what determined healing was not the location of the treatment but the organisation of care, these results in prevalence, incidence, and healing are probably closely related to the organisational change that took place, as of 2010, in the health centre “Pare Claret,” where this research was carried out. This change included the creation of a wound unit and the proactive role of reference wound nurses per patient.
Like all studies, this research is not exempt of biases and/or limitations. Limitations proper to a retrospective time series study can be found, in which, as described, we worked with information from an electronic health record. This implies possible information and registration bias because of a lack of correct record keeping and/or inadequate classifications. We were not aware either whether any interventions, in addition to those mentioned in the discussion, during this period had any effect on what we could observe (history and/or maturation bias). However, to counter this limitation as much as possible, as indicated in the methods section, when searching for patients with VLUs using the VLU selection criteria, an exhaustive examination of full clinical histories was performed, including that of free observation fields in the records. We also analysed any diagnosis code that could be confused with VLU.
5. CONCLUSIONS
Incidence and prevalence increased throughout the years under study and doubled in patients aged 65 and over. In a primary care centre, the profiles of people with VLUs mainly corresponded to women of an advanced age above 70 years.
Despite there being greater incidence and prevalence, the healing process improved over the years and took less time over the period under study. Furthermore, increasingly less time elapsed between the detection of the ulcer and its diagnostic confirmation via ABPI.
The role of a reference nurse at the wounds unit and the organisational structure around this problem can lead to improvements and influence approaches to this type of lesion. The effects of these interventions on VLU approaches and healing should be examined through future experimental studies.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
ACKNOWLEDGEMENTS
We thank the Catalan Institute of Health (ICS) for providing us with access to electronic health records, especially Dr. Francesc Orfila for his support in creating the database. We also thank the Translation Service at the University of Alicante. This paper reports partial data of a PhD thesis (first phase) developed by the first author. This project was funded by a research grant from the Catalan Institute of Health with reference (XB).
Berenguer Pérez M, López‐Casanova P, Sarabia Lavín R, González de la Torre H, Verdú‐Soriano J. Epidemiology of venous leg ulcers in primary health care: Incidence and prevalence in a health centre—A time series study (2010‐2014). Int Wound J. 2019;16:256–265. 10.1111/iwj.13026
Funding information Institut Català de la Salut, Grant/Award Number: Mòduls de Recerca del Àmbit d'Atenció Primari
REFERENCES
- 1. Marinel.lo J. Concepto, clasificación y epidemiología de las úlceras de la extremidad inferior. In: Marinel.lo Roura J, ed. Úlceras de la extremidad inferior. 1st ed. Barcelona, Spain: Glosa; 2005:25‐44. [Google Scholar]
- 2.Conferencia Nacional de Consenso sobre úlceras de la Extremidad Inferior‐ CONUEI. Documento de Consenso CONUEI. Barcelona, Spain: Edikamed S.L.; 2009.
- 3. Wipke‐Tevis DD, Rantz MJ, Mehr DR, et al. Prevalence, incidence, management, and predictors of venous ulcers in the long‐term‐care population using the MDS. Adv Skin Wound Care. 2000;13(5):218‐224. [PubMed] [Google Scholar]
- 4. Briggs MCS. The prevalence of leg ulceration: a review of the literature. EWMA J. 2003;3(2):14‐20. [Google Scholar]
- 5. Lal BK. Venous ulcers of the lower extremity: definition, epidemiology, and economic and social burdens. Semin Vasc Surg. 2015;28(1):3‐5. [DOI] [PubMed] [Google Scholar]
- 6. Sasanka CS. Venous ulcers of the lower limb: where do we stand? Ind J Plastic Surg. 2012;45(2):266‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smith JJ, Guest MG, Greenhalgh RM, Davies AH. Measuring the quality of life in patients with venous ulcers. J Vasc Surg. 2000;31:642‐649. [DOI] [PubMed] [Google Scholar]
- 8. González‐consuegra RV, Verdú J. Quality of life in people with venous leg ulcers: an integrative review. J Adv Nurs. 2011;67(5):926‐944. [DOI] [PubMed] [Google Scholar]
- 9. Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American venous forum. J Vasc Surg. 2011;53(5 suppl):2S‐48S. [DOI] [PubMed] [Google Scholar]
- 10. Abbade LP, Lastória S, Rollo Hde A. Venous ulcer: clinical characteristics and risk factors. Int J Dermatol. 2011;50(4):405‐411. [DOI] [PubMed] [Google Scholar]
- 11. Lozano Sánchez FS, Carrasco Carrasco E, Díaz Sánchez S, Escudero Rodríguez JR, Marinel.lo Roura J, Sánchez Nevarez I. Determinantes de la gravedad en la insuficiencia venosa crónica. Estudio C‐VIVES. Angiologia. 2013;65(1):1‐9. [Google Scholar]
- 12. Finlayson K, Wu ML, Edwards HE. Identifying risk factors and protective factors for venous leg ulcer recurrence using a theoretical approach: a longitudinal study. Int J Nurs Stud. 2015;52(6):1042‐1051. [DOI] [PubMed] [Google Scholar]
- 13. Sociedad Española de Angiología y Cirugía Vascular . Capítulo Español de Flebología. Libro Blanco sobre insuficiencia venosa crónica y su impacto en la Sanidad Española. Horizonte del año 2012. Macro‐estudio prospectivo basado en el método Delphi. Madrid, Spain: SEACV; 2004. [Google Scholar]
- 14. Álvarez J, Lozano F, Marinel.lo J, Masegosa A. Estudio DETECT 2006: encuesta epidemiológica realizada en España sobre la prevalencia asistencial de la IVC en atención primaria. Angiologia. 2008;60(1):27‐36. [Google Scholar]
- 15.Nelson EA, Bell‐Syer SEM, Cullum NA, Webster J. Compression for preventing recurrence of venous ulcers. Cochrane Database of Systematic Reviews 2000, Issue 4. Art. No.: CD002303. 10.1002/14651858.CD002303 [DOI] [PubMed] [Google Scholar]
- 16. Lazarus G, Valle MF, Malas M, et al. Chronic venous leg ulcer treatment: future research needs. Wound Repair Regen. January–February 2014;22(1):34‐42. 10.1111/wrr.12102 Epub 2013 October 17. [DOI] [PubMed] [Google Scholar]
- 17. Harrison MB, Graham ID, Lorimer K, et al. Nurse clinic versus home delivery of evidence‐based community leg ulcer care: a randomized health services trial. BMC Health Serv Res. 2008;8:243. Available from:. http://www.biomedcentral.com/1472-6963/8/243. Accessed May 15, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Soldevilla J, Torra JE, Verdú J, Rueda J, Martínez F, Roche E. Epidemiology of chronic wounds in Spain: results of the first national studies on pressure and leg ulcer prevalence. Wounds. 2006;18(8):213‐226. [Google Scholar]
- 19. O'Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev. November 14, 2012;11:CD000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Scottish Intercollegiate Guidelines Network (SIGN) . Management of Chronic Venous Leg Ulcers. A National Clinical Guideline. Edinburgh, UK: SIGN; 2010. Available from: http://www.sign.ac.uk. Accessed May 17, 2018. [Google Scholar]
- 21. Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol. 2002;46(3):381‐386. [DOI] [PubMed] [Google Scholar]
- 22. Heyer K, Protz K, Glaeske G, Augustin M. Epidemiology and use of compression treatment in venous leg ulcers: nationwide claims data analysis in Germany. Int Wound J. 2017;14:338‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McCosker L, Tulleners R, Cheng Q, et al. Chronic wounds in Australia: a systematic review of key epidemiological and clinical parameters. Int Wound J. September 26, 2018. 10.1111/iwj.12996 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brown A, Bums E, Chalmers L, et al. Effect of a national community intervention programme on healing rates of chronic leg ulcer: randomised controlled trial. Phlebology. 2002;17(2):47‐53. [Google Scholar]
- 25. Sauer K, Rothgang H, Glaeske G. BARMER GEK Heil‐ und Hilfsmittelreport 2014. Available from: https://www.barmer.de/blob/36198/.../data/pdf-heil-und-hilfsmittelreport-2014.pdf. Accessed October 20, 2018.
- 26. Weller C, Evans S. Management of venous leg ulcer in general practice—practice nurses and evidence based guidelines. Aust Fam Physician. 2012;41(5):331‐337. [PubMed] [Google Scholar]


