Abstract
The Wolf isotopic response describes the occurrence of a new, unrelated disease that appears at the same location as a previously healed disease. The most common primary skin disorder of this phenomenon is herpes zoster and less frequently, herpes simplex. We report a case of 79‐year‐old woman who have bullous pemphigoid (BP) with dermatomal distribution that developed at the site of previously healed herpes zoster. Based on clinical, histological and immunofluorescence findings, the patient was diagnosed with localized BP in a site of prior herpes zoster. BP developing at the site of healed herpes zoster is the first reported case. Recognition of this phenomenon is important for correct clinicopathologic diagnosis and may improve our understanding of the underlying pathophysiologic processes.
Keywords: Isotopic response, Pemphigoid, Zoster
The term ‘isotopic response’ was coined by Wolf in 1995 to describe the occurrence of a new skin disorder at the site of another unrelated and already healed skin disease 1. Isotopic response is distinctly different from an isomorphic response, which is also known as the Koebner phenomenon that describes the development of the same disease at a site of damaged or traumatised skin. The most common primary skin disorder of isotopic response phenomenon is herpes virus infection: herpes zoster is most common and herpes simplex and varicella are less frequent 2. Several cutaneous lesions such as comedones, xanthoma, granuloma annulare, granulomatous dermatitis, acneiform eruption, pseudolymphoma, psoriasis, lichen planus, lichen simplex chronicus, eosinophilic dermatosis and cutaneous malignancy have been reported to occur at the site of a herpes zoster scar 2.
A 79‐year‐old female patient presented to our clinic with a week history of painful clusters of vesicles in a zosteriform distribution from T2 to T4 on the right anterior chest to C5 to C6 on the right upper extremity, which was diagnosed as herpes zoster. The herpetic infection had been treated with valacyclovir 1000 mg three times a day for 7 days. The lesions resolved in 2 weeks after the onset of the eruption. A month after the resolution of herpes zoster, she developed vesicles and bullae at the sites of the previously healed herpes zoster and the lesions had spread. On physical examination, there were multiple tense vesicles and bullae associated with crusting and erosions on the right breast and the right upper extremity (Figure 1). Histopathological examination was performed for the differential diagnosis among bullous pemphigoid (BP), linear IgA bullous dermatosis. The biopsy showed sub‐epidermal bulla formation filled with numerous eosinophils (Figure 2). Direct immunofluorescence from peri‐lesional skin showed linear staining of the basement membrane zone (BMZ) with IgG and C3. 1 mol/l NaCl salt split skin test showed the presence of IgG autoantibodies and C3 bound to the epidermal side. The patient was diagnosed with BP at the site of the healed herpes zoster as an isotopic response. She started on oral prednisolone 40 mg daily, which resulted to a complete healing of the erosions within 2 months.
Figure 1.

Multiple tense vesicles and bullae associated with crusting and erosions on the right breast and the right upper extremity.
Figure 2.
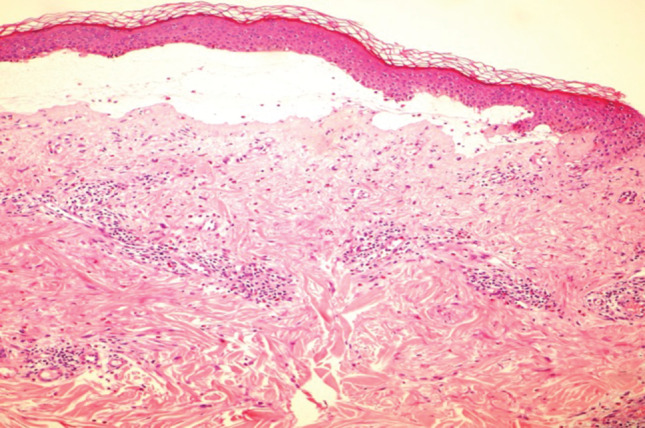
Sub‐epidermal blister filled with numerous eosinophils.
The isotopic response refers to the appearance of a new disease process within the same location as a previous disease. The interval between the first and the second disease is diverse ranging from days to years 1. Isotopic response may have different pathogenetic explanations, and viral, vascular, neural and immunological factors may play a relevant role 3.
The pathogenesis of BP is characterised by tissue‐bound and circulating IgG autoantibodies against two components of the hemidesmosome of stratified epithelia, BP 230 kD (BPAg1) and BP 180 kD (BPAg2, COL17). Most cases of BP occur apparently without any obvious precipitating factor; however, the inducing factors of BP can be identified in several cases such as drug intake, physical agents and viral infections. Viruses can induce autoimmune diseases and may share epitopes with its host, thus leading to the development of cross‐reactive autoantibodies (molecular mimicry). In isotopic response, some neural alteration might be the first step, with subsequent impairment of immunological function, and viral and vascular mechanisms may be only cofactors in certain cases 2. The relationship between BP and neurologic disease was found to be statistically significant. Four major neurologic diagnoses were observed including cerebrovascular disease, dementia, Parkinson's disease and epilepsy. The link between BP and neurologic diseases could potentially be explained by the presence of an immunological cross‐reactivity between the skin and the brain. Also, herpes zoster can be considered as one of the infectious peripheral nerve diseases 4, 5.
Localised BP (LBP) is a rare autoimmune sub‐epidermal bullous disorder characterised by chronic intermittent eruptions that affect only a restricted area of the body. The distribution of lesions on our patient was limited to the field that fits to the T2–T4 and C5–C6 dermatomes. We believe that our case can be categorised as LBP, according to the lesion distribution, specifically as zosteriform. The pathogenesis of LBP is most likely similar to that of generalised BP 6. However, the localised nature of the lesions may be due to local factors in addition to an immune reaction. Local factors such as trauma, UV light 7, hydrostatic pressure and, as in our case, previously resolved but unrelated skin lesion like herpes zoster infection may play a role in the pathogenesis of LBP. It differs from the generalised form by its more benign course. Localised lesions may remain localised or develop into classical BP 8. In our patient, no rebound after 1 year on maintenance therapy and no residual scarring were observed.
Wolf isotopic response remains an interesting phenomenon; recognition of this phenomenon is important for the correct diagnosis and may improve our understanding of the underlying pathophysiological processes.
References
- 1. Wolf R, Brenner S, Ruocco V, Filioli FG. Isotopic response. Int J Dermatol 1995;34:341–8. [DOI] [PubMed] [Google Scholar]
- 2. Ruocco V, Ruocco E, Ghersetich I, Bianchi B, Lotti T. Isotopic response after herpesvirus infection: an update. J Am Acad Dermatol 2002;46:90–4. [DOI] [PubMed] [Google Scholar]
- 3. Wolf R, Lotti T, Ruocco V. Isomorphic versus isotopic response: data and hypotheses. J Eur Acad Dermatol Venereol 2003;17:123–5. [DOI] [PubMed] [Google Scholar]
- 4. Langan SM, Groves RW, West J. The relationship between neurological disease and bullous pemphigoid: a population‐based case‐control study. J Invest Dermatol 2011;131:631–6. [DOI] [PubMed] [Google Scholar]
- 5. Taghipour K, Chi CC, Vincent A, Groves RW, Venning V, Wojnarowska F. The association of bullous pemphigoid with cerebrovascular disease and dementia: a case‐control study. Arch Dermatol 2010;146:1251–4. [DOI] [PubMed] [Google Scholar]
- 6. Kawahara Y, Matsumura K, Hashimoto T, Nishikawa T. Immunoblot analysis of autoantigens in localized pemphigoid and pemphigoid nodularis. Acta Derm Venereol 1997;77:187–90. [DOI] [PubMed] [Google Scholar]
- 7. Pfau A, Hohenleutner U, Hohenleutner S, Eckert F, Landthaler M. UVA provoked localized bullous pemphigoid. Acta Dermatol Venereol 1994;74:314–6. [DOI] [PubMed] [Google Scholar]
- 8. Person JR, Rogers RS 3rd, Perry HO. Localized pemphigoid. Br J Dermatol 1976;95:531–4. [DOI] [PubMed] [Google Scholar]


