Abstract
The aim of this study was to develop a tool to measure the knowledge of nurses on pressure ulcer prevention. PUKAT 2·0 is a revised and updated version of the Pressure Ulcer Knowledge Assessment Tool (PUKAT) developed in 2010 at Ghent University, Belgium. The updated version was developed using state‐of‐the‐art techniques to establish evidence concerning validity and reliability. Face and content validity were determined through a Delphi procedure including both experts from the European Pressure Ulcer Advisory Panel (EPUAP) and the National Pressure Ulcer Advisory Panel (NPUAP) (n = 15). A subsequent psychometric evaluation of 342 nurses and nursing students evaluated the item difficulty, discriminating power and quality of the response alternatives. Furthermore, construct validity was established through a test–retest procedure and the known‐groups technique. The content validity was good and the difficulty level moderate. The discernment was found to be excellent: all groups with a (theoretically expected) higher level of expertise had a significantly higher score than the groups with a (theoretically expected) lower level of expertise. The stability of the tool is sufficient (Intraclass Correlation Coefficient = 0·69). The PUKAT 2·0 demonstrated good psychometric properties and can be used and disseminated internationally to assess knowledge about pressure ulcer prevention.
Keywords: Knowledge assessment tool, Nursing, Pressure ulcers, Prevention, Psychometric validity
Introduction
Pressure ulcer prevalence in Europe remains high, between 8·9% and 18·2% in hospitals and between 6·4% and 31·4% in nursing homes 1, 2, 3. To improve the quality of care, nurses should possess up‐to‐date knowledge concerning the prevention of pressure ulcers. Knowledge is important to decide which patients need prevention, which measures are effective and how these measures should be applied. Knowledge also has an impact on the attitude of nurses towards pressure ulcers, which in turn is significantly correlated with the application of adequate pressure ulcer prevention 4. Research demonstrated that on the one hand, only 10·8–13·9% of the patients at risk received adequate prevention. On the other hand, more than 70% of the patients without risk received a form of prevention, which is redundant and inefficient 4, 5. Lack of knowledge and a negative attitude towards pressure ulcer prevention are common barriers for the application of guidelines in clinical practice 6.
The worldwide guidelines for pressure ulcer management recommend the assessment of the knowledge of nurses about pressure ulcer prevention regularly using a reliable and valid assessment tool 6. Multiple knowledge assessment tools were developed internationally, but the limited evaluation of the psychometric properties is a major problem 7. One of the most common internationally used knowledge assessment tools is the Pressure Ulcer Knowledge Assessment Tool (PUKAT) 7, 8, 9, 10, 11. This tool was developed in 2010 by Beeckman et al. at Ghent University, Belgium. The PUKAT has proven to be valid and reliable and consists of 26 multiple‐choice items covering six themes: aetiology and development, classification and observation, nutrition, risk assessment, prevention: reduction of the magnitude of pressure and shearing and prevention: reduction of the duration of pressure and shearing. The tool has good content validity (CVI = 0·78–1·00) and a high test–retest reliability (ICC = 0·88) 7, but it is no longer up‐to‐date. Recently, several new evidence‐based guidelines for the prevention and treatment of pressure ulcers were published 1, 6, 12. The Belgian Health Care Knowledge Centre (KCE) published a national guideline for the prevention of pressure ulcers 1. Besides, the collaboration between the European Pressure Ulcer Advisory Panel (EPUAP), the National Pressure Ulcer Advisory Panel in the USA (NPUAP) and the Pan Pacific Pressure Injury Alliance (PPPIA) resulted in a second edition of their evidence‐based guidelines for the prevention and treatment of pressure ulcers 6. Finally, the National Institute for Health and Care Excellence (NICE) also published an update of their guidelines for the prevention and treatment of pressure ulcers 12. Because of the large number of new guidelines, the PUKAT 7 was no longer up‐to‐date. A knowledge assessment tool integrating the recent guidelines was needed to be able to measure the knowledge of nurses and nursing students about pressure ulcer prevention according to the newest guidelines. The aim of this study was to meet this need by developing and testing the validity and reliability of a new knowledge assessment tool based on the PUKAT 7 and the recently published national and international guidelines.
Methods
Study design
A prospective psychometric instrument validation study was designed. Content validity, face validity, validity of the multiple‐choice test items (item difficulty, discriminating index and quality of the response alternatives), construct validity and stability of the knowledge assessment tool were evaluated.
Development of the tool
The development of the knowledge assessment tool was based on the phases described by Mishel 13.
Phase 1: tool development
The themes of the new tool were: aetiology, classification and observation, risk assessment, nutrition, prevention of pressure ulcers and specific patient groups. These themes were in line with the original PUKAT 7. However, the theme prevention contained both the components reduction of the magnitude and reduction of the duration of pressure and shear. A new theme was also created to integrate items about the specific guidelines for particular patient groups. Based on the PUKAT and the new guidelines from the Belgian Health Care Knowledge Centre (KCE) 1, the EPUAP/NPUAP/PPPIA collaboration 6 and the National Institute for Health and Care Excellence (NICE) 12, a knowledge assessment tool including 28 multiple‐choice items was developed. Research demonstrated that the way in which multiple‐choice items are composed has an impact on the way in which the question is approached 14. To create a tool with a pedagogically oriented approach, the Multiple‐choice Item‐writing Guideline from Haladyna et al. was used 15. Each item was composed of a stem containing the problem and several response alternatives. The stem included the central idea to promote the thinking process, starting once the question was read 15, 16. Besides, the stem was worded positively 16. A new element was the use of cases and pictures to be able to evaluate theoretical knowledge as well as practical knowledge. For each item, five response alternatives were formulated: two positively worded alternatives, two negatively worded alternatives and a last option to allow the respondent to indicate if he does not know the answer. The presence of an equal amount of positively and negatively worded response alternatives restricted the possibility of one alternative (e.g. the only positively worded) being suggestive. The presence of the supplementary response alternative ‘I do not know the answer’ restricted the possibility of guessing.
The knowledge assessment tool was submitted to two groups of experts and to a pilot study to assess face and content validity. In a first phase, the new version of the knowledge assessment tool was translated into English and submitted to NPUAP. Based on their feedback, both in the English and Dutch versions, structure, the content and language of 21 items were adapted. In the second phase, a panel of seven experts from the EPUAP evaluated the knowledge assessment tool in a Delphi procedure. The experts were five wound care and/or pressure ulcer prevention nurses, a wound care coordinator and a physician specialised in wound care and wound healing. They were asked to assess the importance of the questions (not important at all – not important – important – very important), the clarity of the questions (not clear – clear) and the accuracy of the response alternatives (not correct – correct). Panel members were invited to give further comments and feedback. Based on their feedback, 13 items were adapted and three items removed. In the third phase, the knowledge assessment tool was pilot tested; one nursing student, three nurses with different profiles and a wound care nurse participated. They were asked to assess the readability of questions and response alternatives (hard to read – readable – easy to read), the clarity of the questions (not clear – clear) and the clarity of the response alternatives (not clear – clear). The participants were invited to give further comments and feedback. Based on their feedback, seven items were adapted. Figure 1 gives an overview of the completed phases in the development of the knowledge assessment tool. The new knowledge assessment tool PUKAT 2·0 consisted of 25 multiple‐choice items covering six themes most relevant to pressure ulcer prevention (see Table 1).
Figure 1.
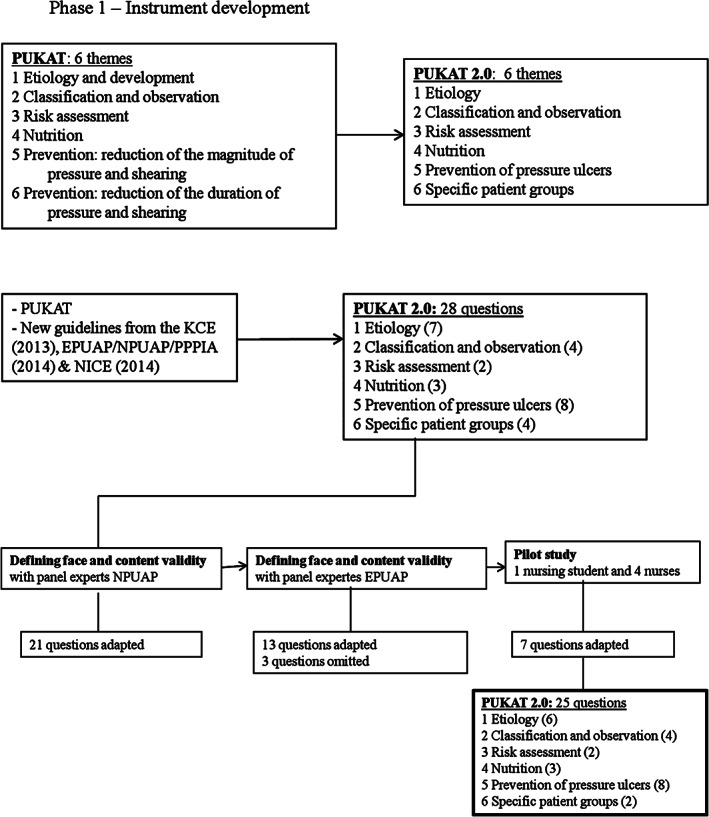
Development of the instrument.
Table 1.
PUKAT 2·0
| THEME: AETIOLOGY |
| 1. There are several causal factors in the development of pressure ulcers. Which of the following factors is one of them? |
| a. Diabetes. |
| b. Incontinence. |
| c. Fever. |
| d. Reduced level of activity.† |
| 2. A patient sits with the head of bed elevated to 60°. What happens when his skin sticks to the underlying surface when he slides down in bed? |
| a. The pressure increases. |
| b. Problems with the microclimate occur (temperature and relative humidity). |
| c. Shear increases.† |
| d. Friction/rubbing increases. |
| 3. What is the average percentage of patients with pressure ulcers in European hospitals? |
| a. Between 1% and 5%. |
| b. Between 5% and 10%. |
| c. Between 10% and 15%.† |
| d. Between 15% and 20%. |
| 4. Excessively moist skin (due to e.g. incontinence or wound exudate) combined with increased body temperature are associated with pressure ulcer development. Is this statement correct? |
| a. Yes, excessive skin moisture and raised temperature cause pressure ulcers. |
| b. Yes, excessive skin moisture and raised temperature are risk factors for the development of pressure ulcers.† |
| c. No, wounds that occur in a moist and warm environment are always defined as incontinence‐ associated dermatitis (IAD). |
| d. No, an increased temperature results in better blood flow and thus decreases the risk of pressure ulcers. |
| 5. CASE: A patient is sitting in a chair in the morning and in the afternoon, each time 2 hours. The rest of the day he spends in bed. He cannot mobilise himself. When does this patient have the highest risk to develop a pressure ulcer (if no prevention is applied)? |
| a. There is no higher risk to develop a pressure ulcer if a seated position in chair is combined with a lying position in bed. |
| b. The risk to develop a pressure ulcer is highest when he is seated in a chair because high pressure is applied during a short period of time. |
| c. The risk to develop a pressure ulcer is highest when he is lying in bed because lower pressure is applied during a longer period of time. |
| d. The risk to develop a pressure ulcer is high in this specific case, both when seated in a chair and lying in bed. A short‐term high pressure can have the same effect as a long‐term low pressure.† |
| 6. Which statement is correct? |
| a. The use of moisture‐absorbing pads decrease the risk of pressure ulcers. |
| b. The use of water and soap can erode the skin barrier, thereby increasing the risk of superficial skin damage.† |
| c. Massaging the skin (during washing and drying) is effective to prevent pressure ulcers. |
| d. Dressing the heels (with a bandage) will decrease the risk of heel pressure ulcer development. |
| THEME: CLASSIFICATION AND OBSERVATION |
| 7. CASE: You observe a new blister on the heel of a patient who can reposition himself in bed. You take a look at his file, but you colleagues never reported a non‐blanchable erythema or a wound. Which statement is correct? |
| a. The blister is not a pressure ulcer. |
| b. The blister is a Category II pressure ulcer. |
| c. The blister is a Category I pressure ulcer as long as it remains intact. |
| d. There is insufficient information to know if this is a pressure ulcer or not.† |
| 8. Which of these pictures is a pressure ulcer category I? |
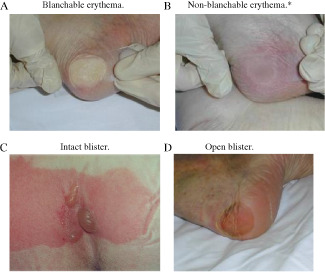
|
| 9. In which of these categories can necrotic tissue be present? |
| a. Category I, II, III and IV. |
| b. Category II, III and IV. |
| c. Category III and IV.† |
| d. Category IV only. |
| 10. CASE: The nurse observes a bony structure in a wound. In which category can you classify this pressure ulcer? |
| a. Category IV.† |
| b. Category IV if there are signs of undermining of the adjacent tissue. |
| c. Category IV if there is necrosis. |
| d. Category IV if there are signs of a reduction of the supply of blood to the tissue. |
| THEME: RISK ASSESSMENT |
| 11. CASE: A patient is recently admitted to your nursing unit. The patient has no signs of skin redness (blanchable/non‐blanchable), but is bedridden. When completing the Braden risk assessment tool, the score indicates that there is no risk for pressure ulcer development. No prevention is needed. However, you are very surprised because your clinical experience tells you that this patient is at risk. What are you going to do now? |
| a. You do not implement a prevention plan because both the skin assessment and the scoring tool indicated that there is no increased risk. |
| b. You do not implement a prevention plan because risk assessment instruments are developed to replace clinical judgment. |
| c. You take preventive measures because your clinical judgment is as important as the result of the risk screening using the tool.† |
| d. You decide to reassess the patient on a daily basis (using the instrument) and to start prevention if the Braden risk assessment instrument indicates an increased risk to develop a pressure ulcer. |
| 12. Which of these statements about the frequency of skin assessment on pressure points in hospitals is correct? |
| a. The frequency of skin assessment is a medical decision (made by a medical doctor). |
| b. Skin areas with an increased risk for pressure ulcer development should be inspected at least once a week. |
| c. The skin of patients at risk should be inspected at least twice a week. |
| d. The skin of all patients should be inspected at least daily.† |
| THEME: NUTRITION |
| 13. CASE: A 23‐year‐old previously healthy male was recently admitted to the hospital with a spinal cord injury (car accident). He is immobile and has no problems eating of drinking. Is nutritional supplementation needed to reduce the risk for pressure ulcers? |
| a. Yes, I provide nutritional supplementations (vitamin tablets) to prevent pressure ulcers. |
| b. Yes, I provide nutritional supplementations (drinks enriched with the amino acid arginine) to prevent pressure ulcers. |
| c. No, I will not change the nutrition of this patient as long as no signs of pressure ulcers are observed (redness or skin breakdown). |
| d. No, I will not change the nutrition of this patient as long as nutritional intake is adequate.† |
| 14. Which nutritional elements are the most essential to prevent pressure ulcers? |
| a. Carbohydrates, fats and proteins. |
| b. Proteins and fluids.† |
| c. Carbohydrates and proteins. |
| d. Fat, fluids and protein. |
| 15. What type of patients (in terms of body weight) have an increased risk to develop pressure ulcers? |
| a. Extremely thin patients. |
| b. Obese patients. |
| c. Both extremely thin and obese patients.† |
| d. Body weight and BMI are not associated with pressure ulcer risk. |
| THEME: PREVENTION OF PRESSURE ULCERS |
| 16. What is the percentage of patients with an increased risk to develop pressure ulcers that receive adequate prevention in a chair and in bed in hospitals? |
| a. <20%.† |
| b. Between 20% and 50%. |
| c. Between 50% and 70%. |
| d. >70%. |
| 17. CASE: Your colleague informs you that she positioned a patient in bed in a semi Fowler position. What does this mean? |
| a. The patient lies on his side in an angle of 30°. |
| b. The patient lies on his side in an angle of 45°. |
| c. The patient lies in a supine position, with both head of bed and upper legs elevated up to an angle of 30°.† |
| d. The patient lies in a supine position, with the head of bed elevated up to an angle of 45°. |
| 18. Which repositioning protocol is most effective to prevent pressure ulcers? Starting with the patient supine, then… |
| a. Lateral 30 ° left – supine ‐ lateral 30 ° right – supine – lateral 30 ° left – …† |
| b. Lateral 90 ° left – supine – lateral 90 ° right – supine – lateral 90 ° left – … |
| c. Lateral 30 ° left – supine – lateral 30 ° right – supine – lateral 90 ° left – supine – lateral 90 ° right – … |
| d. Lateral 30 ° left – lateral 90 ° left – supine – lateral 30 ° right – lateral 90 ° right – supine – … |
| 19. The use of a ring cushion (donuts) is effective to prevent pressure ulcers when patients are seated in a chair of wheelchair. Is this statement correct? |
| a. Yes, because the pressure near the bony prominence is reduced. |
| b. Yes, because it redistributes pressure and shear effectively around the area at risk. |
| c. No, because the contact surface between the patient's skin and the surface is smaller.† |
| d. No, as it is only effective if a patient had a pressure ulcer in the past. |
| 20. How should bed linen be used to prevent pressure ulcers? |
| a. Do not secure the sheets under the mattress, so they can move along with the patient. |
| b.Do not secure the blanket under the mattress, so it can move along with the patient.† |
| c. Make sure the sheets are stretched tight. |
| d. Put moisture‐absorbing pads under the patient. |
| 21. Which is the most effective technique to position a patient when seated? |
| a. In an upright position with the knees in a 90° angle and the feet not touching the ground. |
| b. In an upright position with the legs being supported so that an angle of more than 90° is created at the knees. |
| c. In a semi‐reclined position with the knees in a 90° angle with the feet not touching the ground. |
| d. In a semi‐reclined position with the legs being supported so that an angle of more than 90° is created at the knees.† |
| 22. CASE: Your patient is lying on a pressure redistributing foam mattress. Do you take other measures to prevent pressure ulcers on the heels? |
| a. No. A pressure redistributing foam mattress is sufficient. |
| b. No. A pressure redistributing foam mattress combined with repositioning is sufficient. |
| c. Yes. I will place a pillow from the knee to the Achilles tendon to off‐load the heels.† |
| d. Yes. I will place a pillow under the Achilles tendon to off‐load the heels. |
| 23. How does repositioning prevent pressure ulcers? |
| a. The amount of pressure and shear will be reduced. |
| b. The amount and duration of pressure and shear will be reduced. |
| c. The duration of pressure and shear will be reduced.† |
| d. It reduces friction at the bony prominences. |
| THEME: SPECIFIC PATIENT GROUPS |
| 24. Which of these statements is correct about the development of pressure ulcers in the operating room? |
| a. Pressure ulcers are not likely to occur during surgery. If redness is observed just after surgery, it is most likely to be a burn wound. |
| b. Immobilisation after surgery causes pressure ulcers to develop, not the immobilisation during the surgery itself. |
| c. When pressure ulcers develop during surgery the first visible signs appear a few days later; making people think they developed after surgery.† |
| d. A pressure ulcer appearing postoperatively is always the result of immobilisation during surgery. |
| 25. Which is the location on the body where babies have the highest risk to develop a pressure ulcer? |
| a. Occiput.† |
| b. Heels. |
| c. Shoulders. |
| d. Sacrum. |
*The response alternative ‘e. I do not know the answer.’ has to be added to every item.
Indicates the correct answer.
Phase 2: psychometric evaluation of the tool
Validity of the multiple‐choice test items. Item difficulty: Item difficulty, expressed by a P‐value, refers to the percentage of participants who chose the correct response alternative relative to all participants 15, 17, 18. According to the table of de Gruijter and Van Berkel in Sabbe et al. 14, an item difficulty of P = 0·70 was optimal for items with five response alternatives. Items with a P‐value less than 0·10 were considered to be too difficult, and items with a P‐value greater than 0·90 were considered to be too easy.
Discriminating index: To determine the discriminating index of the items, the participants were divided into two extreme groups: the 27% best‐performing participants and the 27% worst‐performing participants. Each item should be answered correctly by the majority of the best‐performing group and the minority of the worst‐performing group. The discriminating index, expressed by a D‐value, was calculated by subtracting the percentage of correct answers in the worst‐performing group from the percentage of correct answers in the best‐performing group 14, 17. According to the table of Poelman et al. in Sabbe et al. 14, a D‐value less than 0·10 was low; between 0·10 and 0·20 was reasonable; between 0·20 and 0·30 was moderate and greater than 0·30 was good.
Quality of the response alternatives: To evaluate the quality of the response alternatives, the distribution of the incorrect answers over the response alternatives was defined. The attractiveness of the different response alternatives, expressed by an a‐value, was calculated by assessing the percentage of participants who choose each response alternative 14, 17. Sabbe et al. 14 state that the ideal a‐value for a item with five response alternatives was 0·10 and that the a‐value of the response alternatives had to be less than the percentage of correct answers for the item (P‐value). Ideally, all a‐values had to be about equal for each item so that all alternatives function as equal distracters 14.
Construct validity.
Test–retest procedure: The test–retest procedure was used to evaluate the ability of the tool to obtain consistent results when it is completed at two different moments 18. To perform the procedure, the students who had completed the tool the first time were asked to complete it a second time 10 days later 19. The stability of the tool was evaluated for each theme and for the whole tool and was represented by an intraclass correlation coefficient (ICC). A stability of ICC > 0·70 was considered sufficient, and a stability of ICC > 0·80 was preferred 20.
Known‐groups technique: The known‐groups technique was used to evaluate the ability of the tool to make a distinction between groups that are expected to have a different level of expertise 20. The participants were divided into six groups: wound care nurses, nurses responsible for the daily care of patients (bedside nurses), bedside nurses with additional education concerning pressure ulcers, bedside nurses who never completed an educational session concerning pressure ulcers, nursing students in their third year and nursing students in their first year. The scores of the groups with the (theoretically expected) higher level of expertise were compared with the scores of the groups with the (theoretically expected) lower level of expertise.
Phase 3: revision based on the psychometric evaluation
The results of the psychometric evaluation were thoroughly discussed in a meeting with experts from this research group. During this meeting, items and response alternatives were reformulated in order to enhance the validity of the PUKAT 2·0. The PUKAT 2·0 was not re‐evaluated after this revision phase.
Setting and sample
A convenience sample of 342 nurses and nursing students were invited to participate in phase 2 of the study. Students were of an undergraduate level (bachelor in nursing) or a vocational level (diploma in nursing). All students were included in the study. Only the students who were present during both data collecting time points could be included for the test–retest procedure. The nurses worked in five different settings: a general hospital, two university hospitals and two nursing homes. In each hospital, six wards were included: internal medicine, surgery, paediatrics, geriatrics, intensive care and surgery room. Only nurses who were employed in these wards were included in the study.
Procedure
This study was conducted in Belgium between April and June 2016. The students received a printed version of the knowledge assessment tool. They were asked to individually complete the tool while staying in the classroom, without consulting any resources (e.g. handbook, internet). After 10 days, the students were asked to complete the knowledge assessment tool again under the same conditions. Participants were not informed of this test–retest procedure, and no feedback was given. The nurses received a direct link to the knowledge assessment tool via email. They were explicitly asked to complete the tool individually and without any resources.
Analysis of the data
Statistical analyses were performed using SPSS 23·0 (SPSS inc. Headquarters, Chicago, IL). Questionnaires were excluded in case of three or more missing answers or if the option ‘I do not know the answer’ was marked 24 or 25 times. All results were coded as dichotomous variables: correct (1) and not correct (0). The result was coded as not correct if the option ‘I do not know the answer’, multiple answers or no answer was marked. The total score of each participant was calculated as the sum of correct answers. The stability of the tool was determined by calculating the ICC. The known‐groups technique was analysed using the independent sample t‐test. The significance level was set as P < 0·05.
Ethical considerations
This study was approved by the Ethics Committee of the University Hospital of Ghent (B/670201526630) in consultation with the Ethics Committees of the other participating hospitals. The Belgian experts, the participants of the pilot study, the nursing students and the nurses who participated in the study received and signed an informed consent. Personal data about the participants was encrypted.
Results
Characteristics of the participants
In total, 228 nurses and 114 nursing students participated in the study (n = 342). Of all participating nurses, 55·3% had a bachelor degree, and 21% had a diploma degree. Of all the nurses with a bachelor degree, 53.5% were general registered nurses, without being specialised in a specific area (e.g. mental health). Diploma degree nurses did not have training at a professional bachelor level but had a post‐qualification at secondary school level. Of the nurses, 86% worked in a hospital and 14% in a nursing home. More than half of the nurses was older than 35 years (57·9%) and had more than 10 years of professional experience (55·7%). Half of the nurses did not complete any training focusing on pressure ulcers, but 68% expressed the need to complete a course. Of all participating students, 62·3% followed the bachelor program and 37.7% followed the diploma program. An overview of the characteristics of all participants is provided in Table 2. The total score on the tool for the nurses varied between 5 and 22, with an average score of 13 of a maximum of 25 (SD = 3.03). The total score on the tool for the students varied between 1 and 17, with an average score of 9·63 of a maximum of 25 (SD = 3.89). The response rate of the nurses in the 20 participating wards varied between 0% and 100%, with an average response rate of 41·8%. The students completed the knowledge tool in a classroom. As a consequence, the response rate was 100%.
Table 2.
Characteristics of the participants
| Students (n = 114) | Nurses (n = 228) | |
|---|---|---|
| % (n) | % (n) | |
| Gender (% female) | 84.2% (96) | 85·1% (194) |
| Education | ||
| Diploma in nursing | 37·7% (43) | 21% (48) |
| Bachelor in nursing | 62·3% (71) | 55·3% (126) |
| Bachelor nurse with specialisation (e.g. mental health) | na | 13·6% (31) |
| Master of Science in Nursing | na | 10·1% (23) |
| Age category | ||
| <25 years | 78·1% (89) | 9·6% (22) |
| 25–34 years | 14% (16) | 32·5% (74) |
| 35–50 years | 7·9% (9) | 37·3% (85) |
| >50 years | 0% (0) | 20·6% (47) |
| Year of education | ||
| Student 1st year | 62·3% (71) | na |
| Student 2nd year | 14% (16) | na |
| Student 3rd year | 23·7% (27) | na |
| Master | na | 2·6% (6) |
| Specialisation | ||
| General nursing | 53·5% (61) | 52·6% (120) |
| Geriatrics | 0% (0) | 5·7% (13) |
| Paediatrics | 0·9% (1) | 13·2% (30) |
| Emergency and intensive care | 0% (0) | 14·9% (34) |
| Surgery room | 0·9% (1) | 3·1% (7) |
| Wound care | 0% (0) | 1·3% (3) |
| Other | 10·5% (12) | 9·2% (21) |
| Missing | 34·2%(39) | 0% (0) |
| Sector employment | ||
| General hospital | 0% (0) | 44·3% (101) |
| University hospital | 0·9% (1) | 41·7% (95) |
| Nursing home | 0·9% (1) | 14% (32) |
| Ward | ||
| Geriatrics | 1·8% (2) | 32·5% (74) |
| Surgery | 0·9% (1) | 14·9% (34) |
| Internal medicine | 0% (0) | 11·4% (26) |
| Paediatrics | 0% (0) | 13·6% (31) |
| Surgery room | 0% (0) | 8·3% (19) |
| Intensive care | 0% (0) | 16·7% (38) |
| Other | 0% (0) | 2·6% (6) |
| Role | ||
| Nurse | 5·3% (6) | 92·5% (211) |
| Senior nurse | na | 5·3% (12) |
| Specialist nurse in wound care | na | 2·2% (5) |
| Work experience | ||
| <5 years | 4·4 % (5) | 26·3% (60) |
| 5–10 years | 2·6% (3) | 18% (41) |
| 10–20 years | 2·6% (3) | 20·6% (47) |
| >20 years | 0% (0) | 35·1% (80) |
| Work regime | ||
| <50% | 0·9% (1) | 1·3% (3) |
| 50–75% | 0·9% (1) | 17·1% (39) |
| >75% | 2·6% (3) | 81·6% (186) |
| Last PU training? | ||
| <1 years | 1·8% (2) | 11·8% (27) |
| 1–2 years | 0% (0) | 14·5% (33) |
| 2–5 years | 1·8% (2) | 11·85% (27) |
| >5 years | 0% (0) | 11·85% (27) |
| never | 92·1% (105) | 50% (114) |
| Need PU training? | ||
| Yes | 44·7% (51) | 68% (155) |
| No | 44·7% (51) | 32% (73) |
na, not applicable.
Psychometric evaluation of the tool
Validity of the multiple‐choice test items
Item difficulty.
For 23 items, the item difficulty (P‐value) varied between 0·25 and 0·83, with an average of 0·56. One item (item 12) was found to be too easy (0·91), and one (item 20) was too difficult (0·12). An overview is provided in Table 3.
Table 3.
Validity of the multiple‐choice test items and stability
| Domains | Items | Proportion of respondents choosing each response alternative* (= a‐value for incorrect response alternatives) | Item difficulty (P‐value‡) | Discriminating index (D‐value) | Stability (ICC, 95% CI, P‐value) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Response alternatives | |||||||||
| a | b | c | d | Do not know | |||||
| Aetiology | 1 | 0·16 | 0·01 | 0·01 | 0·83† | 0·03 | 0·83 | 0·15 | |
| 2 | 0·17 | 0·03 | 0·29† | 0·51 | 0·03 | 0·29 | 0·20 | ||
| 3 | 0·04 | 0·20 | 0·44† | 0·32 | 0·25 | 0·44 | 0·10 | 0·52 (0·21‐0·71, P = 0·002) | |
| 4 | 0·02 | 0·44† | 0·53 | 0·01 | 0·24 | 0·44 | 0·03 | ||
| 5 | 0·06 | 0·07 | 0·25 | 0·62† | 0·07 | 0·62 | 0·22 | ||
| 6 | 0·09 | 0·43† | 0·29 | 0·19 | 0·17 | 0·43 | 0·16 | ||
| Classification and observation | 7 | 0·10 | 0·39 | 0·12 | 0·39† | 0·35 | 0·39 | 0·09 | |
| 8 | 0·13 | 0·82† | 0·02 | 0·03 | 0·03 | 0·82 | 0·14 | 0·57 (0·30–0·74, P < 0·000) | |
| 9 | 0·01 | 0·11 | 0·58† | 0·30 | 0·23 | 0·58 | 0·30 | ||
| 10 | 0·69† | 0·08 | 0·17 | 0·07 | 0·21 | 0·69 | 0·24 | ||
| Risk assessment | 11 | 0·01 | 0·01 | 0·60† | 0·39 | 0·06 | 0·60 | 0·26 | 0·52 (0·20–0·70, P = 0·002) |
| 12 | 0·0 | 0·03 | 0·06 | 0·91† | 0·06 | 0·91 | 0·17 | ||
| Nutrition | 13 | 0·05 | 0·07 | 0·18 | 0·70† | 0·13 | 0·70 | 0·22 | |
| 14 | 0·17 | 0·53† | 0·18 | 0·12 | 0·09 | 0·53 | 0·17 | 0·26 (−0·22–0·55, P = 0·120) | |
| 15 | 0·09 | 0·01 | 0·59† | 0·31 | 0·04 | 0·59 | 0·10 | ||
| Prevention | 16 | 0·25† | 0·39 | 0·23 | 0·12 | 0·34 | 0·25 | 0·05 | |
| 17 | 0·09 | 0·01 | 0·77† | 0·13 | 0·15 | 0·77 | 0·27 | ||
| 18 | 0·67† | 0·09 | 0·15 | 0·09 | 0·33 | 0·67 | 0·26 | ||
| 19 | 0·17 | 0·20 | 0·57† | 0·06 | 0·25 | 0·57 | 0·34 | 0·40 (0·01–0·63, P = 0·022) | |
| 20 | 0·16 | 0·12† | 0·70 | 0·02 | 0·05 | 0·12 | 0·02 | ||
| 21 | 0·11 | 0·41 | 0·11 | 0·36† | 0·23 | 0·36 | 0·16 | ||
| 22 | 0·06 | 0·21 | 0·57† | 0·16 | 0·12 | 0·57 | 0·25 | ||
| 23 | 0·05 | 0·45 | 0·48† | 0·02 | 0·03 | 0·48 | 0·20 | ||
| Specific patient groups | 24 | 0·05 | 0·15 | 0·56† | 0·24 | 0·33 | 0·56 | 0·19 | −0·03 (−0·69–0·37, P = 0·560) |
| 25 | 0·80† | 0·03 | 0·03 | 0·14 | 0·11 | 0·80 | 0·20 | ||
Based on the proportion of participants who did NOT choose the ‘I do not know’ option.
Correct answer.
This P‐value expresses the proportion of participants who answered the item correctly.
Discriminating index.
The discriminating index (D‐value) varied between 0·02 and 0·34. The D‐value was low for four items, reasonable for nine items, moderate for nine items and good for three items. An overview is provided in Table 3.
Quality of the response alternatives.
The quality of the response alternatives (a‐value) varied between 0·01 and 0·70, with an average of 0·16. A third of the alternatives had a‐value between 0·05 and 0·14 and could be considered an ideal response alternative. An overview is provided in Table 3.
Construct validity
Test–retest procedure.
The stability of the tool was evaluated using a test–retest procedure. The retest was completed by 65 students 10 days after the first test. An overall ICC of 0·69 was found (95% CI 0·49–0·81, P < 0·01). The ICC for the different themes varied between −0·03 (P = 0·56) and 0·57 (P < 0·00). An overview is provided in Table 3.
Known‐groups technique.
The participants were divided in six groups with different expected levels of expertise. The scores of the different groups were compared. The knowledge assessment tool was able to demonstrate a significant difference between all predefined groups. An overview is provided in Table 4.
Table 4.
Known‐groups technique
| Groups | n | Average scores (SD) | Significance (P‐value) |
|---|---|---|---|
| Specialist nurse in wound care* (H) | 5 | 16·80 (3·56) | 0·004 |
| versus bedside nurses† (L) | 206 | 12·89 (2·93) | |
| Specialist nurse in wound care* (H) | 5 | 16·80 (3·56) | <0·001 |
| versus students first year (L) | 71 | 7·79 (3·45) | |
| Bedside nurses† (H) | 206 | 12·89 (2·93) | <0·001 |
| versus students first year (L) | 71 | 7·79 (3·45) | |
| Students third year (H) | 27 | 12·56 (2·38) | <0·001 |
| versus students first year (L) | 71 | 7·79 (3·45) | |
| Bedside nurses with training‡ (H) | 97 | 13·33 (2·64) | 0·043 |
| versus bedside nurses without training§ (L) | 109 | 12·50 (3·13) |
(H), group with theoretically expected higher level of expertise; (L), group with theoretically expected lower level of expertise
Nurses specialised in wound care or pressure ulcer care.
Nurses responsible for the daily care of patients.
Bedside nurses who completed training about pressure ulcers.
Bedside nurses who never completed training about pressure ulcers.
Discussion
The aim of this study was to develop PUKAT 2·0, a valid, reliable and up‐to‐date tool, to measure the knowledge of nurses and nursing students on pressure ulcer prevention. The new knowledge assessment tool consisted of 25 multiple‐choice items, categorised into six themes, covering the most relevant aspects of pressure ulcer prevention.
The PUKAT 2·0 was an update of the PUKAT 7, published in 2010, and one of the most commonly used pressure ulcer knowledge assessment tools. The PUKAT was used for research in Sweden 8, 21, the UK 22 and Italy 9 to assess knowledge of nurses and nursing students. Furthermore, it was also translated into Turkish 10 and Chinese 11. Besides the PUKAT, various other knowledge assessment tools have been developed internationally. However, these tools were characterised by a limited evaluation of psychometric properties. For example, Tweed et al. 23, Strand et al. 24 and Saleh et al. 25 developed tools for research purposes, which were only pilot studied and reviewed by experts. Another knowledge assessment tool, often mentioned in literature, is the Pieper–Zulkowski Pressure Ulcer Knowledge Test (PZ‐PUKT) 26. The PZ‐PUKT consisted of 72 true or false questions, categorised in three themes: prevention, classification and wound description. Content validity, internal consistency and reliability were evaluated. However, evaluation of the stability of the tool, as well as evaluation of the quality of the multiple‐choice items, were lacking 26. The PZ‐PUKT was also used in a modified version by Chianca et al. 27, Ilesanmi et al. 28 and Lawrence et al. 29 without re‐evaluating the psychometric properties. The use of an unmodified version of the PUKAT 2·0 is essential to obtain valid and comparable results.
To our knowledge, the PUKAT 2·0 is the most up‐to‐date knowledge assessment tool on pressure ulcer prevention. All items of the tool were formulated according the most recent evidence‐based guidelines for pressure ulcer prevention 1, 6, 12. In addition, cases and pictures were added to evaluate theoretical knowledge as well as practical knowledge. The PUKAT 2·0 can be used to evaluate the knowledge of nurses and nursing students concerning the most recent recommendations on pressure ulcer prevention.
In comparison to other pressure ulcer knowledge assessment tools, the psychometric properties of the PUKAT 2·0 were evaluated rigorously. The psychometric evaluation included the evaluation of the multiple‐choice items, discriminating index, quality of the response alternatives, stability as well as construct validity. Overall values for item difficulty were good, but one item was found to be too easy (item 12) and one item too difficult (item 20). Item 12 was not adapted because the experts agreed that the frequency of skin assessment is an important aspect of pressure ulcer prevention, and the formulation could not be changed without losing clarity. Concerning item 20, the experts decided to modify the response alternatives in order to reduce confusion and to improve the D‐value (discrimination index), which was also low for this item. Analysis of the quality of the response alternatives revealed that most items contained at least one response alternative with an a‐value less than 0·10, which was too low. The experts thoroughly discussed the consequences of changing these response alternatives and agreed to change the response alternatives of item 1, 15 and 17.
Other response alternatives were not changed because it was reasonable to expect that the lower values were mainly because of a lack of knowledge of the participants. Changing these items could restrict the possibility of distinguishing between different levels of knowledge. As a result, the validity of our tool was further enhanced.
It should be noticed that the internal consistency, which is often evaluated in questionnaires, was not assessed in our study. Research determined that two measurement models can be distinguished in the development of measurement tools: the effect indicator model and the causal indicator model. As this study relates to a measurement model in which the items determine the construct (causal indicator model), the concept of internal consistency is not applicable on our knowledge assessment tool 30.
Despite the fact that PUKAT 2·0 was only developed and tested in Belgium, it was completed by nurses and nursing students with a wide variety of profiles and from different levels of education during the validation process. This allows the knowledge tool to be widely applicable. However, to evaluate a higher level of knowledge (e.g. wound care nurses or experts) or the knowledge of other persons involved in pressure ulcer prevention (e.g. patients and/or family caregivers), a tailored tool should be developed and validated.
The PUKAT 2·0 can be used to evaluate individual knowledge of nurses and nursing students (e.g. before and/or after training or after consulting the guidelines). Providing feedback for incorrect and even correct response alternatives will add an educational dimension to the knowledge assessment tool. In addition, the tool can be applied as part of an implementation project. We decided not to determine an overall cut‐off value indicating sufficient knowledge on pressure ulcer prevention. It is rather recommended for nurses and nursing students to possess knowledge regarding all six domains included in this tool, which was content validated by experts. The results obtained on the separate themes of the PUKAT 2·0 are particularly useful to determine educational needs and priorities and to set up tailored education. For these purposes, the tool can be used in education, research and practice.
Limitations of the study
Worldwide knowledge and insights regarding the prevention of pressure ulcers continue to evolve. As a consequence, regular updates of the PUKAT 2·0 will have to be performed and disseminated.
The measure of the knowledge of nurses and nursing students is a snapshot. Knowledge is not stable; it is continuously affected by daily experiences and learning opportunities. This has to be taken in account when evaluating the stability of the tool.
Conclusion
The PUKAT 2·0 is a revised and updated version of the Pressure Ulcer Knowledge Assessment Tool (PUKAT) developed in 2010 at Ghent University, Belgium. The updated version was developed using state‐of‐the‐art techniques to establish evidence about validity and reliability. The tool consists of 25 multiple‐choice items within six themes covering the most relevant aspects of pressure ulcer prevention. Different types of validity were evaluated: the level of difficulty was decent, the validity content was good and the ability to discern was good. The PUKAT 2·0 demonstrated good psychometric properties and can be used and disseminated internationally to assess knowledge about pressure ulcer prevention in nursing education, research and practice.
Acknowledgements
We would like to thank the experts from the European Pressure Ulcer Advisory Panel (EPUAP) and the National Pressure Ulcer Advisory Panel (NPUAP) and the participants of the pilot study for their valuable contribution to the development of the tool. We also would like to address a special thanks to all the nurses and nursing students who filled in the tool and provided the data to validate PUKAT 2·0.
References
- 1. Beeckman D, Matheï C, Van Lancker A, Van Houdt S, Vanwalleghem G, Gryson L, Heyman H, Thyse C, Toppets A, Stordeur S, Van den Heede K. Een nationale richtlijn voor decubituspreventie. Brussels: Belgian Health Care Knowledge Centre (KCE), 2012. [Google Scholar]
- 2. Briggs M, Collinson L, Wilson L, Rivers C, McGinnis E, Dealey C, Brown J, Coleman S, Stubbs N, Stevenson R, Nelson A, Nixon J. The prevalence of pain at pressure areas and pressure ulcers in hospitalised patients. BMC Nurs 2013;12:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bredesen I, Bjøro K, Gunningberg L, Hofoss D. The prevalence, prevention and multilevel variance of pressure ulcers in Norwegian hospitals: a cross‐sectional study. Int J Nurs Stud 2015;52:149–56. [DOI] [PubMed] [Google Scholar]
- 4. Beeckman D, Defloor T, Schoonhoven L, Vanderwee K. Knowledge and attitudes of nurses on pressure ulcer prevention: a cross‐sectional multicenter study in Belgian hospitals. Worldviews Evid Based Nurs 2011;8:166–76. [DOI] [PubMed] [Google Scholar]
- 5. Vanderwee K, Defloor T, Beeckman D, Demarre L, Verhaeghe S, Van Durme T, Gobert M. Assessing the adequacy of pressure ulcer prevention in hospitals: a nationwide prevalence survey. BMJ Quality Safety 2011;20:260–7. [DOI] [PubMed] [Google Scholar]
- 6. National Pressure Ulcer Advisory Panel (NPUAP) , European Pressure Ulcer Advisory Panel (EPUAP) , Pan Pacific Pressure Injury Alliance (PPPIA) . Prevention and treatment of pressure ulcers: clinical practice guideline, 2nd edn. Perth: Cambridge media, 2014. [Google Scholar]
- 7. Beeckman D, Vanderwee K, Demarré L, Paquay L, Van Hecke A, Defloor T. Pressure ulcer prevention: development and psychometric validation of a knowledge assessment instrument. Int J Nurs Stud 2010;47:399–410. [DOI] [PubMed] [Google Scholar]
- 8. Gunningberg L, Mårtensson G, Mamhidir A, Florin J, Athlin ÅM, Bååth C. Pressure ulcer knowledge of registered nurses, assistant nurses and student nurses: a descriptive, comparative multicentre study in Sweden. Int Wound J 2015;12:462–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Simonetti V, Comparcini D, Flacco ME, Di Giovanni P, Cicolini G. Nursing students' knowledge and attitude on pressure ulcer prevention evidence‐based guidelines: a multicenter cross‐sectional study. Nurse Educ Today 2015;35:573–9. [DOI] [PubMed] [Google Scholar]
- 10. Tulek Z, Polat C, Ozkan I, Theofanidis D, Togrol RE. Validity and reliability of the Turkish version of the pressure ulcer prevention knowledge assessment instrument. J Tissue Viability 2016;25:201–8. [DOI] [PubMed] [Google Scholar]
- 11. Liu M, Yuan H, Chen W, Poon C, Hsu M, Zhang B. Translation, modification and validation of the Chinese version of a knowledge assessment instrument regarding pressure ulcer prevention. Chinese Nurs Res 2016;3:16–23. [Google Scholar]
- 12. National Institute for Health Care Excellence (NICE) . Pressure ulcers: prevention and management of pressure ulcers. United Kingdom: 2014, NICE clinical guideline 179. [PubMed]
- 13. Mishel MH. Methodological studies: instrument development. In: Brink PJ, Wood MJ, editors. Advanced Design in Nursing Research, 2nd edn. California: Sage Publications, 1998:235–70. [Google Scholar]
- 14. Sabbe E, Lesage E. Meerkeuzetoetsen: praktische handleiding voor leerkrachten en docenten. Garant‐uitgevers: Antwerpen, 2012. [Google Scholar]
- 15. Haladyna TM, Downing SM, Rodriguez MC. A review of multiple‐choice item‐writing guidelines for classroom assessment. Appl Meas Educ 2002;15:27. [Google Scholar]
- 16. de Gruijter DNM. Toetsing en toetsanalyse, herziene versie. Nederland: 2008. URL http://media.leidenuniv.nl/legacy/toetsing‐en‐toetsanalyse.pdf (accessed on 02 February 2016).
- 17. Tavakol M, Dennick R. Post‐examination analysis of objective tests. Med Teach 2011;33:447–58. [DOI] [PubMed] [Google Scholar]
- 18. Field A. Discovering Statistics using SPSS (and Sex and Drugs and Rock ‘n’ Roll), 3rd edn. London: Sage Publications, 2009. [Google Scholar]
- 19. Marx RG, Menezes A, Horovitz L, Jones EC, Warren RF. A comparison of two time intervals for test‐retest reliability of health status instruments. J Clin Epidemiol 2003;56:730–5. [DOI] [PubMed] [Google Scholar]
- 20. Polit DF, Beck CT. Nursing Research: Appraising Evidence for Nursing Practice, 7th edn. Philadelphia: Lippincott Williams & Wilkins, 2010. [Google Scholar]
- 21. Sving E, Högman M, Mamhidir A, Gunningberg L. Getting evidence‐based pressure ulcer prevention into practice: a multi‐faceted unit‐tailored intervention in a hospital setting. Int Wound J 2016;13:645–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clarkson P, Bader D, Schoonhoven L, Worsley P. A multidisciplinary approach to pressure ulcer prevention: exploring healthcare professsionals' knowledge and attitudes to pressure ulcer prevention in the community. Physiotherapy 2016;102:256–7.26597694 [Google Scholar]
- 23. Tweed C, Tweed M. Intensive care nurses' knowledge of pressure ulcers: development of an assessment tool and effect of an educational program. Am J Crit Care 2008;17:338–46. [PubMed] [Google Scholar]
- 24. Strand T, Lindgren M. Knowledge, attitudes and barriers towards prevention of pressure ulcers in intensive care units: a descriptive cross‐sectional study. Intensive Crit Care Nurs 2010;26:335–42. [DOI] [PubMed] [Google Scholar]
- 25. Saleh MYN, Al‐Hussami M, Anthony D. Pressure ulcer prevention and treatment knowledge of Jordanian nurses. J Tissue Viability 2013;22:1–11. [DOI] [PubMed] [Google Scholar]
- 26. Pieper B, Zulkowski K. The Pieper‐Zulkowski pressure ulcer knowledge test. Adv Skin Wound Care 2014;27:413–9. [DOI] [PubMed] [Google Scholar]
- 27. Chianca TCM, Rezende JFP, Borges EL, Nogueira VL, Larcher MH. Pressure ulcer knowledge among nurses in a brazilian university hospital. Ostomy Wound Manage 2010;56:58–64. [PubMed] [Google Scholar]
- 28. Ilesanmi RE, Ofi BA, Adejumo PO. Nurses' knowledge of pressure ulcer prevention in Ogun State, Nigeria: results of a pilot survey. Ostomy Wound Manage 2012;58:24–32. [PubMed] [Google Scholar]
- 29. Lawrence P, Fulbrook P, Miles S. A survey of Autralian nurses' knowledge of pressure injury/pressure ulcer management. J Wound Ostomy Continence Nurs 2015;42:450–60. [DOI] [PubMed] [Google Scholar]
- 30. Knotter J, Streiner DL. Internal consistency and Cronbach's α: a comment on Beeckman et al. (2010). Int J Nurs Stud 2010;47:926–8. [DOI] [PubMed] [Google Scholar]


