Abstract
‘Hard‐to‐heal’ wounds are those which fail to heal with standard therapy in an orderly and timely manner and may warrant the use of advanced treatments such as non‐contact low‐frequency ultrasound (NLFU) therapy. This evaluator‐blinded, single‐site, randomised controlled trial, compared NLFU in addition to UK standard of care [SOC: (NLFU + SOC)] three times a week, with SOC alone at least once a week. Patients with chronic venous leg ulcers were eligible to participate. All 36 randomised patients completed treatment (17 NLFU + SOC, 19 SOC), and baseline demographics were comparable between groups. NLFU + SOC patients showed a −47% (SD: 38%) change in wound area; SOC, −39% (38%) change; and difference, −7·4% [95% confidence intervals (CIs) −33·4–18·6; P = 0·565]. The median number of infections per patient was two in both arms of the study and change in quality of life (QoL) scores was not significant (P = 0·490). NLFU + SOC patients reported a substantial mean (SD) reduction in pain score of −14·4 (14·9) points, SOC patients' pain scores reduced by −5·3 (14·8); the difference was −9·1 (P = 0·078). Results demonstrated the importance of high‐quality wound care. Outcome measures favoured NLFU + SOC over SOC, but the differences were not statistically significant. A larger sample size and longer follow‐up may reveal NLFU‐related improvements not identified in this study.
Keywords: Compression, Quality of life, Ultrasound therapy, Venous leg ulcers, Wound healing
Introduction
Vascular ulcers (e.g. venous and arterial ulcers), diabetic ulcers and pressure ulcers are classified as chronic wounds. The scale of the problem of these wounds is huge and well documented. Chronic wounds display characteristics such as a prolonged inflammatory phase, persistent infections, formation of microbial biofilms and ineffective dermal/epidermal cell response, which differentiate them from acute wounds 1. However, if appropriate ‘standard of care’ (SOC) 2 is initiated in a timely manner such chronic wounds can often follow a normal healing trajectory. Troxler et al. introduces the term ‘hard‐to‐heal’ which better explains a wound which fails to heal with standard therapy in an orderly and timely manner 3. Decades of research has led to a greater understanding of the complex pathophysiology of chronic wounds, raising many further questions in the process 4.
Chronic leg ulceration prevalence in the UK is estimated to be 1%, with between 0·12% and 0·32% of the population having an open ulcer 5. Venous leg ulcers (VLUs) become more common with age, and many patients suffer from the condition for a number of years 6. Patients with VLUs have a substantially poorer quality of life (QoL) which is often because of the pain, odour, recurrent wound infection and reduced mobility associated with chronic leg ulceration 7. The cost for treating unhealed venous ulceration in 2005/2006 to the NHS was at least £168 million/year 8. Tennvall and Hjelmgen (2005) 9 showed that the average total cost per patient for treating a VLU for 52 weeks in the UK ranged from €1121 to 2142 depending on size and duration of the wound. When a patient fails to respond to standard care treatments, to reduce the long‐term impact on the patients along with the huge resources and costs incurred, advanced treatments may be considered. Advanced treatments, for example cell‐based therapies or non‐contact low‐frequency ultrasound (NLFU) therapy, have been shown in small‐scale studies to initiate healing which more traditional dressings have failed to do (10–12).
MIST Therapy System (Celleration Inc., Eden Prairie, MN) is a low‐intensity (0·1–0·8 W/cm2), NLFU device designed to promote the healing of chronic wounds. The device delivers continuous ultrasound energy (40‐kHz frequency) through a fine saline mist to the wound bed 13. It is claimed that sound waves stimulate the cells within and below the wound bed to promote wound healing through downregulation of inflammation, a reduction in the number of bacteria and an increase in blood flow 14.
In 2011, the National Institute for Health and Care Excellence (NICE, formerly National Institute for Health and Clinical Excellence) issued medical technologies guidance (MTG5) 15 which stated that NLFU shows “potential to enhance the healing of chronic, ‘hard‐to‐heal’, complex wounds, compared with standard methods of wound management”. The NICE committee noted that the quality of the evidence was limited by small patient numbers and lack of appropriate comparison groups. NICE's published guidance recommended comparative research in the UK to reduce uncertainty about the outcomes of patients with chronic wounds treated with NLFU therapy compared with those given only with standard care.
At the time of this study, randomised controlled trials had been carried out in patients with ischaemic limbs 16 and patients with diabetic foot ulcers 10 treated using NLFU therapy; since then a study on patients with VLUs has been published 17 and a pilot study 18. These randomised controlled trials 10, 16, 17 and several observational studies (mostly retrospective; 12, 19–23) have reported that treatment with NLFU improves wound healing. Kavros reported that significantly more patients with ischaemic wounds treated with NLFU achieved 50% wound closure at 12 weeks compared with those of SOC alone (63% versus 29%; P < 0·001). Ennis et al. reported no significant difference in the number of diabetic foot ulcers healed after 12 weeks of NLFU or SOC (26% versus 22%; P = 0·69) by intention to treat analysis; but a significant difference (40·7% versus 14·3%; P = 0·0366) from ‘per‐protocol’ analysis. Extrapolating the results from Ennis et al. 10, 24 into a US‐based cost model revealed savings of 19·5% from NLFU compared with SOC 25. Olyaie et al. 17 found a statistically significant difference (P = 0·04) in VLU sizes after 4 months of treatment across three groups (standard compression therapy, NLFU and high‐frequency ultrasound); although these patients were young (mean age of 39) and may not have been ‘hard‐to‐heal’ (>4‐week duration). Methodological limitations, reporting issues and aetiological heterogeneity of the study wounds have made results from previous clinical trials difficult to interpret.
Our study is an integral part of NICE's medical technologies evaluation activities – to facilitate the development of further evidence stemming from recommendations in published guidance. Coupled with the fact that there is limited high‐quality evidence on patients with VLUs treated with NLFU, this study has been designed to answer a specific research question posed by NICE: what is the utility of NLFU (as per the manufacturer's instructions for use) in the UK healthcare system compared with standard care for VLUs? The primary objective, based on the outcome measures defined in the medical technologies guidance scope 26, was to test whether there would be a difference in the change in wound area of chronic venous leg ulcers treated for 8 weeks with NLFU plus SOC compared with SOC alone.
Methods
Ethics
The trial protocol was approved by the South East Wales Research Ethics Committee (12/WA/0133) and conducted in accordance with the principles of Good Clinical Practice and in accordance with the 1975 Declaration of Helsinki. All patients provided written consent after receiving written information and prior to the commencement of trial procedures (ISRCTN 24438635; NCT01671748).
Study design and patient population
This study was a UK‐based, single‐centre, assessor‐blinded, randomised, controlled trial designed to show superiority. No substantial amendments were made to the trial protocol after commencement of the study. Adults with chronic venous leg ulcers (≥6‐week and ≤5‐year durations, and between 5 and 100 cm2 area at randomisation) and an ankle brachial pressure index (ABPI) of >0·8 were eligible to participate.
Exclusion criteria were as follows:
Uncontrolled diabetes [haemoglobin A1c (HbA1c) ≥12% in the last 3 months]
Index ulcer has active infection on day of inclusion requiring systemic antibiotic therapy
Renal failure
Exposed tendon, ligament, muscle or bone in the index ulcer
Osteomyelitis, cellulitis or gangrene in study limb
Subjects with an amputation above transmetatarsal in study limb
Active malignancy affecting study limb
Index ulcer is of arterial aetiology
Pregnant or breast feeding women or women of child‐bearing potential not willing to use a method of highly effective contraception for the duration of the study
Planned vascular surgery, angioplasty or thrombolysis procedures during study period. Or patients who are within 6 weeks of having had such a procedure
Planned surgical procedure during study period for the index wound
Prior skin replacement, negative‐pressure therapy and ultrasound therapy to the study wound in the 2 weeks before screening
Currently receiving or has received radio or chemotherapy within 3 months of randomisation
Index wound would require ultrasound near an electronic implant or prosthesis
Not capable of providing informed consent
Currently enrolled in or has been enrolled in another investigation device or drug trial in the last 30 days.
Patients whose wounds reduced by >40% during the first 4 weeks (run in phase where SOC only was administered) were withdrawn and did not progress to randomisation. This run‐in phase selected for wounds which were ‘hard‐to‐heal’ and also standardised the care provided to patients as they had been recruited from a variety of settings. Standard of care for the treatment of venous leg ulcers was compression therapy with a low adherent dressing in contact with the wound in accordance with the NICE pathway for treatment of a patient with a venous leg ulcer (2012).
Study procedures and assessments
Study procedures took place in a single dedicated unit specialising in wound healing research, between August 2012 and November 2013. All enrolled patients received 4 weeks of SOC prior to random allocation (run‐in phase, Figure 1). SOC comprised clinic visits once a week in which the wound was bathed, sharp debridement was performed if necessary, and non‐adherent dressing was applied with compression delivering 40−60 mmHg at the ankle. More frequent visits were arranged if deemed clinically necessary, for example, owing to highly exudating wound or evidence of infection. Following random allocation, patients either continued with SOC (as described previously) for eight further weeks or received NLFU therapy combined with SOC (NLFU + SOC; Figure 1).
Figure 1.
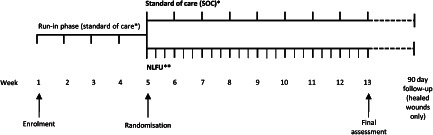
Study design flow diagram. NLFU, non‐contact low‐frequency ultrasound; SOC, standard of care. *Compression therapy and dressing change (with debridement if clinically necessary) at least once a week; wound assessments weekly. **Ultrasound therapy, with compression and dressing change (with debridement if clinically necessary) three times a week; wound assessments weekly.
NLFU consisted of the application of MIST ultrasound therapy (Celleration Inc.) to a clean wound bed for between 3 and 12 minutes (depending on the wound area) three times a week; a non‐adherent dressing and strong compression therapy was applied after NLFU application (three times a week).
Wounds were assessed once a week for 12 weeks (4‐week run‐in phase plus 8‐week treatment phase) and a final visit on week 13. Assessments comprised of a wound measurement using a Silhouette Star (ARANZ Medical, Christchurch, New Zealand) digital imaging device, pain scoring [visual analogue score (VAS) from 0 to 100], and condition of wound bed and peri‐ulcer skin, digital photography, and presence of malodour. Wound margins were traced on the imaging device by a single, blinded assessor to obtain area measurements during the treatment phase. The nature and the frequency of all adverse events (AEs) were recorded. On the first and final visits, participants were invited to complete a Cardiff Wound Impact Schedule (CWIS), a validated questionnaire designed to measure the impact of chronic wounds on patient health‐related quality of life (HRQoL) 27. The questionnaire consists of three domains: (i) physical symptoms and daily living; (ii) social life; (iii) well‐being, (transformed to a score of between 0 and 100 for each domain). The patient also provides a global HRQoL score and satisfaction with HRQoL (each scored between 0 and 10).
All researchers providing treatment with SOC or NLFU + SOC, and those assessing the wound were experienced wound healing clinicians and trained appropriately to use the NLFU device before the study started. Only patients whose index wounds were healed by the final study visit were interviewed by telephone 90 days later to determine whether their index wound remained healed.
Outcome measures
The primary outcome was the change in wound area from baseline (week 5) to week 13 (or the point of healing) controlling for the baseline wound area measurement, as determined by weekly digital wound measurements with blinded assessment of wound margin. Secondary outcomes were change in HRQoL from enrolment to week 13 (or point of healing), incidence of clinical infection, pain (VAS), and wound characteristics (e.g. odour, exudate, wound bed characteristics). The proportion of healed wounds that remained closed 90 days later was recorded.
Sample size calculation
The study was powered to detect a difference in the change in wound area of 20% between the two arms with a two‐sided significance level and power of 90%. A standard deviation of 17·5% came from published literature 12. A minimum of 17 patients in each arm was required, and with an anticipated withdrawal rate of 15%, our aim was to recruit 40 patients, or enough participants to meet the sample size. Higher than anticipated withdrawal rates prior to random allocation meant that a total of 47 patients were recruited to reach the minimum number of patients in each arm of the study as determined by the power calculation.
Randomised allocation and assessor blinding
Following the four‐week run‐in phase, patients were allocated to SOC or NLFU + SOC using an off‐site telephone service where staff had no clinical involvement in the trial and were not involved in the recruitment process. Patients were assigned using a minimisation programme (MINIM) 28 to minimise the imbalance on two prognostic factors (wound area and wound duration) between the two arms of the trial. Both factors were unweighted and had two categories (area group 1: ≥5 and ≤10 cm2; area group 2: >10 and ≤100 cm2; duration group 1: ≥ 6 weeks and <12 months; and duration group 2: ≥ 12 months and ≤5 years). To reduce the possibility of selection bias, MINIM is not entirely deterministic but is approximately 70% to the preferred allocation. To further reduce the risk of allocation prediction, the investigators were blind to the cut‐off values for each category, and the allocation was only provided once the patient details had been irreversibly entered into MINIM. Patients and clinicians providing care were aware of the treatment allocation. A single primary outcome assessor blind to treatment allocation traced the wound boundary of each weekly wound measurement using the Silhouette Star system.
Statistical analysis
All randomised patients were included in the intention‐to‐treat population. Continuous data were checked for normality using Kolmogorov–Smirnov, z‐scores for skewness and kurtosis, visual inspection of box‐plots and histograms; SOC and NLFU + SOC data were also checked for homogeneity of variance using the Levene's test. Where data were normally distributed, the mean with standard deviation (±SD) was reported. Where data deviated from normality, medians were reported with interquartile range (IQR).
A protocol‐prescribed one‐way between groups analysis of covariance (ANCOVA) was used to analyse differences between the NLFU + SOC and SOC arms of the primary endpoint, percentage change in wound area from baseline (week 5) to final visit (week 13). Patients' baseline (week 5) wound area was used as the covariate. Differences between the groups in actual change in wound area (cm2) between weeks 5 and 13 were also analysed in this way. Differences in the primary outcome between the groups were also analysed using a Student's t‐test and reported as non‐adjusted data. ANCOVA was also used for the secondary outcome, change in HRQoL from weeks 1 to 13 (with week 1 HRQoL score as the covariate), and a change in pain score [visual analogue scale (VAS)] from weeks 5 to 13. All variables were checked to ensure that the data did not violate the assumptions of normality, linearity, homogeneity of variances and homogeneity of regression slopes. Change in QoL scores and the number of infections were not normally distributed, and differences between the arms were tested using the non‐parametric Mann–Whitney U‐test. Differences in the number of patients having at least one AE were analysed using Fisher's exact test. In all tests, P‐values less than 0·05 were considered to be significant, and the tests were two sided. No correction was applied to account for the increased probability of a type I error associated with multiple testing because no P‐values were detected to be less than 0·05.
Results
Between August 2012 and August 2013, 47 patients were enrolled into the study and 36 (77%) were randomly allocated to receive either NLFU and standard care (NLFU + SOC) or standard care alone (SOC). Seventeen patients were allocated to NLFU + SOC and 19 to SOC; no patients were withdrawn following random allocation on week 5. Figure 2 shows the flow of participants through the study including reasons for withdrawal of 11 patients during the 4‐week run‐in period. The main reason for withdrawal prior to random allocation was reduction in wound area of >40% in 4 weeks (eight patients).The mean (SD) age during the enrolment of the 36 patients was 69 (12) years, the mean (SD) duration of the index ulcer at enrolment was 19 (16) months [median (range), 12·5 (2–54)], and the mean size of the index ulcer was 17·8 cm2 (12·7) [median (range), 12·3 (6–55)]. No significant differences in the participants' baseline demographics were observed including ulcer characteristics which are determinants of healing, for example wound size, wound duration, and percentage healing during run‐in period (Table 1). The numbers of scheduled, additional, and missed visits per patient are reported in Table 2. The full complement of scheduled treatments available to patients during the 8 weeks of allocated treatment in the NLFU + SOC and SOC‐only arms was 24 and 8, respectively (excluding treatments conducted in the final visit). Following randomisation, NLFU + SOC and SOC‐only patients received a median (range) of 23 (20–24), and 8 (7–8) scheduled treatments during the study, respectively (Table 1). Each application of NLFU had a mean (SD) duration of 3·8 (1·0) minutes. Additional visits were available to standard care patients if deemed clinically necessary by the treating clinician. SOC patients received a median of seven additional visits (range, 0–8) during the 8 weeks of allocated treatment.
Figure 2.
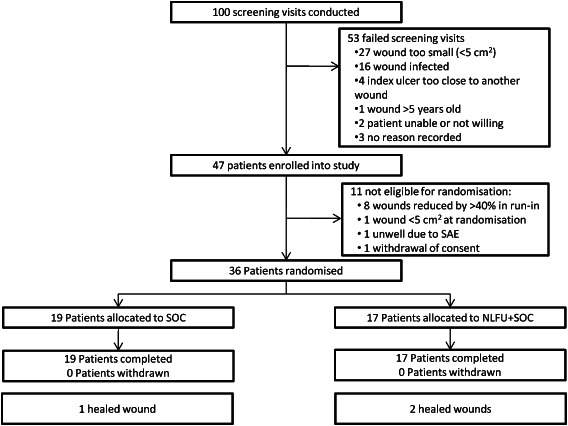
Participant flow diagram. NLFU, non‐contact low‐frequency ultrasound; SAE, serious adverse event; SOC, standard of care.
Table 1.
Baseline demographics of 36 participants allocated to receive either NLFU + SOC or SOC alone
| Baseline demographics | NLFU + SOC (n = 17) | SOC (n = 19) |
|---|---|---|
| Male (%)/female (%) | 47/53 | 37/63 |
| Age (years) | ||
| Mean (SD) | 70·5 (12·7) | 68·2 (12·2) |
| Median (range) | 74·0 (50–91) | 72·0 (42–86) |
| Weight (kg) | ||
| Mean (SD) | 90·1 (25·0) | 96·6 (20·1) |
| Median (range) | 85·75 (67·8–157·1) | 94·0 (55·1–142·0) |
| History of leg ulceration (months) | ||
| Mean (SD) | 109·7 (112·2) | 94·7 (83·2) |
| Median (range) | 84·0 (9–468) | 72·0 (8–300) |
| Index ulcer duration (months) | ||
| Mean (SD) | 15·7 (12·0) | 22·3 (18·5) |
| Median (range) | 12·0 (2·0–40·0) | 13·0 (1·5–54·0) |
| ABPI | ||
| Mean (SD) | 1·27 (0·23) | 1·23 (0·17) |
| Median (range) | 1·25 (0·93–1·83) | 1·21 (0·89–1·54) |
| Wound size at enrolment (cm2) | ||
| Mean (SD) | 15·9 (9·9) | 19·4 (14·90) |
| Median (range) | 11·7 (5·9–35·9) | 12·9 (6·5–55·1) |
| Index ulcer is recurrent (%) | 13 (76·5) | 14 (78·9) |
| Index ulcer location (%) | ||
| Malleolus | 9 (52·9) | 7 (36·8) |
| Gaiter | 7 (41·2) | 12 (63·2) |
| Calf | 1 (5·9) | 0 (0·0) |
| Change in wound size during run‐in (weeks 1–5) | ||
| Mean percentage (%; SD) | −10·9 (23·9) | −13·0 (25·2) |
| Actual change (cm2; SD) | −2·51 (4·2) | −2·55 (4·9) |
ABPI, ankle brachial pressure index; NLFU, non‐contact low‐frequency ultrasound; SD, standard deviation; SOC, standard of care.
Table 2.
Treatment details for 36 randomised patients in the study
| NLFU + SOC (n = 17) | SOC (n = 19) | |
|---|---|---|
| Number of scheduled treatments after randomisation per patient (excluding final visit; including healed weeks) | ||
| Median (range) | 23 (20–24) | 8 (7–8) |
| Mean (SD) | 22·7 (1·2) | 8·0 (0·2) |
| Number of additional visits per patient between enrolment and study end (dressing and compression therapy application only) | ||
| Median (range) | 4·0 (0–4)* | 11·0 (0–12) |
| Mean (SD) | 2·5 (1·8) | 9·6 (2·9) |
| Number of missed treatments per patient | ||
| Median (range) | 1·0 (0–4) | 0·0 (0–1) |
| Mean (SD) | 1·4 (1·2) | 0·1 (0·2) |
| Average duration of NLFU application per patient (minutes) | ||
| Median (range) | 3·3 (2·9–6·1) | – |
| Mean (SD) | 3·8 (1·0) | – |
NLFU, non‐contact low‐frequency ultrasound; SD, standard deviation; SOC, standard of care.
All additional visits were prior to randomisation for patients allocated to receive NLFU.
Primary outcome (change in wound area)
No statistically significant difference was observed in the percentage change in wound area between the two arms while controlling for the baseline wound area (measured at randomisation at week 5; Figure 3, Table 3). Patients treated with NLFU + SOC for 8 weeks showed a −46·6% (SD 38·1%) mean change in wound area, while patients treated with SOC only for 8 weeks showed a −39·2% (38·0%) mean change. The difference between treatment arms [while controlling for the effect of baseline wound area measured at week 5 which was not significant (P = 0·290)] was not significant [−7·42% difference; 95% confidence intervals (CIs) −33·4–18·6; P = 0·565] (Figure 3, Table 3). These percentage changes corresponded to a small and non‐significant difference in the actual wound reduction between the NLFU [−6·18 cm2 (5·54)] and SOC arms [−5·25 cm2 (5·53) of −0·94 cm2 (95% CIs −4·72 to 2·84; P = 0·618)] (Figure 4, Table 3). In this case, the influence of the covariate (baseline wound area) was significant (P < 0·001). Patients in both arms showed a considerable reduction in the wound area during the 12 weeks of the trial (including the 4‐week run in period). NLFU + SOC wounds showed a mean reduction of −48·7% (48·85) and a median reduction of −60·32% (range, −100% to 94·81%) during the 12 weeks. Standard care patients showed a mean reduction of −40·15% (46·13%) and a median reduction of 38·61% (range, −100% to 85·27%) during the 12 weeks of the study.
Figure 3.
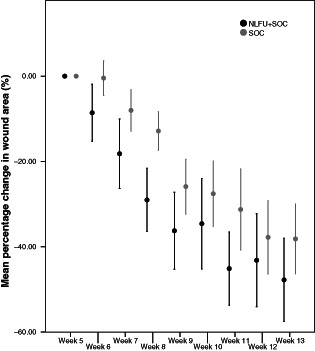
Mean percentage change in wound area from randomisation (week 5) to each subsequent week in patients allocated to receive 8 weeks of either NLFU and standard care or standard care alone. NLFU, non‐contact low‐frequency ultrasound; SOC, standard of care. Error bars represent ±1 standard error. Data for the two arms at the same time points are offset for clarity.
Table 3.
Primary outcome results from 36 patients randomised to receive either NLFU + SOC or SOC alone. Results are shown for percentage and actual area reduction following 8 weeks of treatment. Values which have been adjusted for the influence of the covariate (wound area at the beginning of treatment) are shown alongside non‐adjusted values
| NLFU + SOC (n = 17) | SOC (n = 19) | Difference (95% CIs) | P‐value | |
|---|---|---|---|---|
| Adjusted (planned) | ||||
| Mean percentage change in wound area (%) | −46·6 (SD, 38·1) | −39·2 (SD, 38·0) | −7·4 (−33·4 to 18·6) | 0·565 |
| Actual change in wound area (cm2) | −6·2 (SD, 5·5) | −5·3 (SD, 5·5) | −0·9 (−4·7 to 2·9) | 0·618 |
| Non‐adjusted | ||||
| Percentage change in wound area (%) | −47·8 (SD, 40·3) | −38·2 (SD, 35·6) | −9·6 (−35·3 to 16·1) | 0·453 |
| Actual change in wound area (cm2) | −5·6 (SD, 6·6) | −5·8 (SD, 6·2) | 0·1 (−4·2 to 4·5) | 0·954 |
CI, confidence interval; NLFU, non‐contact low frequency ultrasound; SD, standard deviation; SOC: standard of care.
Figure 4.
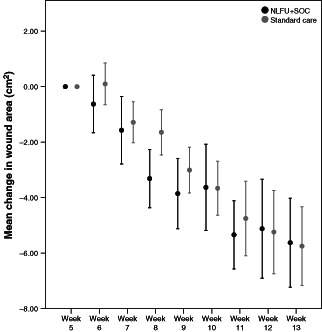
Mean change in wound area (cm2) from randomisation (week 5) to each subsequent week in patients allocated to receive 8 weeks of either NLFU and standard care or standard care alone. NLFU, non‐contact low‐frequency ultrasound; SOC, standard of care. Error bars represent ±1 standard error. Data for the two arms at the same time points are offset for clarity.
Three patients healed during the study period (one NLFU + SOC patient healed after 7 weeks and one after 8 weeks of NLFU + SOC treatment, and one patient who received standard care alone healed after 4 weeks). All three of these patients remained healed 90 days after the end of their study treatment. Nine wounds in the NLFU + SOC arm (52·9%) and seven wounds in the SOC arm (36·8%) reached at least 50% closure after 8 weeks of treatment (not significantly different); 12 NLFU + SOC wounds (70·6%) and 10 SOC wounds (52·6%) reached 25% wound closure. Two patients each in both arms did not improve during the course of the study.
Secondary outcome
Incidence of AEs and infections
A total of 60 AEs (24 in NLFU + SOC arm and 36 in SOC arm) were recorded as infections of the index ulcer or peri‐ulcer skin during the course of the study. No significant difference was observed in the median number of infections per patient between the NLFU + SOC [2 (IQR 0–3)] and SOC arms [2 (IQR 1–3) arms] (P = 0·346). Eleven NLFU + SOC patients and 16 SOC patients experienced at least one infection during the study; the difference was non‐significant (P = 0·255).
A total of 59 non‐serious AEs were recorded in the NLFU group and 70 in the standard care group, with the median number of non‐serious AEs per patient being 3 (IQR, 1·5–5·5) for NLFU and 4 (IQR, 3–4) for standard care. Of these total AEs, 34 in the NLFU arm were related to the index ulcer or surrounding skin, and 59 in the standard care arm. No AEs were related to the NLFU study device (any of ‘possibly’, ‘probably’, or ‘definitely’), and three were classified as related to standard care treatment. One serious adverse event (SAE) occurred after enrolment but prior to randomisation; it was assessed as not related to the study treatment. Six AEs were classified as moderate in nature (two NLFU + SOC; four SOC). Four protocol deviations were recorded during the course of the study. Three were because of patients having dressing changes outside of the study clinic on one occasion, and one was because of a wound measurement being taken 4 days later than scheduled.
Health‐related quality of life
NLFU + SOC and SOC patients showed a modest improvement in domains of ‘well‐being’ and ‘physical symptoms and daily living’ of the CWIS questionnaire between enrolment and the study end (Table 4). In the domain of ‘Social Life’ NLFU + SOC patients reported an improvement of 3.0 (SD 19.8) while SOC patients did not [−0.5 (SD 19.8)]. Across all domains of the questionnaire, differences between the groups were not significant (Table 4). Patients were asked to rate their overall HRQoL at the start and end of the study, as well as their satisfaction with their HRQoL (both scored from 0 to 10). No statistically significant difference in the median change in QoL scores between NLFU + SOC (median, −1; IQR, −2 to 2) and SOC (median, 0; IQR, −1 to 1) patients was found (P = 0·490). No difference was found in the change in QoL satisfaction between NLFU + SOC (median, 0; IQR, −2 to 1) and SOC (median, 0; IQR, −1 to 1) (P = 0·452) arms.
Table 4.
Change in Cardiff Wound Impact Schedule domain scores between start and end of the study having adjusted for influence of baseline measurement taken at week 1. Each domain is transformed to a score of between 0 and 100. Differences in mean score changes between patients treated with NLFU + SOC and those treated with SOC alone are shown
| Cardiff Wound Impact Schedule domain | NLFU + SOC (n = 17) | SOC (n = 19) | Difference (95% CIs) | P‐value* |
|---|---|---|---|---|
| Well‐being | 8·3 (SD, 16·2) | 8·0 (SD, 16·2) | 0·4 (−10·6 to 11·4) | 0·943 |
| Physical symptoms and daily living | 10·4 (SD, 10·7) | 5·8 (SD, 10·7) | 4·6 (−2·6 to 11·9) | 0·204 |
| Social life | 3·0 (SD, 19·8) | −0·5 (SD, 19·8) | 3·5 (−10·0 to 17·0) | 0·601 |
CI, confidence interval; NLFU, non‐contact low‐frequency ultrasound; SD, standard deviation; SOC, standard of care.
Influence of the covariate of baseline (week 1) measurement of each domain is significant at P < 0·05 across all three domains.
Ulcer pain and other characteristics
At baseline (week 5), patients in the NLFU + SOC group had a mean (SD) pain score of 26·8 (20·9) and median of 30·0 (range, 0–55) and the SOC group mean pain score was 20·7 (19·0) and median 16·0 (range, 0–57; recorded on a VAS from 0 to 100). At the study end (week 13), the NLFU + SOC patients had a mean (SD) pain score of 10·8 (15·0) and median (range) 3·0 (0–48), while SOC patients' mean was 16·9 (19·6) and median 9·0 (0–58) (Figure 5). NLFU + SOC patients reported a mean (SD) reduction in pain score [adjusted for the covariate of week 5 pain score which had a significant influence (P < 0·001)] of −14·35 (14·85) points between weeks 5 and 13, while SOC patients' pain scores reduced by −5·27 (14·84). Figure 5 shows non‐adjusted pain reduction scores. The difference between these adjusted scores was −9·08 (95% CIs, −19·23 to 1·06; P = 0·078), that is, not significant. The number of patients with malodorous wounds reduced following treatment with both NLFU + SOC and SOC alone (Table 5). In addition, the number of wounds which were heavily or moderately exuding reduced in both groups following treatment (Table 5).
Figure 5.
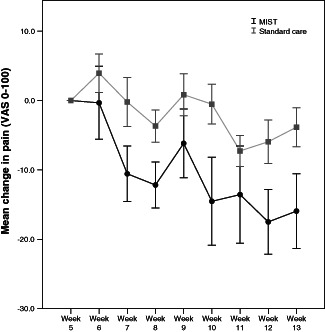
Mean change in patient reported pain scores from randomisation (week 5) to each subsequent week in patients allocated to receive 8 weeks of either NLFU + SOC or SOC alone. NLFU, non‐contact low‐frequency ultrasound; SOC, standard of care. Pain was measured on a visual analogue scale (VAS) from 0 to 100. Error bars represent±1 standard error.
Table 5.
Wound bed characteristics including wound bed condition, level of exudate, and wound odour, of patients before enrolment, at randomisation, and at study end. Each value refers to the number of patients in each group with percentages in parentheses
| NLFU + SOC | SOC | ||||
|---|---|---|---|---|---|
| At enrolment | Pre‐treatment | Post‐treatment | Pre‐treatment | Post‐treatment | |
| Fibrin | |||||
| <50% | 21 (58·3%) | 15 (88·2%) | 15 (88·2%) | 12 (63·2%) | 12 (63·2%) |
| ≥50% | 15 (41·7%) | 2 (11·8%) | 2 (11·8%) | 7 (36·8%) | 7 (36·8%) |
| Slough/necrosis | |||||
| <50% | 25 (69·4%) | 9 (52·9%) | 14 (82·4%) | 18 (94·7%) | 19 (100%) |
| ≥50% | 11 (30·6%) | 8 (47·1%) | 3 (17·6%) | 1 (5·3%) | 0 (0%) |
| Granulation | |||||
| <50% | 20 (55·6%) | 9 (52·9%) | 9 (52·9%) | 9 (47·4%) | 8 (42·1%) |
| ≥50% | 16 (44·4%) | 8 (47·1%) | 8 (47·1%) | 10 (52·6%) | 11 (57·9%) |
| Level of exudate | |||||
| None | 0 (0%) | 0 (0%) | 2 (11·8%) | 0 (0%) | 1 (5·3%) |
| Minimal | 9 (25·0%) | 1 (5·9%) | 9 (52·9%) | 5 (26·3%) | 12 (63·2%) |
| Moderate | 24 (66·7%) | 12 (70·6%) | 5 (29·4%) | 12 (63·2%) | 6 (31·6%) |
| Heavy | 3 (8·3%) | 4 (23·5%) | 1 (5·9%) | 2 (10·5%) | 0 (0%) |
| Copious | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Wound odour | |||||
| Yes | 1 (2·8%) | 4 (23·5%) | 1 (5·9%) | 2 (10·5%) | 1 (5·3%) |
| No | 35 (97·2%) | 13 (76·5%) | 16 (94·1) | 17 (89·5%) | 18 (94·7%) |
NLFU, non‐contact low‐frequency ultrasound; SOC, standard of care.
Discussion
The results of this study demonstrate that high‐quality wound care is instrumental in the outcome for patients with chronic VLUs as demonstrated by the high withdrawal rate owing to reduction in wound size during the run‐in period and improvement in both primary and secondary outcomes in both arms of the study. There was a possible suggestion across several measures (including reduction in wound size, pain and complete healing) that NLFU + SOC arm was superior to SOC‐alone arm; however, none of these differences were statistically significant. Therefore, it is not possible to conclude that NLFU therapy three times a week with SOC accelerates healing in chronic venous leg ulcers compared with SOC alone.
Although treatment with NLFU + SOC reduced the mean wound area more than SOC alone, the difference was not significant using either percentage or actual change in wound area. The difference in the primary outcome did not reach the pre‐defined clinically significant effect of 20% between the arms (actual difference was −7·4%).
There was little difference in patient‐reported measures using the CWIS questionnaire between the groups, and overall QoL showed little improvement from baseline in either arm. Patients in both groups of the study reported a reduction in pain, and although pain in the NLFU + SOC arm reduced considerably more than standard care arm, the difference was not statistically significant. Fewer AEs, including wound‐related AEs and infections, were recorded in the NLFU group; however, again the difference was non‐significant.
This is the first randomised trial on NLFU conducted in the UK and has several strengths. While the study was funded by the device manufacturer, the design, conduct and analysis has been entirely independent. Wound area measurements were performed by a single blinded assessor using a Silhouette digital wound planimetry device to reduce subjectivity and bias. Broad inclusion criteria were set to maximise generalisability, no patients withdrew following randomisation, no patients were lost to follow‐up, and best available standard treatment was applied. Patient‐reported pain and QoL data were collected using a validated tool (CWIS) 27 to explore outcomes important to patients. Excellent patient compliance to the three times a week NLFU regime was shown with few missed visits recorded. To improve homogeneity amongst the wounds, a 4‐week run‐in period was used to standardise pre‐randomisation ulcer treatment and to remove wounds which were not deemed hard‐to‐heal. In addition, the use of ANCOVA enabled the influence of patients' baseline wound measurement of area reduction to be controlled, thus improving the statistical power. Important prognostic factors of wound size and duration were balanced between the arms by a minimisation procedure (adaptive randomisation).
A key limitation of the study was the difference in treatment frequency between the groups which could potentially bias results in favour of NLFU. The rationale for this design was to compare the manufacturer's instructions for use (three times a week) with UK standard practice (treatment at least once a week) 2. Of note is the high frequency with which additional visits were applied (a median of one extra visit for each SOC patient each week). Although the sample size of the study was small, it was calculated to show a substantial clinical effect in line with the claims made by the device manufacturer. However, the standard deviation proved to be larger than estimated from the available literature which resulted in the study having reduced statistical power. A larger sample size may narrow the confidence intervals and a primary outcome in favour of NLFU may be detected (the clinically important difference of −20% was within the 95% CI), although the data presented in Figures 3 and 4 do not show a marked difference in the outcome between using NLFU + SOC and SOC only.
The treatment period of the trial was 8 weeks, and the outcome was percentage area reduction of the wound. A substantially longer trial would be required for the proportion of 100% healed wounds to be used as an outcome measure which Gottrup has argued is a better outcome measure 29. The ability of 4‐week wound reduction to predict healing is well documented 30 and may have been a more appropriate factor than wound area upon which to balance the trial groups. The open‐label nature of this study may also have introduced performance bias in favour of NLFU. Blinding of patients and clinicians can be difficult to administer and maintain in medical device trials 31; a sham device was carefully considered but ultimately ruled out owing to the complexity and inability to separate any ultrasound‐mediated effect from the debriding effects of the device.
Enrolment of homogenous groups of patients in chronic wound healing studies is notoriously difficult. The chronicity of many of the patient' ulcerations was further complicated by ulcer recurrence and effects of skin changes as a result of the underlying disease. The large standard deviation in the primary outcome reflects the heterogeneous nature of wound healing progression. In both arms, there were two patients whose index ulcer grew in size following randomisation. Review of the patients' cases revealed that the worsening NLFU + SOC patients were because of (i) merging the large index ulcer (18·7 cm2) with a small satellite ulcer (1 cm2), and (ii) possible underlying infection which recurred during the study. Additional analysis showed that removal of each patient did not result in a change to the statistical significance of the results.
The results of this study are reflective of results seen in many other wound studies. Where the primary end point is healing, the results often show little or no compelling evidence of a significant difference between the arms. It is possible that NLFU had a positive influence on the trajectory of wound healing and that identification of factors indicative of ‘responders’ versus ‘non‐responders’ may be of value. Clinicians currently rely on subjective wound assessments that may not identify subtle changes within the wound.
Practitioner feedback was that NLFU treatment was well tolerated by patients, it did not add to the patient's pain or discomfort, and for some patients, there was a decrease in pain following treatment (although the difference between arms of the trial was not significant). NLFU was very easy to use within the clinical setting. Following the completion of the study and during return clinic visits by the patients at various time points, practitioners have noted that a further 9 patients in the NLFU + SOC arm (from a total of 17) and 5 patients in the SOC only arm (from a total of 19) went on to complete healing. While this observation should be interpreted cautiously because it was not a study outcome, it suggests that a study with a longer follow‐up, and including patients that have not healed at the end of the study, may identify benefits related to NLFU which were not captured in this study.
This study suggests that while patients receiving NLFU + SOC showed a substantial improvement in their wounds, most, if not all of this effect was because of high‐quality SOC (compression therapy with appropriate dressings) applied by highly skilled practitioners in the context of a clinical trial unit. Early identification of local and systemic infection improved patient outcomes. Furthermore, this randomised controlled trial demonstrates the limited value of single‐arm baseline‐controlled studies where the influence of the compression therapy and best practice in the trial context is obscured. Reporting of such studies leads to inflated effect sizes such as those in the meta‐analysis carried out by Driver et al. 32, which estimated a wound area reduction of 85·2% in approximately 7 weeks owing to NLFU therapy.
Three other randomised controlled trials and a small pilot RCT have been conducted to evaluate the use of NLFU as a treatment for chronic lower limb wounds (10 16–18). A large volume of non‐comparative or baseline‐controlled retrospective and prospective studies also exist which report that NLFU enhances healing of chronic wounds. A small study such as this has wide CIs; it is possible that a much larger trial would show a statistically significant effect, although the effect size might still be small. This study was designed to be pragmatic and generalisable, as such the possibility remains that a narrower population with more recalcitrant wounds may respond to NLFU. Excluding patients whose wounds reduce by >30% in the run‐in phase may be an appropriate way to do this. In addition, the results of this study do not preclude NLFU as a treatment option for wounds other than venous leg ulcers, and the results of other NLFU regimes and doses cannot be extrapolated.
This is the first clinical trial to be conducted in response to questions raised in Medical Technologies Guidance issued by the NICE, the aim being to produce published results to address the uncertainties in the evidence base in a short time period and independently of both NICE and the device manufacturer.
Acknowledgements
The authors would like to acknowledge Ruth Poole (Cedar), Kathleen Withers (Cedar) and Andrew Cleves (Cedar) for their contribution to the management of this study; Jacqueline Fletcher (Cardiff University) and Mark Kelson (Research Design and Conduct Service, Cardiff University) for their input to the design of the study protocol; and Neal Walkley (Cardiff University) and Wendy Davies (Cardiff University) for their technical assistance. This study was sponsored by Cardiff and Vale University Health Board (NHS). This study was funded through an unrestricted research grant and equipment loan from Celleration (device manufacturer); Celleration played no role in the conduct of this study or analysis and reporting of the results. Cedar is a department within the UK NHS, and it receives funding from the National Institute for Health and Care Excellence (NICE) to act as an external assessment centre. NICE was involved in initial discussions about trial design but played no further role in the conduct or analysis of the study.
References
- 1. Demidova‐Rice TN, Hamblin MR, Herman IM. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 1: Normal and chronic wounds: biology, causes, and approaches to care. Adv Skin Wound Care 2012;25:304–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scottish Intercollegiate Guidelines Network . Management of chronic venous leg ulcers: a national clinical guideline (SIGN Guideline 120). Edinburgh: Scottish Intercollegiate Guidelines Network, 2010. [Google Scholar]
- 3. Troxler M, Vowden K, Vowden P. Integrating adjunctive therapy into practice: the importance of recognising ‘hard‐to‐heal’ wounds. [WWW document]. URL http://www.worldwidewounds.com/2006/december/Troxler/Integrating-Adjunctive-Therapy-Into-Practice.html [accessed on 4 November 2014]. [Google Scholar]
- 4. Lazarus G, Valle MF, Malas M, Qazi U, Maruthur NM, Doggett D, Fawole OA, Bass EB, Zenilman J. Chronic venous leg ulcer treatment: future research needs. Wound Repair Regen 2014;22:34–42. [DOI] [PubMed] [Google Scholar]
- 5. Graham ID, Harrison MB, Nelson EA, Lorimer K, Fisher A. Prevalence of lower‐limb ulceration: a systematic review of prevalence studies. Adv Skin Wound Care 2003;16:305–16. [DOI] [PubMed] [Google Scholar]
- 6. Moffatt CJ, Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. QJM 2004;97:431–7. [DOI] [PubMed] [Google Scholar]
- 7. Franks PJ, Moffatt CJ. Who suffers most from leg ulceration? J Wound Care 1998;7:383–5. [DOI] [PubMed] [Google Scholar]
- 8. Posnett J, Franks P. The cost of skin breakdown and ulceration in the UK. In: Pownell M, editor. Skin breakdown—the silent epidemic. Hull: Smith & Nephew Foundation, 2007:6–12. [Google Scholar]
- 9. Tennvall GR, Hjelmgren J. Annual costs of treatment for venous leg ulcers in Sweden and the United Kingdom. Wound Repair Regen 2005;13:13–8. [DOI] [PubMed] [Google Scholar]
- 10. Ennis WJ, Foremann P, Mozen N, Massey J, Conner‐Kerr T, Meneses P. Ultrasound therapy for recalcitrant diabetic foot ulcers: results of a randomized, double‐blind, controlled, multicenter study. Ostomy Wound Manage 2005;51:24–39. [PubMed] [Google Scholar]
- 11. Falanga V. Advanced treatments for non‐healing chronic wounds. [WWW document]. URL http://www.worldwidewounds.com/2005/april/Falanga/Advanced-Treatments-Chronic-Wounds.html [accessed on 4 November 2014]. [Google Scholar]
- 12. Kavros SJ, Schenck EC. Use of noncontact low‐frequency ultrasound in the treatment of chronic foot and leg ulcerations: A 51‐patient analysis. J Am Podiatr Med Assoc 2007;97:95–101. [DOI] [PubMed] [Google Scholar]
- 13. Keltie K, Reay CA, Bousfield DR, Cole H, Ward B, Oates CP, Sims AJ. Characterization of the ultrasound beam produced by the MIST therapy, wound healing system. Ultrasound Med Biol 2013;39:1233–40. [DOI] [PubMed] [Google Scholar]
- 14.Celleration Inc. Science of MIST therapy. http://www.misttherapy.com/medical-professionals/science-of-mist-therapy/ [accessed on 12 June 2014].
- 15. National Institute for Health and Clinical Excellence . Medical technology guidance 5. The MIST Therapy system for the promotion of wound healing. Manchester: National Institute for Health and Clinical Excellence, 2011. [Google Scholar]
- 16. Kavros SJ, Miller JL, Hanna SW. Treatment of ischemic wounds with noncontact, low‐frequency ultrasound: the Mayo clinic experience, 2004‐2006. Adv Skin Wound Care 2007;20:221–6. [DOI] [PubMed] [Google Scholar]
- 17. Olyaie M, Rad FS, Elahifar MA, Garkaz A, Mahsa G. High‐frequency and noncontact low‐frequency ultrasound therapy for venous leg ulcer treatment: a randomized, controlled study. Ostomy Wound Manage 2013;59:14–20. [PubMed] [Google Scholar]
- 18. Yao M, Hasturk H, Kantarci A, Gu G, Garcia-Lavin S, Fabbi M, Park N, Hayashi H, Attala K, French MA, Driver VR. A pilot study evaluating noncontact low frequency ultrasound and underlying molecular mechanism on diabetic foot ulcers. Int Wound J 2012. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cole PS, Quisberg J, Melin MM. Adjuvant use of acoustic pressure wound therapy for treatment of chronic wounds: a retrospective analysis. J Wound Ostomy Continence Nurs 2009;36:171–7. [DOI] [PubMed] [Google Scholar]
- 20. Haan J, Lucich S. A retrospective analysis of acoustic pressure wound therapy: effects on the healing progression of chronic wounds. J Am Col Certif Wound Spec 2009;1:28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Honaker JS, Forston MR, Davis EA, Wiesner MM, Morgan JA. Effects of non contact low‐frequency ultrasound on healing of suspected deep tissue injury: a retrospective analysis. Int Wound J 2013;10:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kavros SJ, Liedl DA, Boon AJ, Miller JL, Hobbs JA, Andrews KL. Expedited wound healing with noncontact, low‐frequency ultrasound therapy in chronic wounds: a retrospective analysis. Adv Skin Wound Care 2008;21:416–23. [DOI] [PubMed] [Google Scholar]
- 23. Escandon J, Vivas AC, Perez R, Kirsner R, Davis S. A prospective pilot study of ultrasound therapy effectiveness in refractory venous leg ulcers. Int Wound J 2012;9:570–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ennis WJ, Valdes W, Gainer M, Meneses P. Evaluation of clinical effectiveness of MIST ultrasound therapy for the healing of chronic wounds. Adv Skin Wound Care 2006;19:437–46. [DOI] [PubMed] [Google Scholar]
- 25. Amir L. Managing chronic conditions: economic analysis can help mitigate costs of diabetic ulcers. Healthc Financ Manage 2014;68:90–4, 96. [PubMed] [Google Scholar]
- 26. National Institute for Health and Clinical Excellence . Medical technologies guidance: scope. The MIST Therapy system for the promotion of wound healing in chronic and acute wounds. Manchester: National Institute for Health and Clinical Excellence, 2011. [Google Scholar]
- 27. Price P, Harding K. Cardiff Wound Impact Schedule: the development of a condition‐specific questionnaire to assess health‐related quality of life in patients with chronic wounds of the lower limb. Int Wound J 2004;1:10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Evans S, Royston P, Day S. MINIM: Allocation by minimisation in clinical trials [computer program]. 2013. [WWW document]. URL http://www-users.york.ac.uk/~mb55/guide/minim.htm [accessed on 4 November 2014].
- 29. Gottrup F, Apelqvist J, Price P. EWMA document: outcomes in controlled and comparative studies on non‐healing wounds: recommendations to improve the quality of evidence in wound management. J Wound Care 2010;19:239. [DOI] [PubMed] [Google Scholar]
- 30. Cardinal M, Eisenbud DE, Phillips T, Harding K. Early healing rates and wound area measurements are reliable predictors of later complete wound closure. Wound Repair Regen 2008;16:19–22. [DOI] [PubMed] [Google Scholar]
- 31. Boutron I, Guittet L, Estellat C, Moher D, Hróbjartsson A, Ravaud P. Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med 2007;4:0370–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Driver VR, Yao M, Miller CJ. Noncontact low‐frequency ultrasound therapy in the treatment of chronic wounds: a meta‐analysis. Wound Repair Regen 2011;19:475–80. [DOI] [PubMed] [Google Scholar]


