Abstract
Reconstruction is a basic task in craniofacial plastic surgery. Different methods must be used to meet the aspirations of surgeons and patients with different defects and deformities. We make a retrospective study of our experience of craniofacial reconstruction. In accordance with 10 years' clinical experience, direct suturing, skin graft transfer, nerve anastomosis, expanded pedicled or random flaps, facial local random flaps, reduction of mandibular fracture and correction of congenital craniofacial deformities were included in this case series. These types of treatment were applied to reconstruct facial defects or deformities according to different circumstances of patients. Directed by rational design and treatment, reconstructive surgery can be executed to treat different cases with different circumstances. A total of 891 different cases with different facial circumstances were treated with different methods: direct suturing (n = 93), skin graft transfer(n = 104), nerve anastomosis (n = 38), expanded pedicled or random flaps(n = 310), facial local random or pedicled flaps(n = 231), reduction of mandibular fracture(n = 112) and correction of congenital craniofacial deformities(n = 13). Reconstructive technique must be directed by reliable methods and special guidelines in Plastic Surgery. Three guidelines are summarised: reconstruction in the first stage and returning injured tissue to its origin site as far as possible for traumatic events; adjacent tissue must be prior to other distant tissue for reconstructive choice; and reconstruction at different stages after careful design.
Keywords: Adjacent tissue, Craniofacial reconstruction, Guidelines, Plastic surgery, Primary reconstruction
Introduction
Reconstruction is a basic and characterised subject in Plastic Surgery. Soft‐tissue defects, cranio‐maxillo‐facial congenital fractures and deformities that are caused by natural disasters, terrorist attacks, incidents and other trauma, congenital malformations, tumours, infections, radiation and surgery failure require reconstructive needs as the face is a critical region that must be repaired, with a high demand for function and aesthetics. No previous reports about the summary of facial reconstruction can be found. In this series, we want to share our experience of facial reconstruction on the basis of different types of defects or deformities.
Patients and methods
Between May 2005 and December 2015, all types of case series were included in this case series: traumatic events, minor or large carcinomas, fracture, congenital deformity, nerve fracture, burn injury, scar contracture deformity, scarred tissue defect, etc. A total of 891 different cases with different facial circumstances were treated with different methods: direct suturing (n = 93), skin graft transfer (n = 104), nerve anastomosis (n = 38), expanded pedicled or random flaps(n = 310), facial local random or pedicled flaps(n = 231), reduction of mandibular fracture(n = 112) and correction of congenital craniofacial deformities(n = 13). According to different methods used in the study, seven types of methods were categorised to treat different cases (Figures 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12).
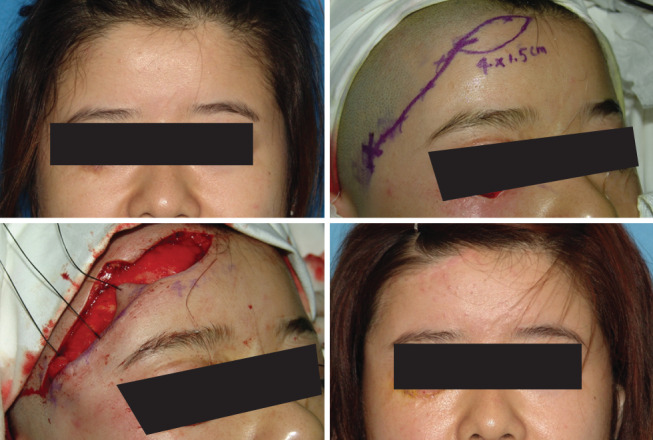
Figure 1.

A 32‐year‐old woman suffered from contusion on the forehead and bilateral upper eyelids. After debridement and direct closure, inconspicuous scar can be found, and function was not affected when opening eyes and closing eyes nearly 8 months postoperatively.
Figure 2.

A 18‐year‐old woman was hurt on the upper lip by accidentally falling down to the ground when she rode a horse. After debridement and closing the wound primarily, aesthetic results were achieved 6 years post‐surgery.
Figure 3.

A 21‐year‐old soldier was ordered to extinguish the forest fire. His face was burned unfortunately. After thorough debridement, skin graft was harvested to repair the wound. Functional and aesthetic results were attained 9 years after the operation. He is now our People's Literative Army commander and on military commission.
Figure 4.
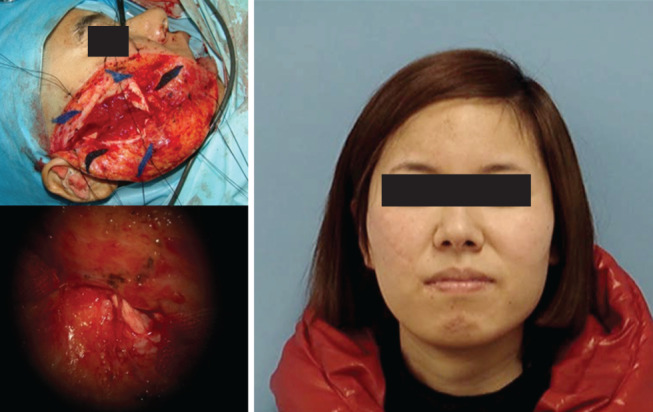
A 33‐year‐old woman was inflicted with a cut on the right face. She was admitted to our hospital 6 hours after the injury. After end‐to‐end sutures, function of facial nerve was restored to its original state. Static and dynamic sates were generally normal 8 months post‐surgery.
Figure 5.
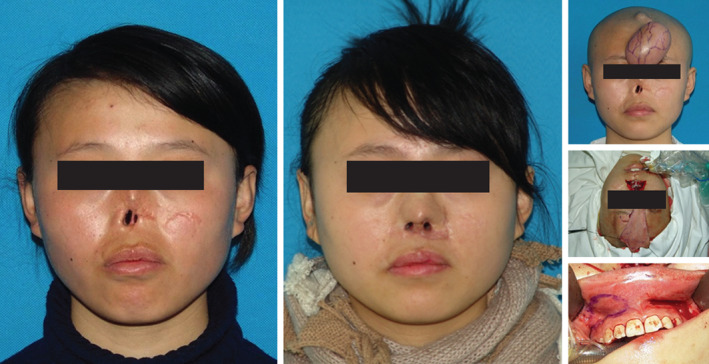
A 25‐year‐old woman was subjected to nasal defect. Rectangular expander of 250 ml was placed in the forehead to generate pedicled forehead flap. After expansion for about 4 months, expanded pedicled forehead flap and costicartilage were transferred to the reconstructed nose. Gingival mucosa was harvested to be used for inner coverage. Appearance improvement can be seen, and ventilation function could be retained 12 months post‐surgery.
Figure 6.

Scarred appearance induced by burn injury was seen on the faciocervical region. Six rectangular expanders with the capacity from 200 to 400 ml were placed around the scar. After 6 months, expanded flaps were transferred to the deformed area. In between, an expanded pedicled forehead flap was transferred to repair the secondary wound on the back of the nose. Better appearance was achieved 14 months after the operation.
Figure 7.

Subjected to bilateral facial cicatrix induced by burn injury, a 44‐year‐old woman was operated on by two rectangle expander for about 4 months pre‐expansion with about 1000 ml saline in each side on the chest wall, which was used to generate a new perforated flap pedicled by the frontal branch of the cervical transverse artery. With preoperative design of the size of 22 cm × 10 cm for each flap, the wound was covered fully. Satisfactory results were obtained 12 months after the operation. No complaint about mammal scar occurred.
Figure 8.

Hypertrophic scar was distributed on the faciocervical area. Two expanders, each with a rectangular expander of 300 ml, were implanted in the head to generate island flap pedicled by bilateral frontal branches of the superficial temporal artery. Another rectangular expander of 300 ml was placed in the cervical area. These bilateral pedicled flaps were transferred from the forehead area to the lower face and cervical area after expansion for 5 months. Improved appearance was found 2 years after the operation.
Figure 9.
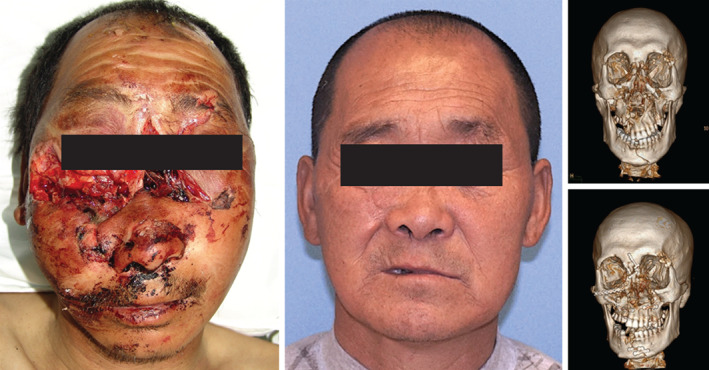
A 61‐year‐old peasant was afflicted with a maxillofacial fracture by a tractor turnover. Fractures of many sites can be observed by three‐dimensional CT scan. After debridement, template application to the fractures and soft tissue returned to its original site, inconspicuous scar and satisfactory facial appearance was be found 1 year after the operation. Function of facial nerve was generally normal.
Figure 10.
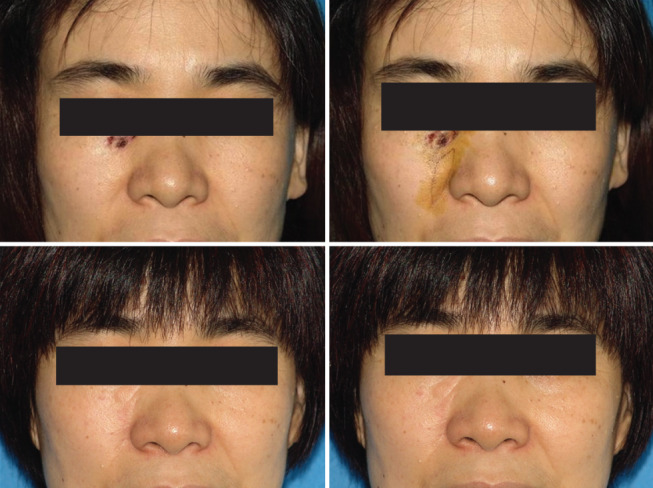
A 40‐year‐old woman was seen with naevus on the inside corner of right eye. Local nasolabial flap was designed and transferred to the defect after resection. Two years after the operation; no evident operative sign and naevus recurrence can be found.
Figure 11.
Right lower eyelid ectropion can be detected and flap pedicled by the right frontal branch of the superficial temporal artery was designed to repair the deformity. Eight months after the operation; original deformity was corrected, and no ectropion can be found.
Figure 12.
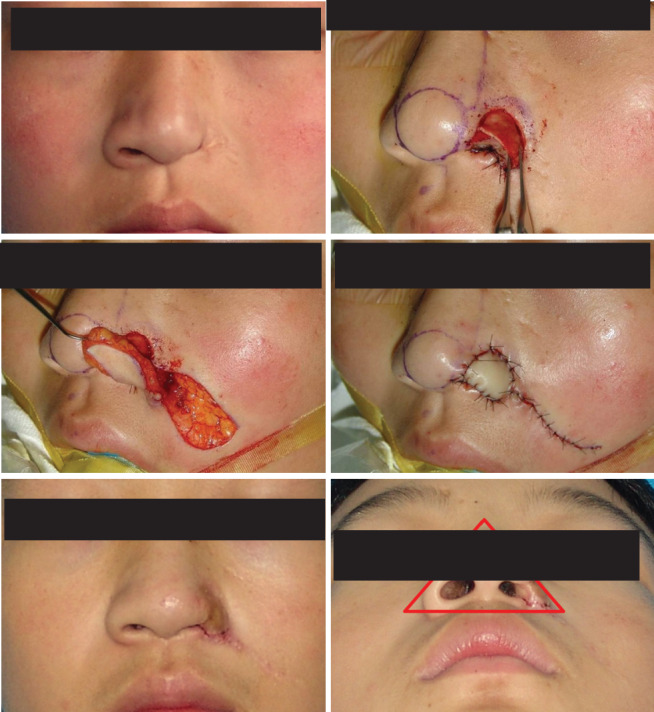
A 23‐year‐old woman was afflicted with scarred defect of left nasal wing. Auricular cartilage and nasolabial flap were combined to repair the wound; 15 months after the operation, general symmetrical appearance was demonstrated in the red triangle region.
Type 1 – Direct suturing for local facial bruise and minor carcinoma
Type 2 – Skin graft
Type 3 – Nerve neurorrhaphy
Type 4 – Expanded pedicled flaps for reconstruction
Type 5 – Reduction of mandibular fracture
Type 6 – Facial local random or pedicled flaps for defects and deformities
Type 7 – Congenital deformity correction
Results
A total of 891 different cases with different facial circumstances were treated with different methods: direct suturing (n = 93), skin graft transfer(n = 104), nerve anastomosis (n = 38), expanded pedicled or random flaps(n = 310), facial local random or pedicled flaps(n = 231), reduction of mandibular fracture(n = 112) and correction of congenital craniofacial deformities(n = 13). Complications were as follows: partial necrosis occurred in 6cases with skin graft transfer and 13 cases with expanded flaps; no necrosis was encountered in facial local flaps; poor occlusal was found in 4 patients with mandibular fracture; partial recovery of facial nerve function was detected after 12 months in 2 cases with facial nerve fracture; 3 cases expressed dissatisfaction with post‐operative outcomes.
Discussion
Facial reconstruction can be challenging. There are several reconstructive options, including primary repair, skin grafts, different local flaps, regional flaps, distant and free flaps, restoration of fracture, congenital deformity correction and nerve anastomosis. The ideal facial soft‐tissue reconstruction should provide a good colour and texture harmony with adjacent tissues. Optimal aesthetic reconstruction of facial defects is dependent on the availability of donor sites with similar colour, texture, sebaceous quality and thickness to the defect tissues. Direct suturing can be a simple method for local contusion and minor carcinoma. Studies showed that skin grafting was one of the most useful reconstructive modalities for skin and subcutaneous tissue defects; however, post‐operative scars were sometimes a determining factor of patient satisfaction; in particular, the colour match between the grafted skin and surrounding recipient skin was important 1. Split‐thickness skin grafting is widely used for primary wound coverage after skin cancer resection or relatively extensive skin defect coverage, such as extensive burns, because donor site morbidity is lower, and wider skin grafts are available 2. Particular attention should be given when skin grafting is considered for defect closure adjacent to eye lid, nasal margin or oral commissure because of concern of skin graft contraction 3. A great number of local flaps, pedicled flaps and micro‐vascular free flaps have been employed over the years for the reconstruction of facial defects. Because of its colour and texture that were thought to be advantageous over skin grafts, a diversity of flaps may be considered first. Assisted by a 3D CT scan, we can precisely identify the sites of mandibular fractures, which facilitated us to restore the fracture accurately. A facial nerve fracture is a critical injury that must be repaired as far as possible, which can promote the function restoration. Congenital deformity is a daunting problem that must be settled with comprehensive methods and staged surgery.
Plastic and Reconstructive Surgery is a discipline that confers the task of reconstruction to its inherent nature. Function and aesthetic problems are equally important, whereas the aesthetic problem is seldom considered in other departments. As a critical region, facial reconstruction is considered one of the most important and most difficult surgeries in cosmetic and reconstructive surgery. According to the above reconstructive cases, three guidelines are summarised in facial reconstruction.
Reconstruction in the first stage and returning injured tissue to its origin site as far as possible for traumatic events
As traffic accidents occur regularly because of more and more cars in China, an increasing number of acute cases are admitted to Emergency department. Another factor is aesthetic demand because they want to restore original appearance. Moreover, China is becoming richer, and people have additional money to consider their spiritual needs besides their material needs. Plastic surgery is also developing at a high rate in China. More and more people are aware of the concept that plastic surgery can make their wounds heal better with inconspicuous scars. Hence, plastic surgeons are required to complete the surgery that is assigned to other surgeons originally. However, these cases must pay a high fee for the surgery, and the majority of them can accept it. Obviously, some cases may request that no scar be found and other similar irrational demands. Under these circumstances, we cannot guarantee the demanded results, and we cannot complete the surgery. They may go to another hospital to seek help to meet their requirements. They do not know the basic knowledge of medicine. It is not a negligible factor that more and more lawsuits are filed about aesthetic surgery in China. As plastic surgeons, we cannot promise patients the fact that guaranteed satisfactory results can be attained. This abnormal phenomenon is rare in governmental hospital and common in private aesthetic hospitals. In our hospital, we set up an independent Emergency Plastic Surgery unit to treat these patients. Local anaesthesia surgery can be accomplished in the outpatient department for minor wounds, while general anaesthesia surgery can be prepared for severe trauma in the regular operating room. However, plastic surgery can not be popularised in remote areas. These acute cases cannot receive the plastic surgery for their craniofacial trauma for a variety of reasons, allowing for satisfactory results and malformation at worst. Every week, some patients from remote areas are transferred to our hospital to request plastic surgery for craniofacial traumatic events.
From the perspective of plastic surgeons, when we treat an acute case, more consideration must be born in mind. Functional and aesthetic problems are equally important. The primary goal in the management of traumatic events is to achieve rapid healing with optimal functional and aesthetic results, especially when a craniofacial wound is encountered. Hence, primary reconstruction or repair must be completed as far as possible. Another important principle is restoring the injured tissue to its original region and allowing for anatomic recovery. Tension‐free suturing must also be followed to reduce the scar. While the size of wound cannot be sutured directly, we should use tissue transfer to cover the wound, such as local flaps. However, secondary deformity in the donor site must be avoided, and scar in the donor site should be hidden from view at best. As different regions have been divided on the face, we must adhere to the regional reconstruction, especially while using the skin graft technique. The craniofacial nerve is a critical portion that can dominate the function of expressional muscles. While craniofacial nerve injury is definite, it is indispensable that nerve anastomosis must be executed as far as possible. Neurotrophic drugs can be also an assistant treatment to facilitate nerve recovery. Then mandibular fracture is also stiffly restored to its original site; the lower mandible fracture must especially be carefully fixed internally as its chew motion is required. Patients must also practice the chew motion after mandibular fracture recovery. Problems with teeth may be solved by dentists.
Experience can be concluded as follows: combined injury, such as brain, chest, abdomen or another fatal injury, is regularly encountered in those acute cases with instable vital signs that cannot be admitted into Plastic Surgery immediately. Traumatic events involving craniofacial sites are often non‐fatal. So, multidisciplinary consults should be prepared. System appraisal of the acute case must be implemented. Surgery of many sites can be executed simultaneously to guarantee not only the survival of acute cases but also functional and aesthetic results. Critical complex structures on the face are usually challenges for us plastic surgeons to reconstruct in the first stage, for instance, the nose and ear. It is advised that soft‐tissue defects must be covered by direct suturing or tissue transfer in the first stage. Cartilage can be carved to form three‐dimensional structures to be placed in the critical sites in the second stage. Hence, not all aesthetic results can be achieved in the first stage in those patients. Preoperative conversation with them about reconstruction with two stages is essential before the surgery. Regional flaps with the same character can be used to close the wound with priority if regional tissue is integral so as to allow for the optimum result. However, the adjacent area is usually wounded. So, skin graft or remote free flap should be considered. From our perspective, complex procedures and high risk are included in the remote free flaps procedure, which is not suitable for traumatic cases. However, if skin graft and regional flaps are not reliable tools that cab be used, we have to choose remote free flaps. We must bear in mind that a severe case, such as cerebral haemorrhage, is not suitable for immediate craniofacial reconstructive surgery. Craniofacial surgery is secondary to a cerebral haemorrhage. Patients with a severe combined injury should be transferred to the ICU or another department that includes critical sites' surgery that may lead to a patient's death.
Adjacent tissue must be prior to other distant tissue for reconstructive choice
Adjacent tissue when present, which is considered the best reconstructive option for moderate‐sized defects in the face, can be recognised as being analogous to the defect and prior to other choices 4. The axial pattern nasolabial and forehead flaps are work horse flaps for coverage of the nasal and perinasal areas because of their rich vascularity, consistent and reliable anatomy, enabling a long and flexible flap on a narrow pedicle 5, 6. The importance of a successful reconstruction of the facial features is apparent because of its exposure, and a simple single‐stage method is therefore preferable if available. Pedicled and expanded pedicled flaps are our preferred tools to cover the wound. On account of rich blood supply and anastomosis in the craniofacial and chest wall, many established flaps, such as nasolabial flap, orbicularis muscle flap and other pedicled flaps, can be used. In accordance with different regions, we should design rational flaps, and the appearance of donor site must be guaranteed after flap harvest. In the above case series, the designed expanded perforated flap pedicled by the frontal branch of the cervical transverse artery causes a bilateral scar on the chest wall or breasts. Afflicted with chronic cicatrisation appearing in the breast or chest skin, the flap is manipulated cautiously in women only when ample conversation is implemented prior to the operation. In view of the flap's route passing along the cervical area, when the cervical area is not involved, the flap is not the best choice for the extra scar on the cervical area. Then, the symmetry of bilateral breasts must be ensured. In Figure 13, after debridement and utility of regional flap to cover the wound, a tight nose‐wing was deficient, and asymmetry upper lib was presented 4 months after the operation. Correction of asymmetry was executed; pedicled flaps can be harvested from the forehead and chest wall, which are reliable regions to be used to develop pedicled flaps. Expanders can be used to enlarge the volume of donor skin. Expanded pedicled flaps can be generated when the expander is placed in the surface of deep fascia to guarantee the demanded artery in the expanded skin. Doppler must be applied to identify the artery preoperatively. Rational capacity of expanders must be carefully considered so as to avoid the excessive additional incision, which is thought to be minimised as far as possible on the face. When the donor site is presented with scar, it can also be used to correct the adjacent area. In our clinical application, scarred nasolabial flaps are used to reconstruct the defects of nasal wing, allowing for satisfactory results. Although adjacent tissue can be acknowledged as a useful tool, reconstruction at different stages after careful design must be considered. Patients with severe injury or deformity regularly require necessitated staged surgery. Cases who are featured by haemifacial atrophy and expanders placement necessitate staged surgery. These deformities and defects cannot be completely corrected in the first stage. Although adjacent local tissue can be the best choice for reconstruction, a remote free flap may be necessary when local tissue cannot be in its rational state.
Figure 13.

A 23‐year‐old worker was hurt by machine when he was on work. Defects of the right partial nasal and upper lip were cut off. After debridement and utility of regional flap to cover the wound, tight nose‐wing was deficient, and asymmetry upper lip was presented 4 months after the operation (the first row). Then, the forehead flap was designed to repair the right nose‐wing defect, and Abbe's flap was transferred to correct the deformity of the upper lip. Appearance was improved on the nose and upper lip 1 year after the operation (the second row).
Reconstruction with staged surgery
Congenital deformities and other procedures involved with expanders transfer are necessitated staged surgery. The former includes mandibular and soft‐tissue deformities. Mandibulardistractionosteogenesis (MDO) is a critical procedure and has received consensus. After MDO, the frame of the mandibular can be improved in the majority of patients. Then, soft‐tissue defects can be repaired with repeated fat graft or artificial substitute to fulfil the deficiency. However, even with the above corrections, post‐operative outcomes cannot be guaranteed. Recurrence of mandibular deformity and soft‐tissue filler absorption can discourage people from continual treatment. Cleft lip and palate is a common facial congenital deformity. In this article, we present a case with congenital no. 3 facial fissure. After comprehensive treatment, the appearance has been corrected satisfactorily. However, pronunciation is now being trained by special experts. Expander is a common useful tool for plastic surgeons. Expanded random flaps and pedicled flaps can be generated at different circumstances. It is critical that in the first stage, the expander must be placed into the different layers. The former can be placed into the superficial fascia, but the latter must be placed into the deep fascia. It is important for us to create a pedicled flap, which is associated with the second surgery. Obviously, Doppler detector is necessitated to identify pedicle (Figures 14, 15, 16).
Figure 14.

A new‐born child was diagnosed with congenital Tisser's 3 fissure. Defects can be found on the right eyelid, nasal and upper lip areas. After careful design and local flaps application, general normal appearance was observed 3 years after the operation, although other corresponding treatments must be added.
Figure 15.

A 6‐year‐old girl was diagnosed with congenital left facial dysplasia. With the application of artificial acellular dermis and repeated fat graft transfer, satisfactory appearance was found 12 months after the operation. However, because the girl is in the process of development, we will follow‐up until she becomes an adult.
Figure 16.

A 16‐year‐old child suffered form left facial dysplasia. He was operated on by osteotomy traction therapy. Ten months after the operation, and the deformed appearance was corrected a lot. Then, maxillary‐zygomatic complex was implanted into the left face, and better appearance was seen 4 months after the operation.
Summary
Plastic Surgery is a department that confers reconstructive surgery as its main task by using tissue transfer as its main tool. As function and aesthetic considerations are inherent in this special discipline, we should adhere to special principles to achieve satisfactory functional and aesthetic results. Although we present the above case series, not all types of cases can be included in this study. We expect the above limited experience to be beneficial for facial reconstruction.
Reference
- 1. Guyuron B, Elof E, Persing JA. Chapter 8: Flaps. In: Plastic surgery: indications and practice. Saunders: Elsevier, 2009. [Google Scholar]
- 2. Eedy D, Breathnach S, Walker N. Surgical dermatology. Oxford; Blackwell Science, 1996. [Google Scholar]
- 3. Heller L, Cole P, Kaufman Y. Cheek reconstruction: current concepts in managing facial soft tissue loss. Semin Plast Surg 2008;22:294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jackson IT. Forehead reconstruction. In: Jackson IT editor. Local flaps of the head and neck, 2nd edn. St. Louis: Quality Medical, 2010. [Google Scholar]
- 5. Thornton JF, Weathers WM. Nasolabial flap for nasal tip reconstruction. Plast Reconstr Surg 2008;122:775–81. [DOI] [PubMed] [Google Scholar]
- 6. Jackson IT. Midline forehead flaps in nasal reconstruction. Eur J Plast Surg 2004;27:105–13. [Google Scholar]


