Abstract
Thromboangiitis obliterans or Buerger's disease is a rare non‐atherosclerotic segmental inflammatory vasculitis that most commonly involves small and medium‐sized arteries, veins and nerves of the extremities, and generally affects young tobacco smokers. A 53‐year‐old man was found to have critical ischaemia of his left lower limb with foot gangrene. He underwent extremely distal surgical revascularisation using a great saphenous vein bypass graft. The choice of a very distal artery as run‐off vessel promoted a faster wound healing and pain relief, with improvement in quality of life.
Keywords: Surgery, Thromboangiitis obliterans, Wound healing
Introduction
Thromboangiitis obliterans (TAO) is a rare non‐atherosclerotic inflammatory disease affecting small and medium‐sized arteries and veins of the upper and lower extremities 1, 2. Young patients of low socioeconomic status with a history of smoking are generally affected.
Here, we describe a case of Buerger's disease of the lower limb, in a patient already submitted to surgical revascularisation of the upper limb for critical ischaemia in our institute 3. Therapeutic indications and management options are discussed.
Case report
A 53‐year‐old man, already submitted to transmetatarsal amputation of the first four fingers of his left foot in another institute, returned in our department complaining pain of his left foot and advanced gangrene at the site of the first finger, after transmetatarsal amputation, with discharge of pus (Figure 1).
Figure 1.

Gangrene and tissue loss at the site of the first finger after transmetatarsal amputation of the left foot.
A femoral pulse was palpable, but popliteal and distal pulses were absent. Hypothermia of the left foot was noted. He was a lifelong smoker but had no other cardiovascular risk factors. His blood pressure was 130/70 mm Hg, and the cardiovascular examination was normal. Electrocardiography showed normal sinus rhythm. Echocardiography excluded a proximal source of emboli, and his ejection fraction was 50%. The autoimmune profile was negative, and the hypercoagulability screen was normal. During hospitalisation, the patient received broad‐spectrum antibiotic therapy, subcutaneous low‐molecular‐weight heparin and intravenous therapy with prostanoids. An ultrasound examination showed patency of the femoral artery, while popliteal and tibial vessels resulted in occlusion. The great saphenous vein was of adequate calibre, length and morphology.
Arteriography revealed normal proximal vessels but distal small and medium vessels disease. An important collateral circulation was observed at the level of thigh and leg. Only a segment of plantar artery was patent (Figure 2A–C). The presence of pain and advanced gangrene of the foot represented the main indications for an attempt of extreme distal surgical revascularisation of the lower limb. He underwent extremely distal femoral–plantar bypass using great saphenous vein (Figure 3A,B), and surgical debridement at the site of first finger amputation. The particular fragility and weakness of the arterial wall involved in the inflammatory process led the surgeon to adopt a particular technique of clamping in order to minimise the trauma to the artery. After systemic heparinisation, a clamp was positioned only on the proximal part of the distal vessel, and an intravenous cannula was introduced into the distal part of the arteriotomy and it was connected by a 20‐cm‐long plastic tube to a 30‐ml syringe filled with heparinised saline solution. This system allowed regular flushing of the artery with heparinised saline solution, preventing thrombosis of the lumen, in addition to systemic heparinisation.
Figure 2.
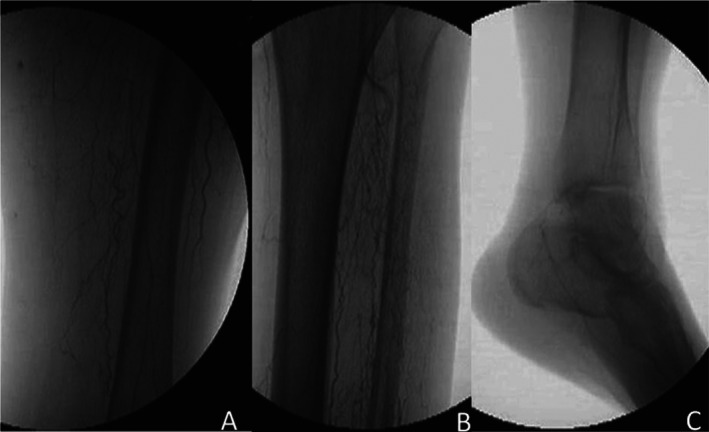
Arteriography revealed normal proximal vessels but distal small‐ and medium vessels disease. An important collateral circulation was observed at the level of thigh (A) and leg (B). Only a segment of plantar artery resulted patent (C).
Figure 3.
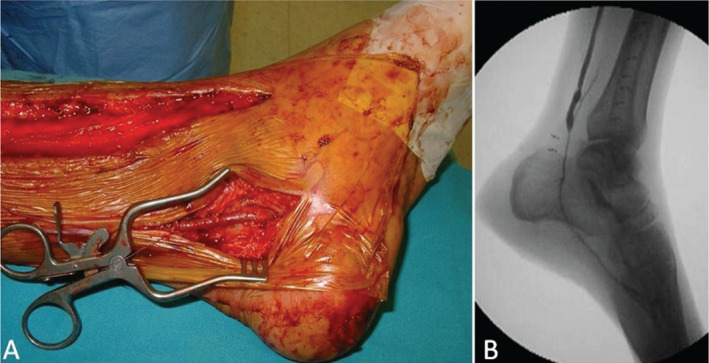
Intraoperative angiographic (A) and surgical (B) image of the distal anasthomosis.
A sample of the arterial wall was taken during surgery and submitted to histological examination to confirm the diagnosis of TAO. During the postoperative period, the patient received antibiotic therapy and subcutaneous low‐molecular‐weight heparin, and he continued intravenous therapy with prostanoids. Ultrasonography showed bypass graft patency and flow in the very narrow side branches of the foot. Limitation in tissue loss was observed clinically, and reduction in the C‐reactive protein level and white cell count occurred. The patient was discharged 10 days later on acetylsalicylic acid of 300 mg daily. Complete healing of the surgical wounds and remission of pain at rest were observed 30 days after surgery (Figure 4).
Figure 4.

Complete wound healing of the foot after surgical revascularisation of the left lower limb.
During follow‐up, ultrasonography showed patency of the bypass graft 12 months after surgery.
Discussion
TAO is a rare non‐atherosclerotic inflammatory disease affecting small and medium‐sized arteries and veins of the upper and lower extremities 1, 2. It tends to affect young people of low socioeconomic status, and smoking is considered a precipitating factor. To prevent a progression of TAO and avoid major amputations, the complete cessation of tobacco use appears necessary. However, in patients with advanced disease, the complete discontinuation of smoking does not rule out recurrent episodes of ischaemia.
Progression of the disease can cause intermittent claudication, pain at rest and ischemic ulceration of the toes, feet or fingers. Superinfection may occur, and the lesions progress to necrosis and distal gangrene.
The risk of major amputation, above or below the knee or even the hand, remains high, at between 4·4% and 11·8%. Median prevalence of amputation in patients with TAO, based on the most recently reported series, has been reported to be as high as 24·4% for minor amputations and 8·6% for major amputations, with a total amputation rate of 33% for patients treated conservatively 1.
In patients with an advanced stage of ischaemia not responding to medical therapy, distal surgical revascularisation represents the main procedure to prevent major amputations and improve the quality of life in these young people. To avoid traumatism of the arterial wall, the use of an atraumatic clamping technique for the run‐off vessel seems to be helpful. An accurate arteriographic and ultrasonographic mapping of the arterial vessels and a scrupulous mapping of the superficial venous system are necessary before surgery to avoid failure of the procedure.
Successful very distal revascularisation provides sufficient circulation to ischaemic areas and helps in the management of infection and tissue loss. Sometimes, the limited period of revascularisation provides a sufficient interval to heal the ischemic lesions, and important development of distal collateral circulation allows a reasonable limb salvage rate.
Other experiences of surgical revascularisation of lower limbs in TAO patients are reported in the literature 3. Dilege et al. 4 recorded 27 patients affected by TAO and submitted to distal revascularisation. During a 36‐month follow‐up, they recorded patency rates at the 12th, 24th and 36th months of 59·2%, 48% and 33·3%, respectively, and a limb salvage rate of 92·5%.
Sasajima et al. 5 reported 71 autogenous bypasses in 61 TAO patients, and they recorded a primary and a secondary patency rate of 48·8% and 62·5% at 5 years, and 43·0% and 56·3% at 10 years, respectively.
In the series reported by Nakajima 6, the 50‐month patency rate was 100% for above‐knee bypasses and 80% at 42 months for below‐knee bypasses.
An alternative to surgery is the sympathectomy that decreases arterial spasm in patients with TAO. A laparoscopic method for sympathectomy has also been used 7, 8, 9. Sympathectomy has been shown to provide short‐term pain relief and to promote ulcer healing in some patients with Buerger's disease, but no long‐term benefit has been confirmed 7.
Spinal cord stimulator and vascular endothelial growth factor gene therapy have been used experimentally in patients with TAO with promising results 9, 10, 11, 12.
Intravenous therapy with iloprost (a prostaglandin analogue) can provide pain relief at rest and complete healing of lesions. It diminishes the risk of amputation 13.
In our experience, the extreme attempt of distal revascularisation represents the gold standard of treatment for young patients affected by TAO, presenting rest pain or trophic lesions (stages 4–6 of Rutherford classification). Pharmacological therapy with intravenous prostaglandins is indicated for patients with TAO presenting claudicatio intermittens and could be considered an adjuvant therapy after surgical procedures.
An accurate preoperative mapping of arterial and venous vessels through ultrasound examination and selective arteriography is necessary to reduce the rate of graft failure.
The choice of a very distal artery as run‐off vessel could promote a faster wound healing of trophic lesions and pain relief, with improvement in the quality of life.
The rapid development of many distal side circles after revascularisation can maintain a sufficient vasculature of the extremities, sometimes also after graft failure.
Acknowledgements
The authors received no funding. The authors declare no conflict of interest.
References
- 1. Puéchal X, Fiessinger JN. Thromboangiitis obliterans or Buerger's disease: challenges for the rheumatologist [Review]. Rheumatology (Oxford) 2007;46:192–9. [DOI] [PubMed] [Google Scholar]
- 2. Mills JL Sr. Buerger's disease in the 21st century: diagnosis, clinical features, and therapy [review]. Semin Vasc Surg 2003;16:179–89. [DOI] [PubMed] [Google Scholar]
- 3. Massara M, De Caridi G, Spinelli F. A case of upper limb extreme surgical revascularization in Buerger's disease. Asian Cardiovasc Thorac Ann 2013, in press. doi: 10.1177/0218492313496587. [DOI] [PubMed] [Google Scholar]
- 4. Dilege S, Aksoy M, Kayabali M, Genc FA, Senturk M, Baktiroglu S. Vascular reconstruction in Buerger's disease: is it feasible? Surg Today 2002;32:1042–7. [DOI] [PubMed] [Google Scholar]
- 5. Sasajima T, Kubo Y, Inaba M, Goh K, Azuma N. Role of infrainguinal bypass in Buerger's disease: an eighteen‐year experience. Eur J Vasc Endovasc Surg 1997;13:186–92. [DOI] [PubMed] [Google Scholar]
- 6. Nakajima N. The change in concept and surgical treatment on Buerger's disease – personal experience and review. Int J Cardiol 1998;66(Suppl 1):S273–80; discussion S281. [DOI] [PubMed] [Google Scholar]
- 7. Chander J, Singh L, Lal P, Ramteke VK. Retroperitoneoscopic lumbar sympathectomy for Buerger's disease: a novel technique. JSLS 2004;8:291–6. [PMC free article] [PubMed] [Google Scholar]
- 8. Lau H, Cheng SW. Buerger's disease in Hong Kong: a review of 89 cases. Aust N Z J Surg 1997;67:264–9. [DOI] [PubMed] [Google Scholar]
- 9. Arkkila PE. Thromboangioitis obliterans (Buerger's disease). Orphanet J Rare Dis 2006;1:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Swigris JJ, Olin JW, Mekhail NA. Implantable spinal cord stimulator to treat the ischemic manifestations of thromboangioitis obliterans (Buerger's disease). J Vasc Surg 1999;29:928–35. [DOI] [PubMed] [Google Scholar]
- 11. Isner JM, Baumgartner I, Rauh G, Schainfeld R, Blair R, Manor O, Razvi S, Symes JF. Treatment of thromboangioitis obliterans (Buerger's disease) by intramuscular gene transfer of vascular endothelial growth factor: preliminary clinical results. J Vasc Surg 1998;28:964–73. [DOI] [PubMed] [Google Scholar]
- 12. De Caridi G, Massara M, Benedetto F, Tripodi P, Spinelli F, David A, Grande R, Butrico L, Serra R, de Franciscis S. Adjuvant spinal cord stimulation improves wound healing of peripheral tissue loss due to a steal syndrome of the hand. Clinical challenge treating a difficult case. Int Wound J 2014, in press. doi: 10.1111/iwj.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fiessinger JN, Shafer M. Trial of iloprost versus aspirin treatment for critical limb ischaemia of thromboangioitis nobliterans. The TAO study. Lancet 1990;335:555–7. [DOI] [PubMed] [Google Scholar]


