ABSTRACT
Pyoderma gangrenosum is a neutrophilic dermatosis clinically characterised by the presence of painful skin ulcerations with erythematous and undetermined borders and histologically by the presence of neutrophilic infiltrates in the dermis. Granulocyte and monocyte adsorption apheresis, also called granulocytapheresis, is a therapeutic strategy for extracorporeal immunomodulation that selectively removes activated granulocytes and monocytes/macrophages from the peripheral blood. Here, we report a case of a 73‐year‐old patient affected by a severe form of pyoderma gangrenosum presenting with multiple painful ulcers and pustules on his trunk and extremities. The disease was resistant to high doses of methylprednisolone and methotrexate and successfully treated by granulocyte and monocyte adsorption apheresis. To the best of our knowledge, this is the first report on the efficacy of granulocyte and monocyte adsorption apheresis in pyoderma gangrenosum in Europe.
Keywords: Granulocyte and monocyte adsorption apheresis, Neutrophilic dermatosis, Pyoderma gangrenosum
Introduction
Pyoderma gangrenosum (PG) is an inflammatory disease, which belongs to the spectrum of neutrophilic dermatoses 1. It is clinically characterised by the presence of painful skin ulcerations with erythematous and undetermined borders and histologically by the presence of neutrophilic infiltrates in the dermis 1, 2. PG has an annual incidence of 3–10 per million persons 1, and it is frequently associated with other diseases, notably ulcerative colitis (UC), Crohn's disease (CD), rheumatoid arthritis, seronegative arthritis, myelodysplastic syndrome, multiple myeloma, polycythemia vera, paraproteinemia and leukaemia 2. The treatment of PG usually includes high‐dose glucocorticosteroids, dapsone, minocycline, methotrexate, cyclosporine, mycophenolate mofetil, intravenous immunoglobulin (IVIG) and TNF‐alpha inhibitors 2, 3.
Granulocyte and monocyte adsorption apheresis, also called granulocytapheresis (GCAP), is a therapeutic strategy for extracorporeal immunomodulation that selectively removes activated granulocytes and monocytes/macrophages from the peripheral blood 4.
It has been initially approved for the treatment of UC because of activated granulocytes 5, 6, 7. GCAP has also been reported to be effective for other disorders attributable to activated neutrophils, including PG 8, 9, 10, 11, 12, 13, 14, 15, 16, 17. Here, we report a case of refractory PG successfully treated by GCAP.
Case report
In January 2015, a 73‐year‐old Caucasian man presented for the first time to our Dermatology Unit with multiple painful ulcers and pustules on his trunk and extremities. He stated that he first noticed an ulcer on his left leg in November 2014. Then, erythema, multiple pustules and the formation of progressively enlarging ulcers appeared on his trunk over 2 months. His past medical history was negative for chronic illnesses except for elevated blood pressure, high cholesterol level and diabetes. On the initial physical examination, we noticed multiple ulcers, varying between 2 cm and 8 cm in diameter, with erythematous and undetermined borders and multiple pustules on his trunk and lower extremities (Figures 1A and 2). Laboratory tests showed elevated white blood cells (13·16 × 109/l) and neutrophil count (9·41 × 109/l), increased erythrocyte sedimentation rate (44 mm/h) and C‐reactive protein level (72·60 mg/dl) and a monoclonal gammopathy of undetermined significance (3·78 g/l). A skin biopsy specimen revealed a dense infiltration of neutrophils through the dermal layer consistent with the histological features of PG. No bacterial or fungal infections were detected in the swabs obtained from the ulcers. Thus, the diagnosis of PG was made on the basis of clinical and histological findings. General examinations, including chest X‐ray, abdominal ultrasonography and PET‐TC, did not show systemic disorders. Systemic therapy with methylprednisolone acetate 60 mg daily was started. Despite the addition of methotrexate 7·5 mg weekly and doxycycline 100 mg twice daily, after 8 weeks of treatment, skin lesions were exacerbated. Methotrexate was discontinued because of liver toxicity, while GCAP (Adacolumn®, Otsuka Pharmaceuticals, Tokyo, Japan) was started in addition to methylprednisolone acetate 60 mg daily. A total of 10 sessions of GCAP at 7‐day intervals were conducted without complications. After the sixth session of GCAP, the ulcers began to heal, leaving scars (Figure 1B). At present, the patient is still taking oral prednisone 5 mg daily and dapsone 50 mg daily as maintenance therapy. No recurrences of ulcers were found during a follow‐up period of 6 months.
Figure 1.
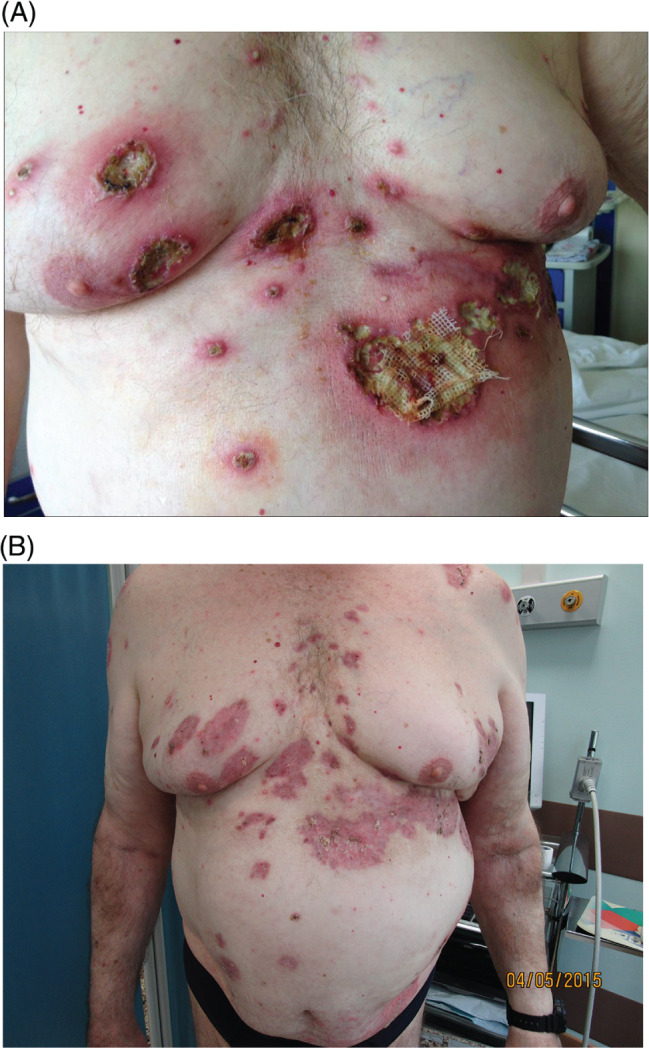
Multiple ulcers with erythematous and undetermined borders and multiple pustules on the trunk (A); changes in clinical findings of the skin ulcers of the trunk after six sessions of GCAP (B).
Figure 2.

Enlargement of a big ulcerative lesion of the shoulder.
Discussion
GCAP was initially approved for the treatment of UC 5, 6, 7. Later, it was shown to be effective on various skin conditions, such as generalised pustular psoriasis, psoriatic arthritis, systemic lupus erythematosus skin rash, Behcet's disease and PG 8, 9, 10, 11, 12, 13, 14, 15, 16, 17.
The efficacy of GCAP has been reported in some patients with both PG and an inflammatory bowel disease (either UC or CD) 13, 18, 19, but only seven patients with PG have been successfully treated with this apheretic technique 14, 15, 16, 17. Case reports on the efficacy of GCAP in PG are limited to Japan, so to the best of our knowledge, this is the first report in Europe.
GCAP is believed to impact not only the quantity but also the quality of granulocytes and monocytes. There are different studies regarding the mechanisms of cytapheresis for the treatment of PG by GCAP. GCAP removes Mac‐1‐expressing neutrophils to the cellulose acetate beads and CD11b + activated neutrophils. Thus, neutrophils are selectively adsorbed, and their cell counts decrease. The result of this process is the reduction of neutrophil infiltration into the inflamed regions. In addition, it reduces the circulating levels of inflammatory cytokines, such as TNF‐alpha, interleukin (IL)‐1b, IL‐6 and IL‐8. However, the precise mechanisms of the GCAP method have not been understood yet 20, 21, 22.
GCAP represents a promising and innovative treatment option for PG and other refractory skin disorders linked to activated neutrophils. It is an effective alternative to currently existing therapies, with minimal side effects compared to other systemic therapies. However, it is difficult to estimate the effects of GCAP alone on PG, because GCAP was used in combination with other therapies in our case. Overall, we consider GCAP a new and safe treatment option for the therapy of steroid and immunosuppressant‐resistant PG.
References
- 1. Cozzani E, Gasparini G, Parodi A. Pyoderma gangrenosum: a systematic review. G Ital Dermatol Venereol 2014;149:587–600. [PubMed] [Google Scholar]
- 2. Ahronowitz I, Harp J, Shinkai K. Etiology and management of pyoderma gangrenosum: a comprehensive review. Am J Clin Dermatol 2012;13:191–211. [DOI] [PubMed] [Google Scholar]
- 3. Goodarzi H, Sivamani RK, Garcia MS, Wehrli LN, Craven H, Ono Y, et al. Effective strategies for the management of pyoderma gangrenosum. Adv Wound Care 2012;1:194–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saniabadi AR, Hanai H, Takeuchi K, Umemura K, Nakashima M, Adachi T, Shima C, Bjarnason I, Lofberg R. Adacolumn, an adsorptive carrier based granulocyte and monocyte apheresis device for the treatment of inflammatory and refractory diseases associated with leukocytes. Ther Apher Dial 2003;7:48–59. [DOI] [PubMed] [Google Scholar]
- 5. Sawada K, Ohnishi K, Kosaka T, Fukui S, Yamamura M, Amano K, et al. Leukocytapheresis therapy with leukocyte removal filter for inflammatory bowel disease. J Gastroenterol 1995;30:124–7. [PubMed] [Google Scholar]
- 6. Shimoyama T, Sawada K, Hiwatashi N, Sawada T, Matsueda K, Munakata A, et al. Safety and efficacy of granulocyte and monocyte adsorption apheresis in patients with active ulcerative colitis: a multicenter study. J Clin Apheresis 2001;16:1–9. [DOI] [PubMed] [Google Scholar]
- 7. Hanai H, Watanabe F, Takeuchi K, Iida T, Yamada M, Iwaoka Y, et al. Leukocyte adsorption apheresis for the treatment of active ulcerative colitis: a prospective, uncontrolled, pilot study. Clin Gastroenterol Hepatol 2003;1:28–35. [DOI] [PubMed] [Google Scholar]
- 8. Fujisawa T, Suzuki S, Mizutani Y, Doi T, Yoshida S, Ogura S, Seishima M. Granulocyte and monocyte adsorption apheresis for generalized pustular psoriasis: therapeutic outcomes in three refractory patients. Ther Apher Dial 2015;19:336–41. [DOI] [PubMed] [Google Scholar]
- 9. Tominaga C, Yamamoto M, Imai Y, Yamanishi K. A case of old age‐onset generalized pustular psoriasis with a deficiency of IL‐36RN (DITRA) treated by granulocyte and monocyte apheresis. Case Rep Dermatol 2015;7:29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fujisawa T, Moriya C, Shibuya Y, Kanoh H, Seishima M. Combination therapy of infliximab and granulocyte/monocyte adsorption apheresis for refractory pustular psoriasis with psoriatic arthritis. Acta Derm Venereol 2013;93:364–5. [DOI] [PubMed] [Google Scholar]
- 11. Kanekura T, Hashiguchi T, Mera Y, Katahira A, Nakamura I, Maruyama I, Kanzaki T. Improvement of SLE skin rash with granulocyte and monocyte adsorption apheresis. Dermatology 2004;208:79–80. [DOI] [PubMed] [Google Scholar]
- 12. Higashi Y, Shimokawa M, Kawai K, Kanekura T. Granulocyte and monocyte adsorption apheresis for Behçet's disease in a pregnant woman. J Dermatol 2013;40:1042–4. [DOI] [PubMed] [Google Scholar]
- 13. Ikeda K, Hamada T, Otsuka M, Iwatsuki K. Beneficial effects of neutrophil‐targeted therapy for pyoderma gangrenosum associated with ulcerative colitis. Eur J Dermatol 2011;21:804–5. [DOI] [PubMed] [Google Scholar]
- 14. Okuma K, Mitsuishi K, Hasegawa T, Tsuchihashi H, Ogawa H, Ikeda S. A case report of steroid and immunosuppressant‐resistant pyoderma gangrenosum successfully treated by granulocytapheresis. Ther Apher Dial 2007;11:387–90. [DOI] [PubMed] [Google Scholar]
- 15. Seishima M, Mizutani Y, Shibuya Y, Nagasawa C, Aoki T. Efficacy of granulocyte and monocyte adsorption apheresis for three cases of refractory pyoderma gangrenosum. Ther Apher Dial 2007;11:177–82. [DOI] [PubMed] [Google Scholar]
- 16. Kanekura T, Kawahara K, Maruyama I, Kanzaki T. Treatment of pyoderma gangrenosum with granulocyte and monocyte adsorption apheresis. Ther Apher Dial 2005;9:292–6. [DOI] [PubMed] [Google Scholar]
- 17. Kanekura T, Maruyama I, Kanzaki T. Granulocyte and monocyte adsorption apheresis for pyoderma gangrenosum. J Am Acad Dermatol 2002;47:320–1. [DOI] [PubMed] [Google Scholar]
- 18. Ohno M, Koyama S, Ohara M, Shimamoto K, Kobayashi Y, Nakamura F, Mitsuru K, Andoh A. Pyoderma gangrenosum with ulcerative colitis successfully treated by the combination of granulocyte and monocyte adsorption apheresis and corticosteroids. Intern Med 2016;55:25–30. [DOI] [PubMed] [Google Scholar]
- 19. Kawakami T, Yamazaki M, Soma Y. Reduction of interleukin‐6, interleukin‐8, and anti‐phosphatidylserine‐prothrombin complex antibody by granulocyte and monocyte adsorption apheresis in a patient with pyoderma gangrenosum and ulcerative colitis. Am J Gastroenterol 2009;104:2363–4. [DOI] [PubMed] [Google Scholar]
- 20. Cuadrado E. Granulocyte/monocyte apheresis as immunotherapic tool: cellular adsorption and immune modulation. Autoimmun Rev 2009;8:292–6. [DOI] [PubMed] [Google Scholar]
- 21. Kanekura T, Hiraishi K, Kawahara K, Maruyama I, Kanzaki T. Granulocyte and monocyte adsorption apheresis (GCAP) for refractory skin diseases caused by activated neutrophils and psoriatic arthritis: evidence that GCAP removes Mac‐1‐expressing neutrophils. Ther Apher Dial 2006;10:247–56. [DOI] [PubMed] [Google Scholar]
- 22. Hanai H, Takeda Y, Eberhardson M, Gruber R, Saniabadi AR, Winqvist O, Lofberg R. The mode of actions of the Adacolumn therapeutic leucocytapheresis in patients with inflammatory bowel disease: a concise review. Clin Exp Immunol 2011;163:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


