Abstract
Resource use and costs for topical treatment of hard‐to‐heal ulcers based on data from the Swedish Registry of Ulcer Treatment (RUT) were analysed in patients recorded in RUT as having healed between 2009 and 2012, in order to estimate potential cost savings from reductions in frequency of dressing changes and healing times. RUT is used to capture areas of improvement in ulcer care and to enable structured wound management by registering patients with hard‐to‐heal leg, foot and pressure ulcers. Patients included in the registry are treated in primary care, community care, private care, and inpatient hospital care. Cost calculations were based on resource use data on healing time and frequency of dressing changes in Swedish patients with hard‐to‐heal ulcers who healed between 2009 and 2012. Per‐patient treatment costs decreased from SEK38 223 in 2009 to SEK20 496 in 2012, mainly because of shorter healing times. Frequency of dressing changes was essentially the same during these years, varying from 1·4 to 1·6 per week. The total healing time was reduced by 38%. Treatment costs for the management of hard‐to‐heal ulcers can be reduced with well‐developed treatment strategies resulting in shortened healing times as shown in RUT.
Keywords: Compression therapy; Cost savings; Dressing material; Hard‐to‐heal leg, foot and pressure ulcers; Structured wound management
Introduction
Hard‐to‐heal ulcers, defined as ulcers which have not healed within 6 weeks 1, are rarely seen in individuals who are otherwise healthy. Ulcer patients frequently display other conditions such as venous or arterial insufficiency, diabetes, and obesity 2, 3. These patients are consequently treated by different caregivers, while the medical and nursing responsibility in Sweden lies within the primary care 2, where the majority of patients are treated. The organisation of wound management differs throughout the country, as pointed out in a recent report from the SBU, the Swedish Council on Health Technology Assessment 4. Many patients have been treated for weeks, months and even years without a proper diagnosis and hence have received suboptimal treatment. Hard‐to‐heal ulcers thus represent a silent epidemic that affects a large fraction of the population and poses a major and growing threat to public health 3.
Healing time is not only an important endpoint in wound management 5 but also, along with the frequency of dressing changes, one of the most important factors in health‐economic assessment of wounds 6, 7. It is difficult to estimate the total cost for all categories of hard‐to‐heal ulcers, as the resource utilisation is often spread over a long period of time and is widely distributed within both health care and society.
Multiple studies have been conducted to determine the best management approach to hard‐to‐heal ulcers, specifically therapies that promote healing, reduce the cost and duration of treatment and reduce or prevent recurrence. Improvement in patient care often focuses on pain, as it has the strongest impact on health‐related quality of life 3, 8, 9.
The amount of money spent on wound care, the loss of productivity for the affected individuals and the families that care for them and their diminished quality of life come at great cost to our society 3. Total costs in the primary and community care are strongly related to the frequency of dressing changes and to healing time, i.e. nursing costs 6, 7, 10, 11, 12.
Other aspects include disability and loss of wages related to leg, foot and pressure ulcers.
To minimise the potential long‐term disability caused by hard‐to‐heal ulcers 3, structured wound management was introduced in clinical practice a decade ago at Blekinge Wound Healing Centre (BWHC), using a web‐based quality registry as a checklist for ulcer assessment and a basis for quality improvement. BWHC is a general practitioner‐led, primary care‐based specialist centre covering the treatment and follow‐up of the majority of ulcer patients across the county (150 000 inhabitants). Initial results showed that accurate diagnosis could lead to effective treatment and consequently to decreased prevalence, care time and costs 10.
The registry was later developed into the Swedish Registry of Ulcer Treatment (RUT), www.rut‐europe.eu, which includes patients with various types of ulcers such as leg, foot and pressure ulcers treated in different parts of Sweden by different caregivers such those from primary care, hospital care, community care and private care. A recently published report based on the RUT data showed that healing time for ulcers decreased significantly from 146 days (21 weeks) in 2009 to 63 days (9 weeks) in 2012 2.
The aim of this study was to analyse resource use in physical units and costs for topical treatment of ulcers that healed during 2009 to 2012, based on data from the RUT, and to estimate potential cost savings from reductions in the frequency of dressing changes and healing times.
Materials and methods
The Swedish RUT
In recent decades, a system of national quality registries has been established in the Swedish health and medical services covering different areas of medicine 13. The aim of the registries is to gather data on diagnoses, symptoms, interventions and treatment outcomes in order to give a continuous systematic evaluation of medical practice.
There are currently around 100 registries, each of which receives central funding after annual applications to SKL, the Swedish Association of Local Authorities and Regions (http://www.skl.se). The majority of the Swedish national quality registries were developed by physicians with special interest in a research field, in order to bring about quality improvement to health care for a specific medical problem. The RUT was initiated and developed by a general practitioner (RFÖ, the main author of this study) and introduced nationally in 2009.
The RUT is a practical tool offering a structured team management of ulcer care with the emphasis on diagnosis and documentation to guarantee optimal treatment. The ambition of the registry is to follow every patient with a hard‐to‐heal ulcer until ulcer healing, regardless of the geographical location within Sweden or where the care is given. In 2012, 184 of the approximately 1390 wound management units in Sweden registered their patients in the RUT, compared with 312 units in December 2014.
The purpose of the registry is to assess a reliable diagnosis and to record treatment strategies such as compression therapy; dressing alternatives including antiseptic treatment, negative pressure wound therapy and larvae therapy; antibiotic treatment and treatment with analgesics. To guarantee continuity of care and facilitate follow‐up of every patient to completion of healing, there is a mandatory variable containing the name of the nurse responsible for ulcer care. This nurse is often the person responsible for registering the patient with RUT. The development and content of the registry have been described previously 2.
Study population
The study population consisted of all patients who were registered in the database between May 2009 and the end of 2012. The number of new registrations increased during this time, with 162 in 2009, 356 in 2010, 428 in 2011 and 529 in 2012. At the end of 2012, the registry contained 1475 patients with a median age of 80 years (range: 11–103 years). The majority of the patients were women (60%), the median ulcer duration was 12 weeks (mean: 117 weeks, range: 1 week–46 years) and the median ulcer size was 3 cm2 (mean: 12 cm2, range: 0·05–600 cm2). For 208 patients, the register data were incomplete and no information about visits, dressing changes or outcome was available. These patients were therefore excluded from further analyses. In addition, 151 patients (10%) had died and 43 (3%) had undergone amputation and were not followed up further in the registry. As we used the results from the earlier study 2, patients who were unhealed at the end of the study period time were also excluded from the analyses of costs. Hence, the patients included in the cost calculations are those who were registered as healed before the end of 2012 (N = 1073) and thus the numbers in the analyses differ from the total number of patients included in the database.
Characteristics of the patients included in the cost calculations are shown in Table 1, and the distribution of ulcer diagnoses is illustrated in Figure 1. The most common type of ulcer was venous leg ulcers. Other types of ulcers such as arterial, venous/arterial, pressure, diabetic, tumour and inflammatory small vessel ulcers were less common.
Table 1.
Characteristics of patients included in the cost calculations based on the Registry of Ulcer Treatment, 2009–2012
| 2009–2012 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|
| N = 1073 | N = 119 | N = 266 | N = 322 | N = 366 | |
| Gender, n (%) | |||||
| Male | 429 (40·0) | 37 (31·1) | 102 (38·3) | 149 (46·3) | 141 (38·5) |
| Female | 644 (60·0) | 82 (68·9) | 164 (61·7) | 173 (53·7) | 225 (61·5) |
| Age, mean (range) | 77 (12–104) | 79 (12–102) | 79 (19–104) | 77 (15–99) | 76 (37–101) |
| Ulcer size in cm2, mean (range) | 8·7 (0–235) | 12·8 (0–159) | 7·7 (0–123) | 7·0 (0–106) | 9·6 (0–235) |
Figure 1.
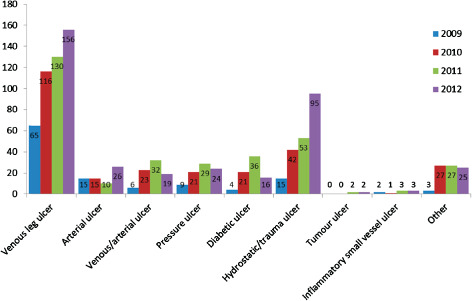
Ulcer diagnoses among patients included in the cost calculations based on the Registry of Ulcer Treatment, 2009–2012.
Cost calculations and analyses
Costs were calculated for dressing material, compression and the nursing staff who performed dressing changes. Costs for compression were added for patients where such treatment was registered at the follow‐up visits (mainly those with venous leg ulcers).
The use of dressings was recorded in the registry as a specific dressing type but without any brand names or size of dressing. Material costs were therefore calculated based on information about unit costs for the most commonly used dressing size of each specific type of dressing in BWHC (personal communication). Material costs were weighted according to unit cost and the proportion of each type of dressing registered in the data base in relation to the total number of registered dressings. The most commonly used type of dressing was polyurethane foam (used in 34% of cases) followed by gels (15%), hydrocolloids (13%) and hydrofibres (9%). Other types of dressings were less common, constituting 1–5% of the total number of dressings. The weighted material cost per dressing change (SEK22·21) was thus calculated according to the actual use of each type of dressing recorded in the registry and the unit cost for each type of dressing. There is no information included in the registry about the time used for each specific dressing change. The unit cost for nurses who performed dressing changes was therefore assumed to approximate the cost for a nursing staff visit (SEK580) on an official price list in the southern part of Sweden 14.
Material and staff costs were calculated according to all dressing changes that were registered for each patient in the database from inclusion until follow‐up after healing and multiplied by the weighted unit costs for dressings and the unit cost for staff. The participating units covered primary care (50%), community care (4%), hospital care (22%), wound healing centres (22%) and private caregivers (2%). All costs are expressed in SEK at 2014 prices. No discounting was performed, because the mean healing time was less than 1 year in all years analysed (2009–2012). The perspective of the analysis was the Swedish health care sector. Information about absence from work due to presence of ulcers is not included in the registry.
Ethical considerations
The approval of the Ethical Review Board of Lund University was obtained (2008/15), and consent was required from all patients before their registration in the national quality registry.
Statistics
The statistical analyses were performed using version 13.1 of the STATA software package (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). Continuous variables are expressed as mean values, ranges and standard deviations (SD), while qualitative variables are presented as numbers and percentages. Healing time was assessed with Kaplan–Meier analysis. A log‐rank test was used for evaluation of healing times.
Results
The mean healing time for patients who healed decreased from 269 days in 2009 to 139 days in 2012, and the corresponding median healing time decreased from 160 to 100 days (P < 0·001) according to log‐rank test analysis. The total healing time decreased by 38%, while the frequency of weekly dressing changes remained almost the same during the study period (Table 2).
Table 2.
Mean healing time in days and average number of weekly dressing changes among patients who healed in 2009–2012
| 2009–2012 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|
| N = 1073 | N = 119 | N = 266 | N = 322 | N = 366 | |
| Healing time (days) | 170 | 269 | 186 | 156 | 139 |
| Dressing changes per week | 1·5 | 1·4 | 1·5 | 1·5 | 1·6 |
Costs
The mean per‐healed‐patient costs for management of hard‐to‐heal ulcers are shown in Table 3 and Figure 2. The total mean per‐patient treatment cost decreased from approximately SEK38 000 in 2009 to SEK20 500 in 2012, mainly as a result of shorter healing times. Staff costs accounted for the major portion (approximately 87%) of total costs. The mean cost of compression decreased from 2009 to 2012 because of a decreased proportion of venous leg ulcers and an increased proportion of other ulcer types, in addition to the decreased number of treatment days until healing.
Table 3.
Mean (SD) costs per patient healed for management of ulcers, 2009–2012 (in SEK, 2014 prices)
| 2009–2012 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|
| N = 1073 | N = 119 | N = 266 | N = 322 | N = 366 | |
| Dressing material | 803 (1073) | 1276 (2184) | 848 (989) | 729 (806) | 682 (680) |
| Nursing staff | 20 978 (28 009) | 33 323 (57 031) | 22 149 (25 827) | 19 039 (21 039) | 17 818 (17 747) |
| Compression | 2322 (2956) | 3624 (4540) | 2449 (3279) | 2108 (2621) | 1995 (2108) |
| Total | 24 103 (30 969) | 38 223 (62 048) | 25 446 (28 798) | 21 876 (23 760) | 20 496 (19 741) |
Figure 2.
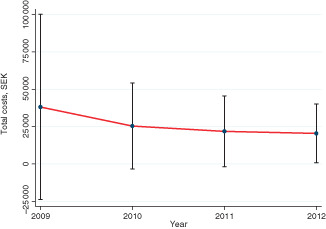
Total costs (mean, SD) for management of ulcers that healed in 2009–2012.
The costs for management of venous leg ulcers were somewhat lower than that for the whole population, but decreased in a similar pattern over the years. In 2009, the total mean per‐healed‐patient costs were approximately SEK32 000, decreasing to SEK19 000 in 2012.
Discussion
We found in the present analysis that the average topical treatment costs for management of hard‐to‐heal ulcers within the Swedish RUT decreased by 46% between 2009 and 2012 for patients who achieved ulcer healing. The reduction of costs was mainly the result of shorter healing times, which were reduced by 38%.
Costs can also be lowered through less frequent dressing changes, as long as the quality of care and healing times are not negatively affected. In the present study, no change in the frequency of dressing changes could be observed during the study period of 4 years. This might be because the centres participating in the registry had already settled on the optimal number of dressing changes per week.
The cost impact of leg ulceration is not well documented in Europe 3. The European Wound Management Association (EWMA) has identified different aspects of hard‐to‐heal ulcers that ought to be taken into account in a health economic analysis from a societal perspective 15. There are three main categories: (i) initial costs for assessment of the wound, (ii) treatment of the wound and (iii) any other health care costs resulting from the wound. In this study, we considered costs for assessment and treatment of the wound until healing. We did not consider other health care costs resulting from the wound, as these data are not registered in the RUT.
Besides treatment costs, some patients are unable to reconcile wound care therapy with the requirements of their jobs. These challenges may lead to lost wages or early retirement, as found in up to 12·5% of workers with venous ulcers in USA 3, 16. We did not consider societal costs related to loss of production, because the patients registered in RUT have a median age of 80 years and as such will have retired from work.
Costs of hospitalisation, as a result of surgery or adverse outcomes, have also been reported as a major contributor to the total costs of care. This is especially true for patients with diabetes and foot ulcers who heal after an amputation, but a Swedish study has shown that for patients who healed primarily without amputation, the main costs were the costs of topical treatment 17.
In the future, we plan to link our registry to the Swedish National Registry for Vascular Surgery (Swedvasc), which would allow us to easily find the patients undergoing surgery.
A potential limitation of the study is that the registry was initiated by the main author. As for the majority of the Swedish national quality registries, most of the research within the specific medical area of the registry is conducted by a steering group and is often carried out by the registry manager. The RUT has been introduced internationally (www.rut‐worldwide.org) and as such has been integrated into research and quality improvement projects worldwide 18.
The registry contains different types of hard‐to‐heal ulcers, such as leg, foot and pressure ulcers. An advantage of the present analysis is that the calculations included all patients recorded in the RUT who had healed before the end of 2012.
A possible limitation of the analysis is that we did not differentiate the cost calculations between different ulcer types, except for venous leg ulcers, where the results showed similar patterns of reduced healing times and related treatment costs as for the whole population.
Subgroup analyses of other types of ulcer would have required a greater number of patients than presently available from the registry. When the registry has been introduced in additional centres and clinics, and more patients have been included, further analyses can be performed.
Another possible limitation is that the cost calculations are limited to the direct management of ulcers, specifically dressing changes including costs of dressing material and nursing staff. One reason for our choice to analyse resource use in physical units and costs for topical treatment of healed ulcers is that these costs are directly related to the frequency of dressing changes and healing time. Another is that the aim of the cost analysis was to focus on the direct management of wound treatment based on the data collected in the registry. Other costs such as surgery and in‐hospital treatment were not included, mainly because information about this type of resources is not available in the registry.
Previous researchers have found that randomised controlled studies may not reflect the complex issues faced in clinical practice 19. The SBU expert group found that data from national quality registries such as the RUT and Swedvasc could be used as a complement to clinical studies, as they constitute a research base with great potential 4.
In Sweden, wound management is negatively impacted by the absence of national guidelines for medical ulcer care as well as the major regional differences in the organisation of wound management with respect to specialised wound clinics, level of care and care processes 4. A future study will investigate the differences in the results of ulcer care between areas in Sweden where the RUT is used and areas where it is not used.
In our study, we found that 10% of the patients had died and 3% had been amputated. The resource consequences for these patients will be addressed in a future study.
The research area of antimicrobial dressing contra treatment with systemic antibiotics for local wound infection is being addressed in an ongoing research study within the frame of the RUT.
A future in‐depth analysis when additional patients have been registered in the database will be focused on different types of ulcers and consider more patient‐related details.
Conclusions
The mean per‐healed‐patient costs for management of hard‐to‐heal ulcers have decreased from approximately SEK38 000 in 2009 to SEK20 500 in 2012, mainly as a result of shorter healing times. Staff costs accounted for the major portion (approximately 87%) of total costs. The costs for management of venous leg ulcers showed a similar pattern over the years.
Treatment costs associated with dressing changes and the management of hard‐to‐heal ulcers can be reduced by using optimal treatment strategies, which result in shortened healing times as shown in the RUT.
References
- 1. Nelzén O, Bergqvist D, Lindhagen A, Hallböök T. Chronic leg ulcers: an underestimated problem in primary health care among elderly patients. J Epidemiol Community Health 1991;45:184–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Oien RF, Forssell H. Ulcer healing time and antibiotic treatment before and after the introduction of the Registry of Ulcer Treatment: an improvement project in a national quality registry in Sweden. BMJ Open 2013;3:e003091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup F, Gurtner GC, Longaker MT. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 2009;17:763–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chronic ulcers in the elderly – prevention and treatment. SBU – Swedish Council on Health Technology Assessment 2014. ISBN: 978‐91‐85413‐67‐6. [PubMed]
- 5. Morrell CJ, Walters SJ, Dixon S, Collins KA, Brereton LM, Peters J, Brooker CG. Cost effectiveness of community leg ulcer clinics: randomised controlled trial. BMJ 1998;316:1487–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Posnett J, Gottrup F, Lundgren H, Saal G. The resource impact of wounds on health‐care providers in Europe. J Wound Care 2009;18:154–61. [DOI] [PubMed] [Google Scholar]
- 7. Ragnarson Tennvall G, Hjelmgren J. Treatment of venous leg ulcers is costly for the health care and the society. The value of preventive measures should be further investigated according to a study. Lakartidningen 2005;102:3027–9 [in Swedish]. [PubMed] [Google Scholar]
- 8. Lindholm C, Bjellerup M, Christensen OB, Zederfeldt B. Quality of life in chronic leg ulcer patients: an assessment according to the Nottingham Health Profile. Acta Derm Venereol 1993;73:440–3. [DOI] [PubMed] [Google Scholar]
- 9. Oien RF, Akesson N, Forssell H. Assessing quality of life in patients with hard‐to‐heal ulcers using the EQ‐5D questionnaire. J Wound Care 2013;22 442–4, 446–7. [DOI] [PubMed] [Google Scholar]
- 10. Oien RF, Ragnarson Tennvall G. Accurate diagnosis and effective treatment of leg ulcers reduce prevalence, care time and costs. J Wound Care 2006;15:259–62. [DOI] [PubMed] [Google Scholar]
- 11. Ragnarson Tennvall G, Andersson K, Bjellerup M, Hjelmgren J, Oien R. Treatment of venous leg ulcers can be better and cheaper. Annual costs calculation based on an inquiry study. Lakartidningen 2004;101 1506–8, 1510, 1512–1513 [in Swedish]. [PubMed] [Google Scholar]
- 12. Ragnarson Tennvall G, Hjelmgren J. Annual costs of treatment for venous leg ulcers in Sweden and the United Kingdom. Wound Repair Regen 2005;13:13–8. [DOI] [PubMed] [Google Scholar]
- 13. Lundström M, Albrecht S, Serring I, Wendel E. Handbook for establishing quality registries. Karlskrona: EyeNet Sweden, 2005. ISBN 91‐631‐8585‐7 (978‐91‐631‐8585‐4).
- 14.Skåne Regional Council. Regional rates and allowances for the Southern Health Region 2014 [in Swedish]. URL http://www.skane.se/Upload/Webbplatser/Sodra%20regionvardsnamnden/prislista/2014/helaprislistan2014.page101.
- 15. Gottrup F, Apelqvist J, Price P. Outcomes in controlled and comparative studies on non‐healing wounds: recommendations to improve the quality of evidence in wound management. J Wound Care 2010;19:237–68. [DOI] [PubMed] [Google Scholar]
- 16. de Carvalho MR. Comparison of outcomes in patients with venous leg ulcers treated with compression therapy alone versus combination of surgery and compression therapy: a systematic review. J Wound Ostomy Continence Nurs 2015;42:42–6. [DOI] [PubMed] [Google Scholar]
- 17. Apelqvist J, Ragnarson Tennvall G, Persson U, Larsson J. Diabetic foot ulcers in a multidisciplinary setting. An economic analysis of primary healing and healing with amputation. J Intern Med 1994;235:463–71. [DOI] [PubMed] [Google Scholar]
- 18. Öien RF, Weller CD. The Swedish national quality Registry of Ulcer Treatment (RUT): how can ‘RUT’ inform outcome measurement for people diagnosed with venous leg ulcers in Australia? WP&R 2014;22:74–7. [Google Scholar]
- 19. Moffatt CJ, Doherty DC, Smithdale R, Franks PJ. Clinical predictors of leg ulcer healing. Br J Dermatol 2010;162:51–8. [DOI] [PubMed] [Google Scholar]


