Abstract
Knowledge about methods and materials and their correct usage is the basis for compression therapy. This study compares knowledge and practical skills of participants with further training with those who had no training. This comparison provides information on whether further qualifications have an impact on knowledge and practical skills.
In seminars for compression therapy, data on specific and non‐specific expertise were acquired. A practical test determined the participants' skills for creating a compression bandage in a pressure value range of 50–60 mmHg.
In total, 1338 participants with specific expertise and 138 participants with non‐specific expertise took part. Knowledge evaluation showed that 7·9% of the specific expertise group had knowledge regarding padding, 10% regarding multi‐component systems and 13·6% regarding ulcer stocking systems. In the practical test, 12·3% of all participants achieved the target range.
The majority of users in both groups is not familiar with the different compression materials or their appropriate usage. In the non‐specific expertise group, knowledge concerning up‐to‐date materials and methods is one‐third lower. The practical test showed major deficits on both sides. Appropriate exercises, for example, with pressure‐measuring devices, should be mandatory for all professional groups who perform compression bandaging.
Keywords: Compression bandages, Multi‐component systems, Practical nursing, Ulcer stocking systems, Venous leg ulcer
Introduction
With a fraction of 37–80%, venous ulceration is the most common type of chronic leg ulcerations 1, 2, 3. The most severe clinical manifestation of venous insufficiency are venous leg ulcers (VLU). Between 0·1% and 0·2% of the German population suffers from VLU 3, 4. In international published studies, the prevalence of VLU in England, US and Sweden ranges between 0·2% and 2·5% 5, 6, 7.
Therapy focuses on the reduction of ambulatory hypertension and oedema. Compression therapy is an important cornerstone for VLU treatment, and the chance of wound healing is significantly lower without it. The higher the level of mobility of a patient, the more effective the compression therapy 8, 9. This treatment expedites the healing of VLU and lowers the rate of recurrence 3, 10, 11. Adequate compression therapy improves quality of life, and poorly performed compression bandaging has little or no benefit 12. During the initial reduction phase (initial decrease oedema), the leg is generally treated with compression bandages. Furthermore, there is strong evidence that higher pressure is better for wound healing than lower pressure 11, 13, 14. Healing of VLU may be delayed by ineffective compression therapy 15.
According to publications and guidelines, a phlebological compression bandage has to be applied with high pressure 3, 16, 17. A phlebological compression bandage that is able to produce a pressure of 30–50 mmHg (millimetres of mercury) in the ankle region may reduce the pressure strain in the vein system 18. Hence, products for the compression therapy of VLU are developed to guarantee such a pressure 19, 20. The pressure values of international classifications differ from each other 15. According to an international consensus of the International Compression Club (ICC), the following compression pressure values are recommended: mild (<20 mmHg); medium (≥20–40 mmHg); strong (≥40–60 mmHg), which is recommended for the treatment of patients with VLU; and very strong (>60 mmHg) 19, 21.
It was observed that the initial pressure under short‐stretch bandages decreases significantly within the first 30 minutes after applying 18. One investigation shows a pressure drop of 50% after 7 hours 20. Compression therapy can only be successful if an adequate pressure persists for an appropriate period of time. Therefore, it is essential to achieve an accordingly high initial pressure by applying short‐stretch bandages.
To date, there are only a few studies that examine the knowledge and practical skills of users, for example, nurses, physicians and therapists and their practical skills for applying compression bandages 15, 16, 17, 18, 20, 22, 23. These studies did not analyse differences between users with specific expertise and those without specific expertise. However, national and international studies show that specialised nursing professionals are more careful in clinical diagnosis and casual therapy and possess more practical skills with regards to the health care of patients with leg ulcers 24, 25, 26, 27, 28 than non‐specialised nurses. The study by Clarke‐Moloney et al. shows a significant improvement of compression therapy as well as longer intervals between dressing changes with trained nurses 28. Therefore, these nurses are more effective in the care of patients with leg ulcers than non‐specialised nurses.
First analyses of knowledge and practical skills concerning compression therapy by nurses, doctors' assistants, physicians and therapists in general were published elsewhere 29. This study adds more data and is focused on the differences between users with specific expertise and users without specific expertise. The aim of the cross‐sectional observational survey is a comparison of the skills and knowledge of qualified nurses, doctors' assistants, physicians and physiotherapists and users with no further qualification. This comparison will provide information on whether further qualifications have an impact on knowledge and practical skills.
Methods
From October 2011 to April 2016, knowledge and practical skills of participants of workshops and seminars for compression therapy were evaluated nationwide. Therefore, the workshops and seminars were divided in those with a focus on basics in wound care (participants who had no specific expertise; NSE) and those with expertise [participants who already had further training (specific expertise; SE)]. The SE group included participants with further professional qualifications who received training for at least 50–70 lessons in wound management. In contrast, the group of NSE had no further specialisation in wound management.
Inclusion criteria
The participants (age > 18) included nurses (hospital, outpatient care and elderly care), doctors' assistants, physicians and physiotherapists who joined seminars on VLU and compression therapy. Participation in the study was independent of the objective of the learning unit, voluntary and not mandatory. The participants agreed, verbally and through their participation, to the non‐commercial and anonymous use of data.
Data collection
Based on a standardised guideline, four questions regarding the knowledge of current materials for compression therapy and their application were asked verbally and answered by the participants by show of hands. A compression bandage has to be upholstered with padding materials 30. Therefore, one question broached the issue of padding: ‘Did you learn the principles of upholstering and underpadding during your education?’ A follow‐up question examined if padding materials were prescribed when patients were treated with short‐stretch bandages: ‘Does the prescription of short‐stretch bandages include padding materials?’ Furthermore, two questions detected the knowledge of the users about multi‐component systems and ulcer stocking systems: ‘Are you familiar with multi‐component systems?’ and ‘Are you familiar with ulcer stocking systems?’ Two additional questions specified if and how often the participants use these products in their daily routine: ‘Do you use these products regularly every week?’ and ‘Do you use these products occasionally every 4–12 weeks?’ The last question evaluated commonly prescribed pressure values: ‘Which levels of pressure are prescribed for compression bandaging of patients with venous leg ulcers?’
Following the theoretical part of the seminar, participants alternately performed a practical test concerning compression bandaging with short‐stretch bandages. The generated pressures were measured and documented. The skills of the participants in performing compression bandaging were examined by measuring the achieved initial resting pressure after completion of compression bandaging. The device used, PicoPress® (Microlab Elettronica, Padova, Italy), is superior to other devices under the aspects of accuracy and reproducibility 31, 32. The PicoPress® sensor, which measures the interface pressure between the compression bandage and the skin, was placed at B1 21, 31. This is the region proximal to the inner ankle, which is recommended in studies for measuring the interface pressure 31, 33.
Compression therapy with short‐stretch bandages has a significant pressure drop in a short time 16, 22. To guarantee the strong pressure, which is needed for treatment of VLU, the participants were requested to achieve a pressure between 50 and 60 mmHg. Rosidal® K (Lohmann & Rauscher, Neuwied, Germany) and Pütterbinden® (Hartmann, Heidenheim, Germany) were used in this study. These short‐stretch bandages were applied via modified Sigg's technique. Depending on leg circumference, at least two short‐stretch bandages are required for this technique. A foam padding (Rosidal® soft; Lohmann & Rauscher) was applied above a tubular bandage (TG size 7; Lohmann & Rauscher). The first short‐stretch bandage starts at the big toe's joint and ends at the lower part of the calf. It covers the entire foot and wraps the leg in tightly rolled circular turns by overlapping the preceding layer by 1 cm. Then, the second short‐stretch bandage is applied in a figure‐of‐eight manner and ends shortly below the knee. Finally, the tubular bandage is now pulled over the entire bandaging and is attached to its end with tape 34.
Statistical analysis
Firstly, the analyses were evaluated descriptively. Open responses were categorised and summarised using qualitative methodologies. On the basis of the study design, missing data were not included. The pressure values with corresponding measures of central tendency are displayed by boxplot. Significant differences were analysed using a Chi‐squared test and t‐test. The Chi‐squared test was used when statistical requirements were satisfied 35. All data analyses were performed using IBM SPSS Statistics, Version 20·0.
Results
During a total of 62 seminars and workshops, all 1338 (90·7%) qualified wound experts with specific expertise (SE) participated in this study. A total of 138 (9·3%) participants who had no specific expertise (NSE) were examined in five further seminars and workshops. The majority of SE were nurses (91·6%; n = 1225). Most of them, 47·5% (n = 635), worked in outpatient care, 28·1% (n = 376) in hospital and 16·0% (n = 214) in elderly care. In addition, 4·9% (n = 65) were doctors' assistants and 3·6% (n = 48) physicians. Of the 138 participants, 55·1% (n = 76) with no further expertise (NSE) worked in hospitals, 38·4% (n = 53) in outpatient care and 6·5% (n = 9) in elderly care.
Knowledge and working practice about compression therapy
The majority of SE could not correctly respond to the questions regarding knowledge about products and methods of compression therapy as cited above. NSE participants showed a marginally higher proportion of unknowingness. About 13·6% of the SE participants were aware of ulcer stocking systems (versus NSE = 9·5%), and 10·0% knew multi‐component systems (versus NSE = 8·7%); 7·9% of the SE had learned to upholster compression bandaging during their education (versus NSE = 5·8%). However, the differences regarding the knowledge about products and methods in compression therapy between SE and NSE participants were not significant (multi‐component systems P = 0·535; ulcer stocking systems P = 0·172).
The knowledge about multi‐component systems (MC) and ulcer stocking systems (US) was best in SE within the group of physicians (n = 48) (MC = 33·3%; n = 16) and US = 56·3% (n = 27) and doctors' assistants (n = 65) [MC, US each = 23·1% (n = 15)] (Figure 1). SE nurses in hospitals (17·8%) and outpatient care (10·7%) had the highest knowledge about padding compared to the other professional SE groups. SE groups, like doctors' assistants, physicians and NSE nurses in elderly care, showed a lack of knowledge regarding padding (Figure 1).
Figure 1.
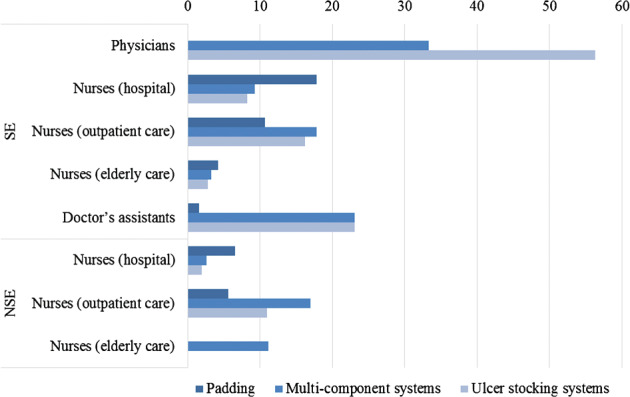
Knowledge of SE and NSE about current products and methods of compression therapy by professional groups in percent (SE: n = 1338; NSE: n = 138).
When asked about the prescription of short‐stretch bandages, significantly more SE reported a prescription of padding material than NSE (SE = 24·2%, NSE = 5·1%; P < 0·001). A total of 44·0% of SE and 14·3% of NSE nurses reported that physicians tend to prescribe padding materials when the benefit of these materials was explained to them. SE participants with knowledge about multi‐component systems worked with these products on a much more regular basis than NSE (SE = 78·4% and NSE = 33·3%; P = 0·002). A total of 32·1% of SE used multi‐component systems on a regular basis, and 46·3% used it occasionally. The proportion was lower in the group of NSE (8·3% regular basis and 25·0% occasionally). All participants in both groups who are aware of ulcer stocking systems also worked with them on a regular basis.
Concerning the question of which pressure values are prescribed for patients with compression bandaging of VLU, 89·1% of SE and 97·1% of NSE participants gave no specific answer. Further answers were: compression bandaging in Pütter technique, powerful or strong compression.
Pressure measurements
A total of 1107 of all participants (SE n = 972, NSE n = 135) performed compression bandaging with short‐stretch bandages by using the modified Sigg's technique. SE participants achieved an average level of pressure of 45·0 mmHg (median = 26·0; standard deviation = 24·6) and NSE 49·4 mmHg (median = 42·0; standard deviation = 28·7). However, these differences were not significant (P = 0·054) (Figure 2).
Figure 2.
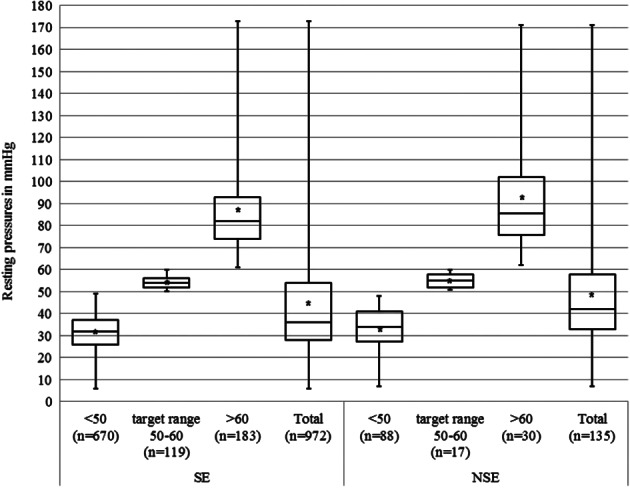
Resting pressure with short‐stretch bandages applied using Sigg's technique by SE (n = 972) and NSE (n = 135).
The target pressure value of 50–60 mmHg was achieved by 12·2 % (n = 119) of SE and 12·6 % (n = 17) of NSE. The majority of 68·9 % (n = 670) of SE and 65·2 % (n = 88) of NSE were below this target (<50 mmHg). Considering the resting pressure, the majority of SE participants achieved pressure values between 28 (lower percentile) and 54 mmHg (upper quantile) and the NSE participants between 33 (lower percentile) and 58 mmHg (upper quantile). In total, all participants achieved pressure values between 6 and 173 mmHg (SE) and between 7 and 171 mmHg (NSE) (Figure 2).
Discussion
A huge lack of knowledge and practical skills concerning compression therapy being performed by nurses, doctors' assistants, physicians and therapists with specific expertise in general have already been shown 29. Compared to the first publication, this study adds a significantly higher number of investigated cases and a comparison of users with specific expertise and users without specific expertise. The objective of this study was to show if there are differences in knowledge about certain aspects of compression therapy and performing compression bandaging between SE and NSE.
The results show that knowledge of the majority of SE and NSE from different professions was not up‐to‐date according to the latest standards for compression materials, methods or their usage. However, it could be shown that health care professionals with further professional qualifications in wound care management have a partially higher level of knowledge and practical skills in compression therapy compared to health care professionals without these qualifications. Significant differences between SE and NSE can be shown in the use of multi‐component systems and padding materials.
Multi‐component systems and ulcer stocking systems are available for more than 15 years. Their composition, the possibilities and necessities of their application and their mechanisms and impact have been thoroughly researched 5, 10, 16, 17. Nevertheless, under 10% of health care givers are aware of these systems. Furthermore, the study has shown that the majority of participants (up to 90%), regardless of expertise, were not able to reach the target pressure range of 50–60 mmHg.
Nevertheless, compared to other studies, we cannot confirm that SE is more effective in the care of patients with leg ulcers than non‐specialised nurses 24, 25, 26, 27, 28. However, we equally found a huge gap between state‐of‐the‐art knowledge and daily practice of SE and NSE. The health care givers do not have enough knowledge about compression therapy or do not use up‐to‐date materials in their daily professional practice, even though professional magazines and journals report regularly on modern methods and utilities.
The lack of knowledge about certain aspects of compression therapy and performing compression bandaging has been shown in other international studies, independent of the participants' professions 22, 23. It is also reflected in the low number of patients with VLU who received compression therapy (40 %) in Germany 10. In accordance with the legal requirement that health care has to be based on guidelines and according to latest scientific knowledge, there is an urgent need for information on compression therapy.
An increase in knowledge regarding material and use and improved skills in compression bandaging may shorten healing time and thus affect the quality of life positively. The acquisition of theoretical knowledge by the professionals may be the basis for adequate compression therapy. However, this study shows that even further qualified carers lack basic knowledge concerning up‐to‐date materials and methods of compression therapy. This implies that qualifications do not always guarantee expertise. In Germany, the practice of compression bandaging is not taught in university medical training. The curricula for nurses' education differ nationwide. On average, 1–2 lessons are spent on this topic 34. This should be completed by practicing with pressure‐measuring devices on a regular basis. The use of these instruments is currently the most practical method for determining the value of interface pressure. Appropriate exercises should be mandatorily offered to all professional groups who perform compression bandaging. The use of pressure‐measuring devices for training is considered a viable way to practice the achievement of predetermined pressure values 31, 36. It should become part of the curricula of physicians and nurses and also part of daily routine. Also, establishing training sessions should be considered for all carers, even the further qualified, who are natural teachers for new staff. The so‐called adaptive compression bandages may be an alternative option. The easy handling of these bandages allows the carer, the patient or relatives to adjust the pressure after a short training session 37.
Furthermore, a number of limitations has to be discussed. It should be considered that a vastly higher number of SE participated in this study. Therefore, significant differences in usage of multi‐component systems cannot be analysed. The non‐anonymous questioning by raising hands was chosen because of time constraints and practical reasons. Therefore, social sanctions and social desirability may have influenced the outcome. This includes a possible limitation of participation or willingness, which could influence the response of the participants (response bias). Furthermore, health care givers with a greater interest in wound care management have a higher willingness to participate. Therefore, it must be concluded that knowledge and practical skills in compression therapy are much lower than expected.
Acknowledgements
The authors thank Marie Christine Duval, Pia Dahlhoff and Mario Gehoff who are a part of the scientific communication team of the IVDP for copy editing.
MA has served as consultant and/or paid speaker for and/or has received research grants and/or honoraries for consulting and/or scientific lectures for and/or has had travel expenses reimbursed and/or participated in clinical trials sponsored by companies including 3M, AOK Bundesverband, Bayer Healthcare, Beiersdorf, Birken, Bode, B. Braun, BSN, BVmed, Coloplast, DAK, Diabet concept, Gerromed, GlaxoSmithKline, Johnson&Johnson, Lohmann&Rauscher, Medi, Medovent, Mölnlycke, Smith&Nephew, Schülke&Mayr, Söring, Sorbion, Systagenix and Urgo.
KP has received fees for consultations and/or presentations for the following companies: 3M Medica, BSN medical, Paul Hartmann AG, Lohmann & Rauscher, URGO, Smith & Nephew, Bauerfeind, medi.
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
KH has no conflict of interests.
References
- 1. DGfW Deutsche Gesellschaft für Wundheilung und Wundbehandlung e.V . Lokaltherapie chronischer Wunden bei Patienten mit den Risiken periphere arterielle Verschlusskrankheit, Diabetes mellitus, chronische venöse Insuffizienz [Internet]. 2012. URL http://www.awmf.org/uploads/tx_szleitlinien/091‐001l_S3_Lokaltherapie_chronischer_Wunden_2012‐verlaengert.pdf [accessed 2 August 2016].
- 2. Dissemond J. Differentialdiagnosen des Ulcus cruris venosum. Phlebologie 2011;40:85–92. [Google Scholar]
- 3. Heyer K, Herberger K, Protz K, Glaeske G, Augustin M. Epidemiology of chronic wounds in Germany: analysis of statutory health insurance data. Wound Repair Regen 2016;24:434–42. [DOI] [PubMed] [Google Scholar]
- 4. Rabe E, Pannier‐Fischer E, Bromen K, Schuldt K, Stang A, Poncar C, Wittenhorst M, Bock E, Weber S, Jöckel KH. Bonner venenstudie der deutschen gesellschaft für phlebologie: epidemiologische untersuchungen zur frage der häufigkeit und ausprägung von chronischen venenkrankheiten in der städtischen und ländlichen wohnbevölkerung. Phlebologie 2003;32:1–14. [Google Scholar]
- 5. Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous leg ulcer: incidence und prevalence in the elderly. J Am Acad Dermatol 2002;46:381–6. [DOI] [PubMed] [Google Scholar]
- 6. Nelzen O, Bergqvist D, Lindhagen A. Venous und non‐venous leg ulcers: clinical history und appearance in a population study. Br J Surg 1994;81:182–7. [DOI] [PubMed] [Google Scholar]
- 7. Wipke‐Tevis DD, Rantz MJ, Mehr DR, Popejoy L, Petroski G, Madsen R, Conn VS, Grando VT, Porter R, Maas M. Prevalence, incidence, management, und predictors of venous ulcers in the long‐term‐care population using the MDS. Adv Skin Wound Care 2000;13:218–24. [PubMed] [Google Scholar]
- 8. Heinen MM, van Achterberg T, op Reimer WS, van de Kerkhof PC, Laat E. Venous leg ulcer patients: a review of the literature on lifestyle and pain‐relates interventions. J Clin Nurs 2004;13:355–66. [DOI] [PubMed] [Google Scholar]
- 9. Registered Nurses Association of Ontario (RNAO) . Assessment and management of venous leg ulcers [Internet]. 2004. URL http://rnao.ca/sites/rnao‐ca/files/Assessment_and_Mangement_of_Venous_Leg_Ulcers.pdf. [accessed on 2 August 2016].
- 10. Heyer K, Protz K, Glaeske G, Augustin M. Epidemiology and use of compression treatment in venous leg ulcers: Nationwide claims data analysis in Germany. Int Wound J 2017;14:338–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O'Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012;11:CD000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moffatt C. Variability of pressure provided by sustained compression. Int Wound J 2008;5:259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nelson EA, Cullum N, Jones J. Venous leg ulcers. Clin Evid 2006;15:2607–26. [PubMed] [Google Scholar]
- 14. Partsch H. Compression therapy of venous ulcers. Curr Probl Dermatol 2006;27:130–40. [DOI] [PubMed] [Google Scholar]
- 15. Keller A, Müller ML, Calow T, Kern IK, Schumann H. Bandage pressure measurement and training: simple interventions to improve efficiency in compression bandaging. In Wound J 2009;6:324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Robson MC, Cooper DM, Aslam R, Gould LJ, Harding KG, Margolis DJ, Ochs DE, Serena TE, Snyder RJ, Steed DL, Thomas DR, Wiersma‐Bryant L. Guidelines for the treatment of venous leg ulcers. Wound Repair Regen 2006;14:649–62. [DOI] [PubMed] [Google Scholar]
- 17. Haute Autorité de Santé (HAS) . Clinical practice guidelines: managing venous leg ulcers (excluding dressings) [Internet]. 2006. URL http://www.has‐sante.fr/portail/upload/docs/application/pdf/managing_venous_leg_ulcers_‐_guidelines.pdf. [accessed 2 August 2016]
- 18. Jünger M, Ladwig A, Bohbot S, Haase H. Comparison of interface pressures of three compression bandaging systems used on healthy volunteers. J Wound Care 2009;18:476–80. [DOI] [PubMed] [Google Scholar]
- 19. World Union of Wound Healing Societies (WUWHS) . Prinzipien der Best Practice: Kompression beim venösen Ulcus cruris. Ein Konsensusdokument. London: MEP Ltd, 2008. [Google Scholar]
- 20. Larsen AM, Futtrup I. Watch the pressure – it drops. EWMA J 2004;4:8–12. [Google Scholar]
- 21. Partsch H, Clark M, Mosti G, Steinlechner E, Schuren J, Abel M, Benigni JP, Coleridge‐Smith P, Cornu‐Thénard A, Flour M, Hutchinson J, Gamble J, Issberner K, Juenger M, Moffatt C, Neumann HA, Rabe E, Uhl JF, Zimmet S. Classification of compression bandages: practical aspects. Dermatol Surg 2008;34:600–9. [DOI] [PubMed] [Google Scholar]
- 22. Stansal A, Lazareth I, Michon Pasturel U, Ghaffari P, Boursier V, Bonhomme S, Sfeir D, Priollet P. Compression therapy in 100 consecutive patients with venous leg ulcers. J Mal Vasc 2013;38:252–8. [DOI] [PubMed] [Google Scholar]
- 23. Coull A, Tolson D, McIntosh J. Class‐3c compression bandaging for venous ulcers: comparison of spiral and figure‐of‐eight techniques. J Adv Nurs 2006;54:274–83. [DOI] [PubMed] [Google Scholar]
- 24. Adderley UJ, Thompson C. A comparison of the management of venous leg ulceration by specialist and generalist community nurses: a judgement analysis. Int J Nurs Stud 2016;53:134–43. [DOI] [PubMed] [Google Scholar]
- 25. Thompson C, Adderley U. Diagnostic and treatment decision making in community nurses faced with a patient with possible venous leg ulceration: a signal detection analysis. Int J Nurs Stud 2015;52:325–33. [DOI] [PubMed] [Google Scholar]
- 26. Benoiton LA, Schmidt E, Tarr GP, Thomson IA, Rennie SC, van Rij AM. Assessment and management of leg ulcers in the community and an outpatient clinic. N Z Med J 2013;126:26–34. [PubMed] [Google Scholar]
- 27. Patton LR. Are community leg ulcer clinics more cost‐effective than home care visits? J Wound Care 2009;18:49–52. [DOI] [PubMed] [Google Scholar]
- 28. Clarke‐Moloney M, Keane N, Kavanagh E. Changes in leg ulcer management practice following training in an Irish community setting. J Wound Care 2008;17:118–21. [DOI] [PubMed] [Google Scholar]
- 29. Protz K, Heyer K, Dorler M, Stucker M, Hampel‐Kalthoff C, Augustin M. Compression therapy: scientific background and practical applications. J Dtsch Dermatol Ges 2014;12:794–801. [DOI] [PubMed] [Google Scholar]
- 30. Wounds International . Principles of Compression in Venous Disease: a Practitioner's Guide to Treatment and Prevention of Venous Leg Ulcers. London: Wounds International, 2013. [Google Scholar]
- 31. Partsch H, Clark M, Bassez S, Benigni JP, Becker F, Blazek V, Caprini J, Cornu‐Thénard A, Hafner J, Flour M, Jünger M, Moffatt C, Neumann M. Measurement of lower leg compression in vivo: recommendations for the performance of measurements of interface pressure and stiffness: consensus statement. Dermatol Surg 2006;32:224–32. [DOI] [PubMed] [Google Scholar]
- 32. Partsch H. Practical value of measuring compression pressure. Dermatol Surg 2010;36:1941. [DOI] [PubMed] [Google Scholar]
- 33. Partsch P. Review compression therapy in leg ulcers. Rev Vasc Med 2013;1:9–14. [Google Scholar]
- 34. Protz K. Moderne Wundversorgung. München: Elsevier GmbH, 2014. [Google Scholar]
- 35. Camilli G, Hopkins KD. Testing for association in 2x2 contigency tables with very small sample sizes. Psychol Bull 1979;86:1011–4. [Google Scholar]
- 36. Partsch H, Mosti G. Comparison of three portable instruments to measure compression pressure. Int Angiol 2010;29:426–30. [PubMed] [Google Scholar]
- 37. Damstra RJ, Partsch H. Prospective, randomized, controlled trial comparing the effectiveness of adjustable compression velcro wraps versus inelastic multicomponent compression bandages in the initial treatment of leg lymphedema. J Vasc Surg Vein Lymph Dis 2013;1:13–9. [DOI] [PubMed] [Google Scholar]


