Abstract
Varicose veins (VVs) and varicose ulceration (VU) are usually considered non‐life‐threatening conditions, but in some cases they can lead to major complications such as fatal bleeding. The aim of this systematic review is to evidence the most updated information on bleeding from VV and VU. As evidence acquisition, we planned to include all the studies dealing with “Haemorrhage/Bleeding” and “VVs/VU”. We excluded all the studies, which did not properly fit our research question, and with insufficient data. As evidence synthesis, of the 172 records found, after removing of duplicates, and after records excluded in title and abstract, 85 matched our inclusion criteria. After reading the full‐text articles, we decided to exclude 68 articles because of the following reasons: (1) not responding properly to our research questions; (2) insufficient data; the final set included 17 articles. From literature searching, we identify the following main issues to be discussed in the review: epidemiology and predisposing factors, pathophysiology and forensic aspects, first aid.
It has been estimated that deaths for bleeding due to peripheral venous problems account up to 0.01% of autopsy cases. From a pathological point of view, venous bleeding may arise from either acute or chronic perforation of an enlarged vein segment through the weakened skin. From a forensic point of view, in cases of fatal haemorrhage the death scene can even simulate non‐natural events, due to crime or suicide. In most cases, incorrect first aid led to fatal complications. Further investigation on epidemiology and prevention measures are needed.
Keywords: bleeding, haemorrage, varicose ulceration, varicose veins
1. INTRODUCTION
Chronic venous disease (CVD) is a clinical condition affecting up to 80% of adult population in western countries.1, 2 Varicose veins (VVs) and varicose ulceration (VU) are clinical manifestation of CVD1, 3 and, although VV and VU are usually considered non‐life‐threatening, in some cases they can lead to major complications such as severe and fatal bleeding.4, 5 In fact, up to 1/1000 autopsy cases for sudden and unexpected death may be due to hemorrage from the aformentioned venous problems.6 Also, from a forensic point of view, in case of fatal hemorrhage from venous complications, the death scene can even simulate non‐natural events, due to crime or suicide, for the massive traces of blood that can be present in these occasions.7
The aim of this systematic review is to evidence the most updated information on bleeding from VV and VU.
2. MATHERIALS AND METHODS
This review was conducted and is reported in accordance with the PRISMA guidelines.8
2.1. Inclusion and exclusion criteria
We planned to include all the studies dealing with haemorrhage originating from VVs and VU. We excluded all the studies, which did not properly fit our research question, and with insufficient data.
2.2. Search strategy
Two members of the research team (R.S. and N.I.) performed a comprehensive literature research using terms identified and agreed by the authors. Medline, and Scopus database were searched, without time limit, using the following keywords: “Haemorrhage/Bleeding” and “varicose veins/varicose ulceration.” We also reviewed the reference lists of retrieved studies to identify studies that had not been identified by the search strategy.
2.3. Data extraction and risk of bias assessment
Two review authors (G.D.M. and S.d.F.) independently assessed both titles and abstracts of 139 Medline + 33 Scopus potentially eligible studies. In case of ambiguous or unclear result, the study was retrieved in full and assessed further by all review authors independently and included if pertinent. All studies were assessed by using the Downs and Black quality checklist9: this system is a well validated, reliable, and methodologically strong tool.10
3. RESULTS
3.1. Study selection
Of the 172 records found, after removing of duplicates, and after records excluded in title and abstract, 85 matched our inclusion criteria (Fig. 1). After reading the full‐text articles, we decided to exclude 68 articles because of the following reasons: (1) not responding properly to our research questions; (2) insufficient data; The final set included 17 articles.
Figure 1.
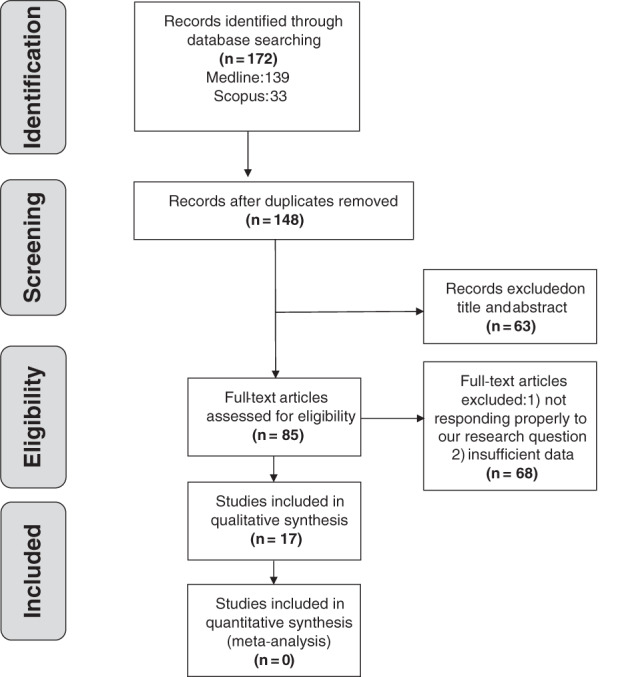
Flow diagram of study inclusion
From literature searching, we found the following main issues: epidemiology and predisposing factors, pathophysiology and forensic aspects, first aid.
3.1.1. Epidemiology and predisposing factors
Little less than 70 cases of venous bleeding has been reported in the scientific literature in the past 50 years.4, 5, 6, 7, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22 It has been estimated that deaths for bleeding due to peripheral venous problems account up to 0.01% of autopsy cases.6, 17, 22 This kind of bleeding is probably underestimated due to the scarcity of reports in the current literature.18 Victims are in general elderly people, usually in their sixth to ninth decades of life, especially if they live isolated, in fact the victims are often found in their homes where they had been alone at the time of death. Although venous problems of the legs are more common in females,1, 2 there is no correlation of the bleeding event with gender or laterality of the lesions.21, 23 Concomitant medical conditions, such as arthritis or weakness from cerebrovascular disease may also predispose to this kind of problem, as these conditions may affect mobility and reactivity of patients.6, 21, 22, 24 Anticoagulant drugs and skin fragility may also contribute to bleeding24, 25 and concomitant cardiovascular disease, such as ischemic heart disease, may contribute to the fatal ending of the bleeding episode that happens for subsequent hypovolemic shock. Also, alcohol abuse may enhance the speed of bleeding due to peripheral vasodilation.6, 22, 24
3.1.2. Pathophysiology and forensic aspects
From a pathological point of view, venous bleeding may arise from either acute perforation of an enlarged vein segment through an overlying weakened skin layer or from an exacerbation of a VU followed by erosion of an underlying enlarged vein. In this context two types of ulceration related to venous hemorrhage have been described: the acute perforative type (APT) and the chronic ulcerative type (CUT).4, 5, 6, 7, 15, 21 The APT is a small (<5 mm) , shallow lesion with slight adjacent cutaneous pigmentation or eczema, according to C4a clinical stage. The CUT is a greater lesion (>5 mm, usually 10‐100 mm) and occurs from large deeper ulcers associated with considerable skin pigmentation and induration with subcutaneous fibrosis according to C4b‐C6 clinical stages that are present in long lasting, serious chronic venous insufficiency (CVI). The VU, in this context, may erode the superficial surface of an underlying vein determining subsequent bleeding.1, 4, 5, 15 The hemorrhage may be spontaneous, with no history of trauma, in most cases, or sometimes may be a consequence of a minor trauma. The localization of a VV above a bone prominence (e.g. the medial malleolar site) may represent a mechanical factor for vein lesion.5, 6, 21, 23 The sclerotic alterations of the vein wall of patients with CVI may also enhance the susceptibility of these vessels.7 In fact, atrophy of the overlying skin, which can be encountered from clinical stage C4, predisposes to skin breakage that concomitantly with ischemic necrosis of the vein wall due also to venous hypertension in CVD produces also a tear in the vein wall with consequent bleeding.1, 6
In fatal cases, the bleeding may be so marked, due to the underlying venous ipertension condition in patients with advanced CVD, that can be even mistaken for arterial hemorrage and leads rapidly to a loss of consciousness and subsequent death, usually in a time lapse between 5 and 20 minutes.20, 21, 23
Autopsy evaluation must be performed with careful layer dissection of the area of hemorrhage to demonstrate ruptured VV and to enable directed histologic examination of the type of ulcers that caused the bleeding. Analysis of the subcutaneous tissues will evidence the presence of dermal fibrosis and hemosiderin staining in case of advanced CVI.6 Furthermore, bloodstain pattern analysis will evidence large stains (13‐22 cm) due to the fact that venous blood escapes under much lower pressure than arteries and it tends to pool until gravitational forces action exceed the surface tension of the blood, thus producing spherical droplets in free fall forming circular stains upon their impact with the floor.17
3.1.3. First aid
Unfortunately, advice regarding haemostatic control is not routinely provided to VV patients. In fact, in most cases death could have been easily prevented by correct application of basic first‐aid techniques.19, 20
To stop the bleeding, with the patient in the lied down position, two simple gestures are required: to elevate the affected leg pressing the bleeding point in order to ease or cease the bleeding and to apply a tourniquet, or compressive bandages, distally to the point of bleeding.19, 20, 21 Soon after appropriate management should be provided in hospital setting.14, 21
Often, if the venous bleeding is misinterpreted as arterial bleeding, the patient may apply incorrectly the ligature proximally above the bleeding point, closer to the heart, or may stand in the upright position, thus exacerbating the bleeding.20
4. DISCUSSION
Varicose veins are a common sign of CVD with a prevalence up to 56% in men and 73% in woman.1, 2, 22, 26 Among the complications of VV, especially in elderly that have the skin more fragile than younger,25, 27 severe bleeding may be encountered in clinical practice and this can be fatal, especially in presence of comorbidities such as ischemic heart disease.6, 22, 24, 27 In physiological conditions and in case of traumatic haemorrage, as the venous system is under low pressure, the coagulation via the coagulation cascade occur spontaneously and rapidly than the arterial system.19 But, if we consider an haemorrage event occurring on a ruptured VV, the bleeding may me massive and the patient could die in less than 20 minutes. This is due to the sclerotic changes and the skin changes occurring respectively in vein wall and skin and subcutaneous tissue that characterize CVD.1, 4, 5, 6, 15, 21, 23 The early skin changes (light pigmentation and eczema) occurring in C4a clinical stage,1 under the venous hypertension, may be responsible of the formation of a small chronic ulcer (<5 mm), connected with a slcerotic varicose superficial vein that can spontaneously rupture and initiate bleeding. In case of more advanced clinical stage of CVD, especially in presence of VU, a larger chronic ulcerative wound (>5 mm, usually 10‐100 mm), connected with superficial but even deeper veins, may start the bleeding.1, 4, 5, 15 As the patients with fatal haemorrage are often found in a pool of blood the death scen may simulate even suicide or crime, so this clinical event is also important from a forensic point of view.7 Therefore, in order to exclude these non‐natural causes of death a meticolous examination of the body and of the point of bleeding must be carried out,6, 7, 15, 16, 17, 21, 23, 24 and at the same time the analysis of the blood stain pattern is also pivotal.17
The victims of fatal bleeding are often elderly subjects living alone, where there is nobody to provide assistance when the wound begins to bleed and furthermore, the first aid tentatives performed by the patient are not even correct such as bandaging proximally or standing in upright position that cause an increase in venous return stimulating even more the bleeding. In fact, correct first aid consists of getting the patients in the lie down position, elevating the affected leg and applying compression by means of bandages or a tourniquet distally beneath the bleeding point.19, 20, 21
Despite the commonplace that VV and VU are benign complications of CVD, this review showed there have been several cases of massive hemorrhage due to this conditions that can became life‐threatening with fatal results. Further investigations in the area of epidemiology and prevention are needed in order to better quantify the real incidence of this threatening events and to better provide prevention and care.
Conflict of interest
The authors have no conflict of interests to declare.
Financial disclosures
This article received no funding.
Serra R, Ielapi N, Bevacqua E, et al. Haemorrhage from varicose veins and varicose ulceration: A systematic review. Int Wound J. 2018;15:829–833. 10.1111/iwj.12934
The first two authors contributed equally to this work.
REFERENCES
- 1. Serra R, Grande R, Butrico L, Fugetto F, de Franciscis S. Epidemiology, diagnosis and treatment of chronic venous disease: a systematic review. Chirurgia. 2016;29(2):34‐35. [Google Scholar]
- 2. Serra R, Buffone G, de Franciscis A, et al. A genetic study of chronic venous insufficiency. Ann Vasc Surg. 2012;26(5):636‐642. [DOI] [PubMed] [Google Scholar]
- 3. Serra R, Butrico L, Ruggiero M, et al. Epidemiology, diagnosis and treatment of chronic leg ulcers: a systematic review. Acta Phlebolol. 2015;16(1):9‐18. [Google Scholar]
- 4. Fragkouli K, Mitselou A, Boumba VA, Siozios G, Vougiouklakis GT, Vougiouklakis T. Unusual death due to a bleeding from a varicose vein: a case report. BMC Res Notes. 2012;5:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Evans GA, Evans DM, Seal RM, Craven JL. Spontaneous fatal haemorrhage caused by varicose veins. Lancet. 1973;2(7842):1359‐1361. [DOI] [PubMed] [Google Scholar]
- 6. Byard RW, Gilbert JD. The incidence and characteristic features of fatal hemorrhage due to ruptured varicose veins: a 10‐year autopsy study. Am J Forensic Med Pathol. 2007;28(4):299‐302. [DOI] [PubMed] [Google Scholar]
- 7. Doberentz E, Hagemeier L, Veit C, Madea B. Unattended fatal haemorrhage due to spontaneous peripheral varicose vein rupture‐‐two case reports. Forensic Sci Int. 2011;206(1–3):e12‐e16. [DOI] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264‐269. W64. [DOI] [PubMed] [Google Scholar]
- 9. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377‐384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Collaborating Centre for Methods and Tools (2008). Quality Checklist for Health Care Intervention Studies. Hamilton, ON: McMaster University. (Updated June 1, 2010). Retrieved from http://www.nccmt.ca/resources/search/9. Accessed July 11, 2017.
- 11. Batman LS, Slovin I. An unusual cause of stillbirth: maternal hemorrhage from ankle varicosity. Del Med J. 1975;47(8):427‐428. [PubMed] [Google Scholar]
- 12. du Toit DF, Knott‐Craig C, Laker L. Bleeding from varicose vein – still potentially fatal. A case report. S Afr Med J. 1985;67(8):303. [PubMed] [Google Scholar]
- 13. Wigle RL, Anderson GV Jr. Exsanguinating hemorrhage from peripheral varicosities. Ann Emerg Med. 1988;17(1):80‐82. [DOI] [PubMed] [Google Scholar]
- 14. McCarthy WJ, Dann C, Pearce WH, Yao JS. Management of sudden profuse bleeding from varicose veins. Surgery. 1993;113(2):178‐183. [PubMed] [Google Scholar]
- 15. Morrow PL, Hardin NJ, Karn CM, Beloin R, McDowell RW. Fatal hemorrhage caused by varicose veins. Am J Forensic Med Pathol. 1994;15(2):100‐104. [DOI] [PubMed] [Google Scholar]
- 16. Racette S, Sauvageau A. Unusual sudden death: two case reports of hemorrhage by rupture of varicose veins. Am J Forensic Med Pathol. 2005;26(3):294‐296. [DOI] [PubMed] [Google Scholar]
- 17. Byard RW, Veldhoen D, Manock C, Gilbert JD. Blood stain pattern interpretation in cases of fatal haemorrhage from ruptured varicose veins. J Forensic Leg Med. 2007;14(3):155‐158. [DOI] [PubMed] [Google Scholar]
- 18. Tollefsen I. Fatal haemorrhage from a varicose vein: a case report from 50 years ago. EJVES Extra. 2007;13:60‐61. [Google Scholar]
- 19. Cocker DM, Nyamekye IK. Fatal haemorrhage from varicose veins: is the correct advice being given? J R Soc Med. 2008;101(10):515‐516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hejna P. A case of fatal spontaneous varicose vein rupture‐‐an example of incorrect first aid. J Forensic Sci. 2009;54(5):1146‐1148. [DOI] [PubMed] [Google Scholar]
- 21. Jelev L, Alexandrov A. A case of fatal bleeding from acute varicose leg ulcer: clinic‐pathological characteristics. EJVES Extra. 2011;21:e33‐e35. [Google Scholar]
- 22. Ampanozi G, Preiss U, Hatch GM, et al. Fatal lower extremity varicose vein rupture. Leg Med (Tokyo). 2011;13(2):87‐90. [DOI] [PubMed] [Google Scholar]
- 23. Aquila I, Sacco MA, Gratteri S, Di Nunzio C, Ricci P. Sudden death by rupture of a varicose vein: case report and review of literature. Med Leg J. 2017;85(1):47‐50. [DOI] [PubMed] [Google Scholar]
- 24. Gilbert JD, Byard RW. Ruptured varicose veins and fatal hemorrhage. Forensic Sci Med Pathol. 2017. in press. 10.1007/s12024-017-9897-y. [DOI] [PubMed] [Google Scholar]
- 25. Serra R, Ielapi N, Barbetta A, de Franciscis S. Skin tears and risk factors assessment: a systematic review on evidence‐based medicine. Int Wound J. 2018;15(1):38‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Beebe‐Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175‐184. [DOI] [PubMed] [Google Scholar]
- 27. Nikolić S, Zivković V. Bloodstain pattern in the form of gushing in a case of fatal exsanguination due to ruptured varicose vein. Med Sci Law. 2011;51(1):61‐62. [DOI] [PubMed] [Google Scholar]


