Abstract
In our hospital, an adverse event reporting system was initiated that alerts the plastic surgery department immediately after suspecting contrast media extravasation injury. This system is particularly important for a large volume of extravasation during power injector use. Between March 2011 and May 2015, a retrospective chart review was performed on all patients experiencing contrast media extravasation while being treated at our hospital. Immediate treatment by squeezing with multiple slit incisions was conducted for a portion of these patients. Eighty cases of extravasation were reported from approximately 218 000 computed tomography scans. The expected extravasation volume was larger than 50 ml, or severe pressure was felt on the affected limb in 23 patients. They were treated with multiple slit incisions followed by squeezing. Oedema of the affected limb disappeared after 1–2 hours after treatment, and the skin incisions healed within a week. We propose a set of guidelines for the initial management of contrast media extravasation injuries for a timely intervention. For large‐volume extravasation cases, immediate management with multiple slit incisions is safe and effective in reducing the swelling quickly, preventing patient discomfort and decreasing skin and soft tissue problems.
Keywords: Complications, Contrast Media, Extravasation, Tomography
Introduction
Extravasation injury is the accidental administration of a desiccant or vesicant solution into the tissue rather than the intention installation into the vessel 1. The reported incidence of extravasation injury is 0·1–6·5% in the general population, 11% in general paediatric patients and 0·5–22% in patients treated using chemotherapy 2, 3, 4, 5. The incidence of radiographic contrast media (CM) extravasation is increasing with more widespread use of computed tomography (CT). A large volume of CM extravasation can occur because of the use of a power CM injector. A published report estimated the incidence of CM extravasation to be approximately 0·45% during power injector use, and more recently, a large study from the USA reported a 0·7% rate of CM extravasation incidence (475 cases of nearly 70 000 CT procedures performed) 6, 7. In our hospital, an adverse event reporting system was initiated that alerts the plastic surgery (PS) department immediately after suspecting CM extravasation injury from CT scanning. This system has enabled the timely assessment and proper care of each extravasation case. This is particularly important for a relatively large volume of extravasation or if the patient feels severe pressure on the affected limb. In such instances, multiple slit incisions are made in the affected limbs, permitting the quick removal of extravasated CM.
Materials and methods
The current study was approved by the Institutional Review Board (IRB) of our medical institution (IRB approval number: AJIRB‐MED‐MDB‐15‐471).
Between March 2011 and May 2015, a retrospective chart review was performed on all patients experiencing extravasation while being treated at Ajou University Hospital. A total of 603 patients were included who had suffered extravasation injury from any type of fluid. Of these, 80 patients experienced CM extravasation. Patient records were retrospectively evaluated for age, gender, anatomical location of extravasation, type and volume of extravasated agent, needle gauge, flow rate of power injector, kind of treatment and the resulting complications. In terms of the volume of extravasated agent, after stopping the power injector immediately after identification of the extravasation, we recorded the injected volume (original volume of the CM – remaining volume of the CM). We substituted this injected volume as ‘expected extravasation volume’.
Drainage of extravasated CM with multiple slit incisions was conducted for a portion of these patients (Figure 1). In detail, the intravenous catheter used for CM injection was removed, and the area near the catheter insertion was disinfected with povidone iodine solution. Multiple slit incisions (usually 5–10 incisions) 2–3 mm long were made near the catheter insertion site with a size‐11 sterile blade, carefully avoiding visible vessels. The affected limb was then squeezed toward the slit incisions, and squeezing was continued until no more CM drained out, and the patient felt relieved of the pressure. The wound area was covered with an aseptic dressing with light compression. Patients were advised to elevate the affected site. For further drainage of the remaining CM, the incisions were not sutured. The status of the incision site was checked the following day and during the next 2–14 days by office visits.
Figure 1.

Multiple slit incision procedure. (A) Drainage of extravasated contrast media (CM) with multiple slit incisions. (B) Multiple slit incisions, 2–3 mm in size, were made near the catheter insertion site with a number‐11 blade, carefully avoiding visible vessels. The affected limb was then squeezed toward the slit incisions, with squeezing continued until no more CM drained out, and the patient felt relieved of the pressure. (C) Oedema of the affected limb disappeared within 1–2 hours of treatment.
Results
Over a 4‐year period, in our hospital, 80 cases of CM extravasation were reported from approximately 218 000 CT scans using an intravenous contrast agent, representing an incidence rate of 0·036%. The mean age of the 80 patients (52 women, 28 men) was 58 years at the time of diagnosis (range 2–94 years). Figure 2 shows the incidence of the CM extravasation by age. The most common anatomical locations of extravasation were the forearm area (right: 28, left: 34), followed by the dorsum of the hand (right: 11, left: 5) and two other sites. Five different brands of non‐ionic contrast agents were given in all the cases, Bonorex (Central Medical Service, Seoul, Korea), Omnihexol (Korea United Pharm, Seoul, Korea), Optiray (Reyon Phram, Seoul, Korea), Scanlux (Dasol Life Science, Seoul, Korea) and Iomeron (Bracco Imaging Korea, Seoul, Korea). The injected flow rates ranged from 0·6 to 5 ml/second. In all cases, a power CM injector was used. The mean gauge of needles for the power injector was 20·2 (range 18–24). Mean volume of the extravasated agent was 44·5 ml (range 5–140 ml). The mean flow rate of the power CM injector was 2·8 ml/second (range 0·6–5 ml/second). The expected extravasation volume was less than 50 ml for 57 patients. They were treated conservatively using light compression, elevation of the affected limb and pain control. Additionally, hyaluronidase injection after initiating the conservative care was performed for 12 cases. The expected extravasation volume was larger than 50 ml, or severe pressure was felt on the affected limb without a sign of compartment syndrome in 23 patients. They were treated with multiple slit incisions followed by squeezing. In these cases, oedema of the affected limb disappeared after 1–2 hours after treatment, and the skin incisions healed within a week (average of 6·3 days). Scars were not remarkable after the wounds healed, and there were no reported case of wound infection. There were five cases of minor complications, which included bullae formation and epidermolysis. Two of these were had been treated with multiple slit incisions, and three cases had received conservative management. These wound problems were spontaneously resolved without a surgical procedure being necessary.
Figure 2.
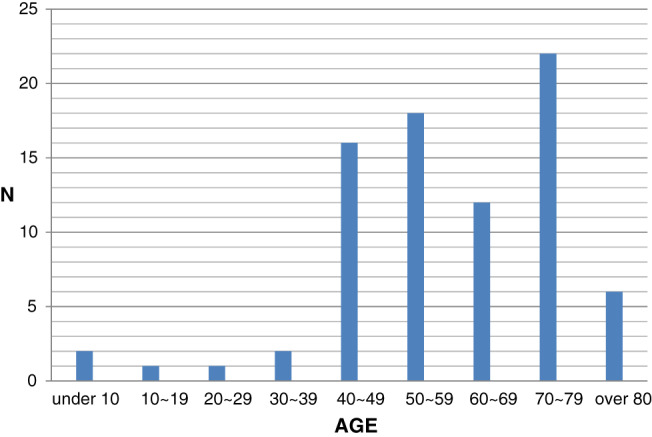
The incidence of the contrast media extravasation by the age.
Discussion
All extravasation injuries require immediate attention with prompt evaluation and appropriate treatment. Each hospital should prepare a protocol that can deal with a suspected extravasation case promptly, efficiently and systematically. Clinical sequelae of extravasation injury vary from temporary inflammatory response to severe tissue damage as it can produce soft tissue necrosis that requires surgical intervention. Tissue necrosis is dependent on the volume and toxicity of the substance that has extravasated. There have been reports of subsequent soft tissue loss, scarring, secondary wound infection, abscess formation, tissue adhesion, contracture of affected limbs and amputations 1, 8.
With the advent and rise in use of low‐osmolar non‐ionic CM in the past decade, soft tissue complications associated with CM extravasation injury have decreased 9. Extravasation of non‐ionic CM reportedly causes less necrosis, oedema and haemorrhage than conventional ionic CM 10. Non‐ionic CM has been reported to result in significantly fewer gross morphological changes and lesser local histological necrosis than conventional CM 11. Although most CM extravasation injuries do not have long‐term consequences, with minimal or no adverse effects, there is concern about relatively larger volumes of CM being rapidly injected with a power CM injector. One study reported that 58% of CM extravasation was associated with large volumes of extravasated CM exceeding 50 ml 9.
The optimum treatment strategy is not yet clear, although elevation of the affected limb, ice or warm packs and hyaluronidase injection are in general use 2, 6. Hyaluronidase is an enzyme that breaks down the interstitial barriers in the connective tissue by disrupting the interstitial polysaccharide bonds that normally hold cells together. This promotes the removal of extravasated material by the lymphatics and capillaries 12. It is generally accepted that hyaluronidase is a safe and efficacious treatment used for extravasation of many different agents 2, 13. Topical application of silver sulfadiazine and Intrasyte gel to the affected area is recommended whenever skin blistering is observed 6. More invasive methods of treatment include saline irrigation followed by suction, local administration of various vitamins and enzymes, negative pressure therapies and a combination of liposuction and saline/hyaluronidase washout 8, 13, 14, 15. Prompt fasciotomy is required if compartment syndrome is suspected.
Studies from several hospitals have shown that seeking urgent PS consultation for suspected extravasation cases reduces complication rates and improves patient outcomes 1, 16. Ghanem et al. 1 reported that the introduction of hospital guidelines for early referral to specialist service significantly increases the number of patients treated early by ensuring that all suspected cases are referred promptly to specialist service in childhood extravasation injuries. This report indicated that hospital guidelines for CM extravasation result in a major reduction in the incidence of skin necrosis and an important reduction in surgical intervention needed to treat the immediate and delayed consequences of these injuries. In 2011, our hospital initiated an adverse event reporting system for consulting with the PS department immediately after a suspected case of CM extravasation from CT scanning. Figure 3 provides the guidelines of initial management of CM extravasation injuries during CT scanning at Ajou University Hospital. Briefly, if potential CM extravasation is believed to have occurred during CT scanning, the first assessment is made by a nurse who documents the event and alerts the ward or the emergency room doctor to contact the PS department. The nurse then sends the patient back to the ward or emergency room. If the patient is from the outpatient department, the nurse sends the patient to the PS outpatient department and documents the event. The PS doctor examines the patient. If extravasation is confirmed, the PS doctor chooses the treatment option. If the expected extravasation volume is less than 50 ml, the patient is treated conservatively using light compression, affected limb elevation, pain control and hyaluronidase injection. If the expected extravasation volume is larger than 50 ml or the patient feels severe pressure on the affected limb without a sign of compartment syndrome, multiple slit incisions are made, followed by squeezing. In case of suspected compartment syndrome, we consider immediate fasciotomy, although in our experience, there have been no cases of compartment syndrome.
Figure 3.
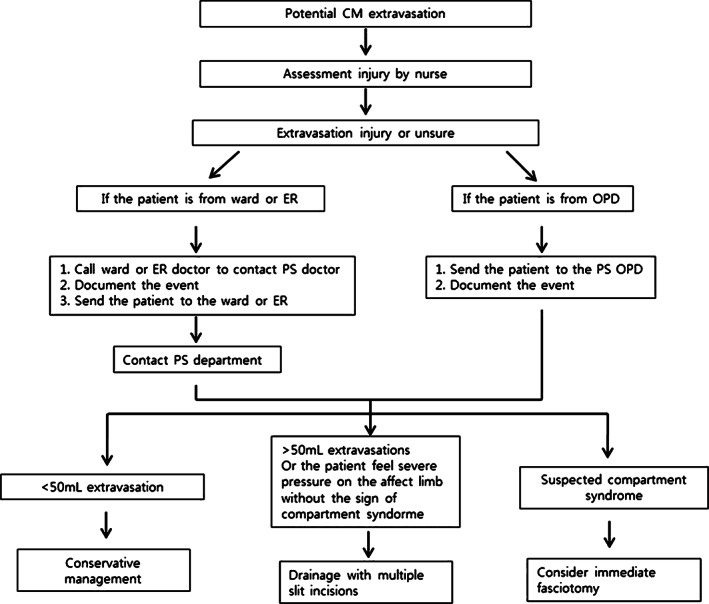
Algorithm summarising the guidelines of the initial management of contrast media extravasation injuries during computed tomography scanning.
With this protocol, we could assure the favourable results in terms of lowering complication rates and preventing severe adverse effects like compartment syndrome or extensive soft tissue loss requiring surgical intervention. If a minor wound develops, appropriate wound care is also started without delay. This strategy can increase patient satisfaction because of the lowered complication rate, and, if complications occur, their easier treatment. Although there is a general belief that non‐ionic CM extravasation injury can be managed with only conservative care, we have tried to minimise the likelihood of tissue injury with multiple slit incisions followed by squeezing rather than a wait‐and‐see response in case of large‐volume extravasations.
The strategy is based on the following premises. First, use of the power injector has increased, and there are large volumes of CM injected frequently. Automatic injection does appear not to influence the incidence of complication but does affect the severity of complications and the number of patients who must receive surgery as a consequence 16. Second, it is difficult to closely observe and follow‐up outpatients, and one cannot properly check the progression of symptoms of the nerve compression or vascular compromise. We believe it is better to remove the extravasated agents rapidly to reduce complication rates and minimise the patient discomfort. In our experience, multiple silts do not induce further wound problems or scar formation. Although this was not a randomised controlled study, we suggest this protocol and treatment method as clinical guidance of treatment of CM extravasation.
We propose a set of guidelines for the initial management of CM extravasation injuries from CT scanning for a timely intervention by the PS department. This reduces the complications and avoids the occurrence of severe adverse effects, such as compartment syndrome or extensive soft tissue loss. Appropriate wound care can also be started without delay if a minor wound develops. For large‐volume extravasation cases, immediate management with multiple slit incisions followed by squeezing is safe and effective in reducing the swelling quickly, preventing patient discomfort and decreasing skin and soft tissue problems associated with CM extravasation injuries.
References
- 1. Ghanem AM, Mansour A, Exton R, Powell J, Mashhadi S, Bulstrode N, Smith G. Childhood extravasation injuries: improved outcome following the introduction of hospital‐wide guidelines. J Plast Reconstr Aesthet Surg 2015;68:505–18. [DOI] [PubMed] [Google Scholar]
- 2. Hanrahan K. Hyaluronidase for treatment of intravenous extravasations: implementation of an evidence‐based guideline in a pediatric population. J Spec Pediatr Nurs 2013;18:253–62. [DOI] [PubMed] [Google Scholar]
- 3. Brown AS, Hoelzer DJ, Piercy SA. Skin necrosis from extravasation of intravenous fluids in children. Plast Reconstr Surg 1979;64:145–50. [DOI] [PubMed] [Google Scholar]
- 4. Camp‐Sorrell D. Developing extravasation protocols and monitoring outcomes. J Intraven Nurs 1998;21:232–9. [PubMed] [Google Scholar]
- 5. Napoli P, Corradino B, Badalamenti G, Tripoli M, Vieni S, Furfaro MF, Cordova A, Moschella F. Surgical treatment of extravasation injuries. J Surg Oncol 2005;91:264–8. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 6. Tonolini M, Campari A, Bianco R. Extravasation of radiographic contrast media: prevention, diagnosis, and treatment. Curr Probl Diagn Radiol 2012;41:52–5. [DOI] [PubMed] [Google Scholar]
- 7. Wang CL, Cohan RH, Ellis JH, Adusumilli S, Dunnick NR. Frequency, management, and outcome of extravasation of nonionic iodinated contrast medium in 69,657 intravenous injections. Radiology 2007;243:80–7. [DOI] [PubMed] [Google Scholar]
- 8. Goon PK, Dalal M. Limb‐threatening extravasation injury: topical negative pressure and limb salvage. Plast Reconstr Surg 2006;117:1064–5. [DOI] [PubMed] [Google Scholar]
- 9. Sbitany H, Koltz PF, Mays C, Girotto JA, Langstein HN. CT contrast extravasation in the upper extremity: strategies for management. Int J Surg 2010;8:384–6. [DOI] [PubMed] [Google Scholar]
- 10. Cohan RH, Leder RA, Bolick D, Herzberg AJ, Hedlund LW, Wheeler CT, Helms MJ, Dunnick NR. Extravascular extravasation of radiographic contrast media. Effects of conventional and low‐osmolar agents in the rat thigh. Invest Radiol 1990;25:504–10. [DOI] [PubMed] [Google Scholar]
- 11. Kim SH, Park JH, Kim YI, Kim CW, Han MC. Experimental tissue damage after subcutaneous injection of water soluble contrast media. Invest Radiol 1990;25:678–85. [DOI] [PubMed] [Google Scholar]
- 12. Cochran ST, Bomyea K, Kahn M. Treatment of iodinated contrast material extravasation with hyaluronidase. Acad Radiol 2002;9(2 Suppl):S544–6. [DOI] [PubMed] [Google Scholar]
- 13. Goutos I, Cogswell LK, Giele H. Extravasation injuries: a review. J Hand Surg Eur Vol 2014;39:808–18. [DOI] [PubMed] [Google Scholar]
- 14. Vandeweyer E, Heymans O, Deraemaecker R. Extravasation injuries and emergency suction as treatment. Plast Reconstr Surg 2000;105:109–10. [DOI] [PubMed] [Google Scholar]
- 15. Yilmaz M, Demirdover C, Mola F. Treatment options in extravasation injury: an experimental study in rats. Plast Reconstr Surg 2002;109:2418–23. [DOI] [PubMed] [Google Scholar]
- 16. Fallscheer P, Kammer E, Roeren T, Meuli‐Simmen C. Injury to the upper extremity caused by extravasation of contrast medium: a true emergency. Scand J Plast Reconstr Surg Hand Surg 2007;41:26–32. [DOI] [PubMed] [Google Scholar]


