Abstract
Pain and secretion of purulent materials are symptoms that are often associated with the pilonidal sinus. Generally, these symptoms are neglected by patients for a long time. Patients seek medical attention too late, fearing a prolonged period of pain and inability after surgery. The optimal therapy for pilonidal sinus should have the following characteristics: high healing rate, low recurrence rate, minimal postoperative pain and low cost. The aim of this study is to explore the effectiveness and safety of a new minimally invasive treatment: the scarless outpatient ablation of pilonidal sinus (SOAP). A total of 31 consecutive patients were enrolled; 27 of 31 patients were declared healed after the surgery (87·09%). After 1 year, only 4 of 27 patients (14·81%) reported symptoms related to recurrence of the disease. The average duration of the operation was 7·47 minutes. Patients reported the disappearance of painful symptoms after approximately 2·62 days and had been away from work for 0·53 days. No complications were recorded during the period of study. The advantages of the procedure examined in this study are its simplicity and rapidity of execution, its outpatient setting, its low cost and lack of complications. In our opinion, a randomised controlled trial should be conducted to validate the results related to this technique.
Keywords: Farrell applicator, Minimally invasive, Outpatient, Pilonidal disease, Scarless
Introduction
Pilonidal sinus is a disease affecting mainly men (male/female: 2/1), whose incidence in the general population is 26/100 000 1. An incidence of 8·8% has been reported in a population study considering young male recruits during medical examination for military service 2.
Several risk factors have been identified. A high incidence of pilonidal sinus is linked to a series of conditions: age between 18 and 30, male sex, hairiness, obesity, deep intergluteal cleft, lack of hygiene and sedentary occupation 3, 4.
The etiopathogenesis of pilonidal sinus is unclear. Initially it was thought to be a congenital disease related to remnants of the medullary canal. At the present time, it is considered as an acquired disease due to the penetration of hairs and epithelial debris into the subcutaneous tissue 5, 6.
The histological evidence of the lack of a wall in a pilonidal sinus may justify the use of minimally invasive therapeutic methods, which do not call for full excision of the sinus but solely for the removal of ectodermal debris within it.
Pain and secretion of purulent materials are symptoms that are often associated with pilonidal sinus. Generally, these symptoms are of moderate extent and are neglected by patients for a long time. Many patients tolerate symptoms up to 1 year before seeking treatment, fearing a prolonged period of pain and inability after the operation 1.
Methods
This study has been carried out by the Department of Minimally Invasive Surgery, University of Naples ‘Federico II’. Patients suffering from pilonidal sinus who presented at the outpatient department from January 2012 to December 2012 have been enrolled. Exclusion criteria are: previous surgical operations for pilonidal disease, age <18, inability to take care of personal hygiene autonomously, inability to maintain a prone posture for a few minutes, American Society of Anesthesiologists (ASA) score >2 and the presence of an acute abscess. Prior to their enrolment all patients were asked to give written informed consent. Study protocol was approved by the local ethics committee.
Surgical technique
The patient is placed in the prone position with buttocks slightly spread apart. After trichotomy and skin disinfection of the intergluteal cleft with 10% povidone–iodine (Betadine 10%, Meda Pharma S.p.A., Milan, Italy), the region is infiltrated with 5 ml of 2% mepivacaine (Carbosen 2%, Galenica Senese, Siena, Italy). A 20G round needle is used for a low pressure lavage of the cutaneous orifices with saline solution. In each cutaneous orifice, a 0·9 mm Farrell applicator (Integra Miltex, Plainsboro Township, NJ) is introduced (Figure 1). The Farrell applicator is a tool used in a variety of middle‐ear procedures such as the placement of cotton after a surgical procedure or to assist in the cleaning of pus. A rotating movement allows the Farrell applicator to proceed subcutaneously, by screwing inside the fistulous tract due to its thread. It is necessary to stop progression when the applicator comes out of another cutaneous orifice or when very vigorous pressure is required to go further. In this case, the probe is retracted without any rotating movement, allowing the hairs and debris wrapped around the thread to be dragged outside. This procedure generally causes a minimal bleeding which can be stopped by a new lavage of fistulous orifices with saline solution. If bleeding does not stop, another lavage of fistulous orifices with 3% hydrogen peroxide is carried out to achieve an optimal hemostasis. Finally, the scraping of the cutaneous orifices is performed to allow reepithelialisation and closure by secondary intention. After being under observation for a few minutes, the patient is allowed to ambulate and return home without requiring any antalgic therapy.
Figure 1.

Farrell applicator.
Study design
Once they are back home, patients are asked to note down daily the extent of pain on a special form based on the visual analogue scale (VAS 0‐10) as well as to take a 1 g paracetamol tablet if necessary (Figure 2). Patients are first seen in 15 days: if healing does not occur, the procedure is repeated and patients are seen again in 15 days. Unless recovery is achieved by the second attempt, the technique is considered to be a failure and patients undergo the excision of the pilonidal sinus with healing by secondary intention. All patients were declared healed after the first or the second attempt and were called for follow‐up 1 year after the procedure.
Figure 2.
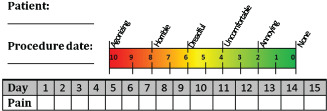
Visual analogue scale.
Outcome
The outcomes taken into account are: healing rate at 15 and 30 days (healing is associated with complete reepithelialisation, absence of pain and secretion), recurrence rate at 12 months, time to pain relief, surgery time, time away from work and complications.
Results
A total of 35 consecutive patients were considered for enrolment in this study (Table 1). Three patients were excluded because of an acute abscess. Only one patient refused to participate in the trial. A total of 31 patients were enrolled and subjected to the procedure; 21 patients were declared healed after 15 days and were seen after 12 months: follow‐up ended for all patients at 12 months. Delayed recovery was reported in ten patients. These patients who were declared non‐healed after 15 days underwent a new procedure: six of them were judged healed 15 days after the second procedure and were seen after 12 months: follow‐up is completed for all of them. Four patients were declared non‐healed after the second treatment and were recorded as a technique failure (Figure 3). Consequently, they underwent excision of the pilonidal sinus with healing by secondary intention.
Table 1.
Patients' characteristics
| Characteristic | Value |
|---|---|
| Patients enrolled | 31 |
| Male/female | 29/2 |
| Age (years) | 27 (18–45) |
| BMI | 24 (22–27) |
| Symptom duration (years) | 2 (0·1–10) |
| Single/multiple orifices | 5/26 |
| ASA score = 1 | 27 |
| ASA score = 2 | 4 |
BMI, body mass index.
Figure 3.
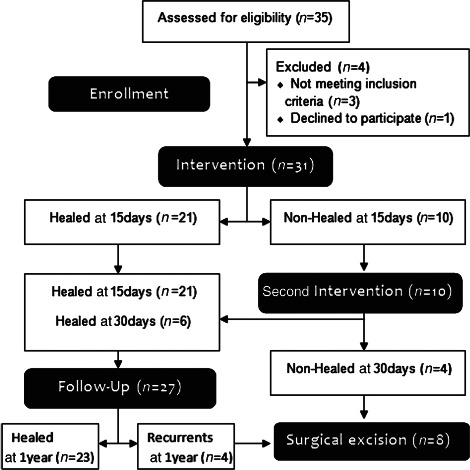
Flow diagram.
Healing rate
Healing is defined as the achievement of complete reepithelialisation of the wound without pain and secretion (Table 2). Healing was assessed 15 days after the procedure. Among the 31 patients who underwent the operation, 21 were declared healed after 15 days (67·74%, 21/31). Ten patients were judged non‐healed after 15 days and underwent the second procedure. They were seen after 30 days: 6 of them were declared healed (19·35%, 6/31). As a result, the number of successes is 27 (87·09%, 27/31).
Table 2.
Summary of results
| Outcome | Value |
|---|---|
| Healing rate at 15 days | 67·74% (21/31) |
| Healing rate at 30 days | 87·09% (27/31) |
| Recurrence rate at 12 months | 14·81% (4/27) |
| Time to pain relief | 2·62 days (range 1–7) |
| Operative time | 7·47 minutes (range 5–21) |
| Time off work | 0·53 days (range 0–3) |
| Complications | None |
Recurrence rate
A total of 27 patients were declared healed after the first or the second attempt and were called for follow‐up at 12 months. Four of them reported a recurrence of symptoms or disease recurrence was noticed during clinical examination (14·81%, 4/27): excision of the pilonidal sinus with healing by secondary intention was performed for these patients.
Time to pain relief
A total of 21 patients were declared healed after the first procedure and reported resolving of painful symptoms (VAS score <2) after 2·62 days (range 1–7).
Operative time
The average duration of the procedure was 7·47 minutes (range 5–21). All procedures were performed as outpatient surgery and patients returned home autonomously after being under observation for a few minutes.
Time off work
A total of 21 patients were declared healed after the first procedure and had to take 0·53 day off from work (range 0–3).
Complications
No complications have been reported after the procedure except for a minimal bleeding which was controlled through a lavage with a physiological solution.
Discussion
A total of 31 consecutive patients were enrolled in this study. On the whole, 27 of 31 patients have been declared healed (21 patients after 15 days, 6 patients after 30 days) and have been called for follow‐up at 12 months. During the period of 1 year, 4 of 27 patients reported symptoms related to a recurrence of the disease or showed signs of recurrence. No complications were recorded during the period of study. All procedures were performed on an outpatient basis and the patients were able to return home after being observed for a few minutes. The average duration of the operation was 7·47 minutes (range 5–21). Patients have reported the disappearance of painful symptoms (VAS <2) after approximately 2·62 days (range 1–7) and have been away from work for 0·53 days (range 0–3).
This study is based on the hypothesis that pilonidal disease is an inflammation due to hair and epithelial debris entrapped in the subcutaneous tissue. Based on the grounds of the conducted tests, structural alterations in the excised tissue have not been identified except for a foreign body tissue reaction 7. This hypothesis is supported by the onset, in the interdigital spaces of barbers, of a pathology similar to pilonidal disease, which is probably due to short hairs penetrating the skin because of cutaneous microlesions 8. According to our hypothesis, the removal of these foreign bodies may reduce the inflammation and encourage healing.
Numerous methods have been proposed for the treatment of pilonidal disease. Therefore, we analysed all systematic reviews and meta‐analyses dealing with pilonidal disease which have been published from 2000 to 2013. Most surgeons support the idea that the area affected by pilonidal disease is to be completely excised. Yet controversy exists over whether the wound should be sutured or left open. According to a recent systematic review of the existing literature, the excision of the diseased tissue with healing by secondary intention leads to a better outcome in terms of recurrence (recurrence rate = 4·8%) 1. However, this operation involves a long period of hospitalisation, acute postoperative pain and a long recovery time (2–6 months) 9. As far as the wound is concerned, on the one hand healing by primary intention results in faster recovery; on the other hand, there is a higher risk of recurrence (recurrence rate = 10·50%) 1. In order to avoid these problems, some techniques dealing with flap reconstruction have been introduced, although they require more sophisticated technical skills and they may have serious complications such as infection and flap necrosis.
Over the years, numerous techniques of conservative treatment have been employed. In 1994, the encouraging results achieved by Armstrong were published. His patients were treated by shaving off the intergluteal cleft until recovery from pilonidal disease occurred 10. In 2002, Lavelle suggested the use of laser hair removal 11. In 2009, a review of the literature regarding the use of phenol in the treatment of pilonidal disease, whose healing rate is 60–100%, was published 12. In 2013, a promising therapeutic endoscopic method [Video‐assisted ablation of pilonidal sinus (VAAPS)] has been described. Although it allows an early return to work (3 ± 3 days) and a faster recovery (15 days), it requires proper equipment and further validation. 13.
In our opinion, compared with other methods, the advantages of the procedure examined in this study are its simplicity and rapidity of execution (average duration: 7·47 minutes), its outpatient setting, its low cost and lack of complications. No postoperative morbidity has been described and faster healing allows an early return to work (time off from work 0·53 days). Moreover, no particular dedicated equipment is required to perform this procedure, except for the Farrell applicator which is available for $10. Finally, this technique does not preclude the chance to perform other treatments in case clinical symptomatology is not sufficiently controlled.
In another work published in 1965 a technique partly similar to the one taken into account in this study was used. In this work a nylon bristle brush was used to remove epithelial debris entrapped in the fistulous tract. Unfortunately, long‐term results of this experience have never been published 14.
Our research has been carried out taking into consideration a small number of patients. Numerous potential biases related to the lack of a control group and of procedures for randomisation exist. Therefore, the results achieved cannot be generalised. Nevertheless, the practicability and safety of the procedure is assured by the easy technique, the lack of complications and the encouraging outcomes. In our opinion, a randomised controlled trial should be conducted in order to validate the results related to this technique.
References
- 1. Al‐Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010;20:CD006213. doi: 10.1002/14651858.CD006213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Akinci OF, Bozer M, Uzunköy A, Düzgün SA, Coşkun A. Incidence and aetiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg 1999;165:339–42. [DOI] [PubMed] [Google Scholar]
- 3. Karydakis GE. New approach to the problem of pilonidal sinus. Lancet 1973;2:1414–5. [DOI] [PubMed] [Google Scholar]
- 4. Clothier PR, Haywood IR. The natural history of the post anal (pilonidal) sinus. Ann R Coll Surg Engl 1984;66:201–3. [PMC free article] [PubMed] [Google Scholar]
- 5. Allen‐Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg 1990;77:123–32. [DOI] [PubMed] [Google Scholar]
- 6. Bascom J. Pilonidal disease: long‐term results of follicle removal. Dis Colon Rectum 1983;26:800–7. [DOI] [PubMed] [Google Scholar]
- 7. Beck DE, Roberts PL, Saclarides TJ, Senagore AJ, Stamos MJ, Wexner SD. The ASCRS textbook of colon and rectal surgery, 2nd edn. New York: Springer, 2011. [Google Scholar]
- 8. Efthimiadis C, Kosmidis C, Anthimidis G, Grigoriou M, Levva S, Fachantidis P, Psihidis G. Barber's hair sinus in a female hairdresser: uncommon manifestation of an occupational disease: a case report. Cases J 2008;1:214. doi: 10.1186/1757-1626-1-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris CL, Holloway S. Development of an evidence‐based protocol for care of pilonidal sinus wounds healing by secondary intent using a modified reactive Delphi procedure. Part one: the literature review. Int Wound J 2012;9:156–72. doi: 10.1111/j.1742-481X.2011.00874.x[Epub 2011/10/17]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Armstrong JH, Barcia PJ. Pilonidal sinus disease. The conservative approach. Arch Surg. 1994;129:914–9. [DOI] [PubMed] [Google Scholar]
- 11. Lavelle M, Jafri Z, Town G. Recurrent pilonidal sinus treated with epilation using a ruby laser. J Cosmet Laser Ther 2002;4:45–7. [DOI] [PubMed] [Google Scholar]
- 12. Kayaalp C, Aydin C. Review of phenol treatment in sacrococcygeal pilonidal disease. Tech Coloproctol 2009;13:189–93. doi: 10.1007/s10151-009-0519-x[Epub 2009/08/05]. [DOI] [PubMed] [Google Scholar]
- 13. Milone M, Musella M, Di Spiezio Sardo A, Bifulco G, Salvatore G, Sosa Fernandez LM, Bianco P, Zizolfi B, Nappi C, Milone F. Video‐assisted ablation of pilonidal sinus: a new minimally invasive treatment—a pilot study. Surgery 2014;155:562–6. doi: 10.1016/j.surg.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 14. Lord PH, Millar DM. Pilonidal sinus: a simple treatment. Br J Surg. 1965;52:298–300. [DOI] [PubMed] [Google Scholar]


