Abstract
Skin tears appear to be a hidden and extensive problem despite an increased focus in the literature on skin tear epidemiology, prevention strategies and management modalities. Currently, there has been no report of skin tear epidemiology published in Singapore. The aim of the present study was to pilot the methodology by WoundWest at one of the tertairy hospitals in Singapore. The secondary objective was to determine the prevalence and current nursing management of skin tears within two selected acute medical wards in the hospital. A point prevalence survey was conducted within the two medical wards. Six registered nurses acted as the surveyors and underwent pre‐survey education. Inter‐rater reliability testing was conducted. Surveyors were paired and performed skin examinations on all available patients in the two wards. Data were collected on age, gender, skin tear anatomical locations, their Skin Tear Audit Research categories, dressings used on identified skin tears and related documentation. A total of 144 (98%) patients consented to skin inspections. Findings demonstrated a skin tear prevalence of 6·2%; all skin tears were found to be hospital‐acquired and located on the extremities. Most (78%) were in the age range of 70–89 years. There was a dearth in nursing documentation of the skin tears identified and their management. The findings suggested that nurses were lacking in the knowledge of skin tears, and documentation, if available, was not consistent. There is an urgent clinical need for the implementation of a validated skin tear classification tool; standardised protocols for skin tear prevention and management; and a comprehensive skin tear educational programme for hospital care staff. Quarterly hospital‐wide skin tear prevalence surveys are also needed to evaluate improvement strategies.
Keywords: Prevalence, Skin tears
Introduction and background of the study
Skin tears are common acute wounds that nurses encounter during their routine clinical practice. They are reported to commonly occur as a result of manual handling of patients 1, 2, 3. They tend to occur among the elderly because of normal physiological changes in the ageing skin 4, 5. It is estimated that the incidence of skin tears in USA stands at 1·5 million each year 2, 3, 6. In Western Australia (WA), state‐wide hospital prevalence surveys conducted across 86 public hospitals in 2007, 2008 and 2009 found skin tears to be the third largest group of wounds, and most were hospital‐acquired 7. Skin tears are a significant problem among the elderly 8, 9. Care of skin tear wounds in the elderly can be difficult, and it is known to be associated with prolonged hospitalisation stays, increased health care costs 10, 11 and adverse impacts on patients' quality of life 12.
Skin tears are generally considered to be preventable 13. Nurses are known to play a vital role in preserving skin integrity 4. Nurses' knowledge and skills with regards to skin tear prevention and management directly affect the quality of care and outcomes among hospitalised patients 14. The degree to which nursing interventions can prevent skin tears remained unknown in Singapore, and their management have been a matter of debate among nurses because skin tear prevention and management clinical guidelines did not exist in Singapore at the moment.
Singapore is a country located in Southeast Asia, an island between Malaysia and Indonesia 15. It is a multi‐cultural country with three main ethnic compositions: Chinese (74%), Malay (13%) and Indian (9·1%) 15. Similar to other developed countries, Singapore has an ageing population. There is now one in 12 Singaporeans aged 65 and above, with the ratio anticipated to increase to 5 in 12 Singaporeans by 2030 16
The lack of prevalence data in Singapore prompted the authors to undertake the current study. This pilot study aimed to determine the prevalence and nursing management of skin tears among patients in two medical wards in a teaching tertiary hospital in Singapore. It was also conducted to determine the feasibility and adequacy of the methodology prior to undertaking a larger hospital‐wide study in the future.
The prevalence data obtained was deemed to be useful in enabling the organisation to gain insight into the scope of the problem. More importantly, the findings will guide the development of prevention and management strategies to enhance clinical practice and subsequent patient outcomes within the surveyed wards and perhaps across the hospital.
Literature review
Skin tears are predominantly observed among the elderly. Payne and Martin 17 defined skin tears as:
‘A traumatic wound occurring principally on the extremities of older adults, as a result of friction alone or shearing and friction forces, which separate the epidermis from the dermis (partial thickness wound) or which separate both the epidermis and the dermis from underlying structures (full thickness wound)’.
The elderly are known to be significantly affected by the amount of pain, discomfort, anxiety and distress as a consequence of having a skin tear 13, 18. It can also affect an individual's well‐being in terms of psychological, mental, social and spiritual wellness 19.
Ageing of the integumentary system
Knowledge of the skin anatomy and pathophysiological changes related to ageing of the integumentary system is essential in enabling health care professionals to have a better understanding of the formation of a skin tear among elderly. Duthie et al. stated that the skin serves as the largest organ of the human body and acts as a barrier to protect internal organs from possible damage from exposure to excessive temperature changes, mechanical trauma, ultraviolet irradiation, toxic chemicals and invasion of micro‐organisms 20. The skin dermo‐epidermal junction, also known as the basal membrane zone (BMZ), which adheres the basal layer of the epidermis to the dermis slowly becomes flattened with ageing. The BMZ acts as a mechanical support for the dermis. It also regulates the transfer of protein, oxygen and nutrients across the dermo‐epidermal junction. This directly results in the effacement of dermal papillae and epidermal rete pegs 20. The poor attachment of the dermo‐epidermal layer results in less nutrient transfer between the epidermis and dermis compartments 5, while the loss of dermal capillaries results in diminished vascularisation to the skin 21. These changes may contribute to making the skin more susceptible to a tear even with minor shearing and friction.
Tiramas proposed that alteration of the dermis collagen predisposes the dermis to tear‐type injuries as the collagen and elastin fibres, which are found in the dermis and which give skin its tensile strength, becomes weakened or diminished with ageing 22. The skin is no longer able to withstand minor external shearing and traction forces. Benbow 8 and Duthie et al. 20 report that the loss of dermal thickness of up to 20% in the elderly may account for the paper‐thin, and almost transparent, type of skin that is so commonly observed among the elderly. These alterations in skin integrity account for friable skin that is at higher risk of developing a skin tear 5.
Elderly and skin tears
There are numerous factors that contribute to the breakdown of skin integrity. Besides age‐related skin changes, factors such as dehydration, compromised nutrition status, altered sensation and vision impairments that increase the risk of falls, decrease mobility and cognitive impairment are common risk factors identified in the literature 3, 5, 23, 24.
White et al. 24 proposed that individuals who are dependent and unable to perform activities of daily living (ADLs) were more likely to acquire skin tears as a result of the lifting and transferring activities. They emphasised that elderly, who might suffer from degeneration of brain function and declining functional status, are more prone to falling or bumping into equipment or objects and incur skin tears as a consequence. In addition, LeBlanc and Baranoski 3 and Lloyd‐Jones 25 suggested that skin tears frequently occurred in individuals who have a previous history of skin tears as a result of the reduced tensile strength of scar tissue.
Prevalence and characteristics of skin tears
Prevalence is defined as ‘the total numbers of existing cases or condition in a given population at a specific point of time’ by the Australia Wound Management Association, as cited in Mulligan et al. 26. It is written and calculated as a percentage (%), of the total instances of injury or disease in the population divided by the total number of individuals in the studied population.
According to Carville et al. 27 and White 28, skin tears are perceived to be as common as other wounds and occur more than pressure ulcers. White reported that 98·6% of nurses (RNs) (N = 118) in their study perceived that skin tears were common or extremely common 28. It was estimated that there were 1·5 million skin tears per year in institutionalised adults in USA 29. The Western Australia WoundWest state‐wide survey project that was first rolled out in May 2007 aimed to collect data on the number and types of wound from all public hospitals in the state. Following additional surveys, WoundsWest reported that skin tear prevalence was 8%, 11% and 9% in 2007, 2008 and 2009, respectively, and skin tears were predominantly found among the elderly 30. In another earlier study conducted in one of the hospitals in South Australia, 10·69% (n = 20) of patients surveyed were found to have skin tears 31. However, it was challenging to compare the prevalence rates across studies as the age range of the patients was not reported in the earlier study.
Skin tears can occur on any part of the body 11, 12. However, several authors 1, 11 reported that the majority of skin tears were found at the extremities of the body. Malone et al. conducted a 1‐year retrospective study in a single urban long‐term care institution and reported that 79·8% of the skin tears found were on the residents' upper extremities, especially the forearms and hands 11. A total of 14% were located over the residents' legs and feet; while those on the head accounted for 4% and the trunk 1·2%. Not surprisingly, Payne and Martin 17 reported that skin tear injuries were found at the posterior flank and sacral area. Skin tears on the sacral area could be mistaken as stage II pressure ulcers; however, the aetiology of both types of wounds was different 32.. Edwards, Gaskill and Nash 1 compared four types of dressings within two nursing homes, found that 60% of those who were eligible for recruitment to the study (n = 54) presented with skin tears that were located laterally or anteriorly over the right lower limb. The prospective descriptive survey conducted by McGough‐Csarny and Kopac of 154 nursing home residents found that 74% of the skin tears were located on the participants' upper extremities 5. The skin tears were relatively small, and wound dimensions ranged between 0·1 cm and 2·9 cm. Malone et al. reported that 289 out of 321 of skin tears in their study measured 1·89 ± 1·37 cm (mean ± SD), which makes the sizes of the wounds in both studies comparable 11.
Classification of skin tears
There is a need to classify skin tears when they occur. Several authors have stated that there is no common language used in identifying and classifying skin tears across all health care settings 6, 17, 27. A uniform skin tear definition and classification system may assist in standardising clinical teaching, practice, communication, care planning and research among health care professionals 3, 27, 28. The Payne–Martin Classification System was first presented in 1986 after a skin tear descriptive study was conducted to investigate the epidemiology and management of skin tears. Knowledge level among nurses has since improved. In the study by McTigue, registered nurses from two acute care community hospitals achieved strong baseline scores regarding identification and assessment of skin tears (97%), Payne categories of skin tears (83%) and skin tear treatment (74%) 33.
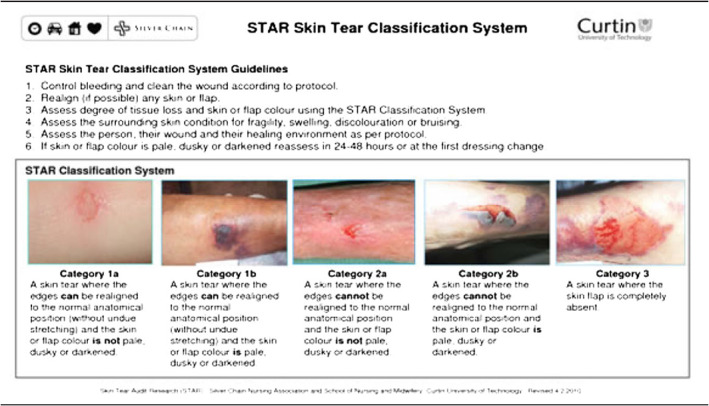
The Payne–Martin system is comprised of five categories and two sub‐categories, which classifies the amount of epidermal loss (%) 17. Carville et al. 27 highlighted that terms used in the Payne–Martin Classification System appeared ambiguous when they attempted to validate the classification among nurses with expertise in skin tear management. This finding led to the development of the Skin Tear Audit Research (STAR) Classification. The STAR classification system is also divided into five categories, with two subcategories (Table 1).
Table 1.
STAR skin tear classification system 34
Significance of current study
Although skin tear classification systems were reported in the literature, they are not well known and poorly utilised within the health care sector in Singapore. As a phenomenon, nurses tend to disregard skin tears as a type of wound unless it is massive in size and appears problematic to manage. Through clinical observation, some have been noted to misapply the pressure ulcer staging system in classifying and documenting the skin tears. This leads to misdiagnosis, inappropriate management, under‐reporting of skin tear incidence and inconsistencies in the assessment and documentation.
McErlean et al. stated that skin tear audits should be conducted to quantify the scope of the problem before initiating any skin tear prevention and management strategies within health care settings 31. The availability of the skin tear incidence or prevalence data will then enable the organisation to have some preliminary information on the trend and facilitate ongoing measurement, monitoring and evaluation via future survey or research undertaken on the topic of skin tears. The ongoing monitoring will serve as part of the ‘Quality Indicator’ and benchmark with other local or international institutions in the future. This current pilot study was therefore carried out to determine the baseline prevalence of skin tears and nursing management of skin tears among patients in two medical wards in a teaching tertiary hospital in Singapore. It was also conducted to determine the feasibility and adequacy of the methodology prior to undertaking a larger hospital‐wide study in the future.
Methods
Study design, sample and settings
A point prevalence survey methodology was adopted. The study site was a large teaching tertiary hospital in Singapore.
As the survey is a pilot study, it was conducted in two acute medical wards with a total of 146 beds. These wards were chosen because of the multifaceted disciplines and the availability of a high number of older patients. A convenience population‐based sample was adopted. All adult in‐patients at the time of survey were invited to participate in the survey. Ethics approval for the study was obtained from Curtin University (HREC: SON&M 5–2012) and the SingHealth Centralised Institutional Review Board (CIRB: 2012/215/A). As skin inspection is considered to be a normal component of routine nursing care, verbal consent was obtained prior to the inspections. Nursing records were reviewed within the ward level for skin tear documentation.
A hospital‐acquired wound was defined as ‘a wound that has no documentation present within 24 hours of admission, and it is presumed that the wound occurred between the time of admission and the actual survey day’ 26.
Surveyors' education and inter‐rater reliability
The survey team consisted of six registered nurses: two Nurse Clinicians, two Senior Staff Nurses and two Staff Nurses. A 90‐minute education session on the STAR skin tear classification and the use of the skin tear prevalence survey data collection tool was delivered by the Principal Investigator (PI), who is a wound nurse expert, two days prior to the actual survey day. An education package was developed specifically to educate the surveyors prior to the commencement of the survey. The package comprised of the following training components (Table 2).
Table 2.
Training components
|
Module 1‐Background information and understanding of skin tears Outlined the epidemiology of skin tears, background of ageing skin and elaborate the impact of skin tears on the patients, carers and health care system. |
|
Module 2‐STAR classification tool Outlined the definition of STAR categories and the use of STAR Classification Tool. |
|
Module 3‐Surveyors' inter‐rater‐reliability test Twenty skin tear images were used to test the surveyors' competency in classifying the skin tears using the STAR tool. |
|
Module 4‐Wound dressing products Outlined the common wound dressing products that are available in the hospital with the images attached. |
|
Module 5‐Survey process flow chart and the understanding of the survey method Introduced the survey flow chart and reinforced the importance of protocol process. |
|
Module 6‐Data collection tool Outlined the instructions of filling up data collection tool |
At the same time, an inter‐rater reliability test for the classification of skin tears using the STAR tool was conducted, and surveyors were asked to classify 20 skin tear photographs of various skin tear categories. The images were provided by the STAR researcher from the Silver Chain and Curtin University STAR skin tear image collection 34. Three surveyors were required to attempt a second inter‐rater test with six new skin tears images added to the first test. An inter‐rater reliability of 80% was achieved after two rounds.
Survey
Surveyors were paired to perform skin examination on all consenting patients. This is to ensure thorough inspection of the skin and enhance accuracy of results. The survey was conducted on 11 April 2012. Once a skin tear was identified on the patient, anatomical locations of the skin tear, the STAR category of skin tear and the presence of any existing dressing products on the skin tear were recorded.
Admission and updated documentation for the skin tear 48 hours prior to the survey was determined by checking the nursing records, nursing care plan and wound chart. The patient's documentation was examined to ascertain whether the skin tear was noted to be present on admission or deemed to be hospital‐acquired. The dressing in situ over the skin tear was recorded and compared with that documented in the patient's record (Figure 1).
Figure 1.
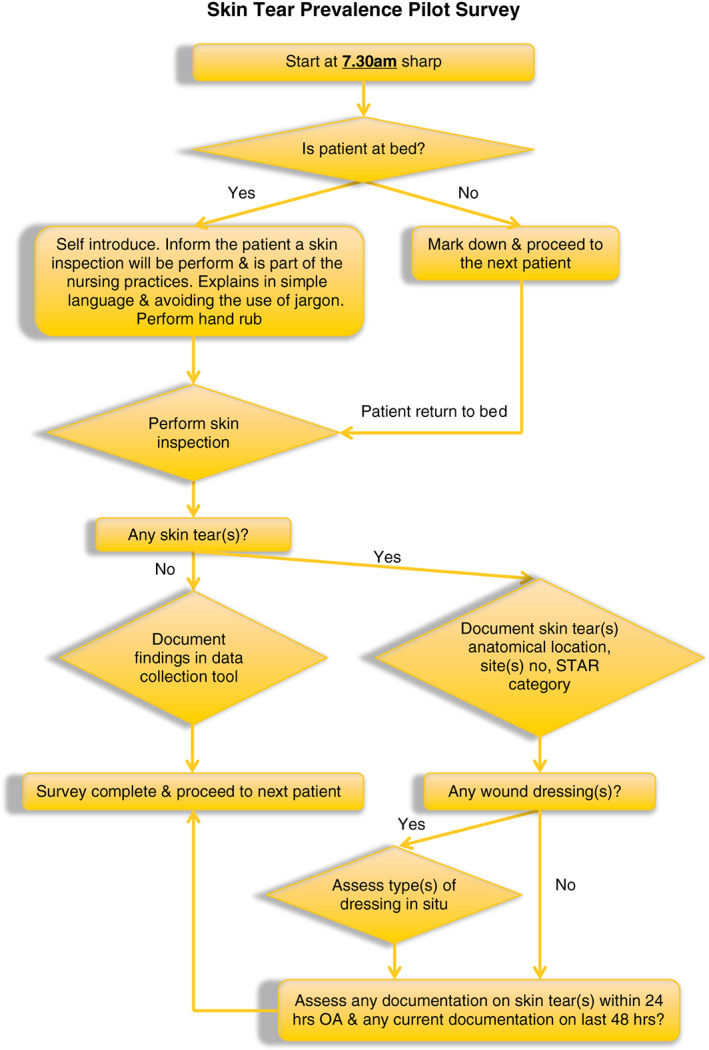
Skin tear prevalence survey flow chart.
Data collected were entered into statistical software SPSS Version 21·0 and analysed using descriptive statistics.
Results
A total of 146 patients were approached with a response rate of 98·6% (n = 144) in the two medical wards. Eighty‐six were females (60%). Overall skin tear prevalence was 6·2%. Nine patients had at least one or more skin tears present at the point of the survey. A total of 14 skin tears were identified. Four patients aged 80–89 years presented with one or more skin tears; three were in age group 70–79 years, and one each in age group 40–49 and 50–59 years. Patients aged 70 years and above accounted for 70% (n = 7) of the total number of patients found with one or more skin tears. The majority of skin tears were found to be under STAR Category 3 (43%) followed by STAR Category 1a (36%) and 7% each for STAR Category 1b, 2a and 2b (Table 3).
Table 3.
Demographics and characteristics of skin tears observed
| N (%) | ||
|---|---|---|
| Gender (n = 144) | Male | 58 (40) |
| Female | 56 (60) | |
| Skin tears observed | 9 (6·2) | |
| Age range of patients with one or more skin tears (n = 9) | 80–89 | 4 (44) |
| 70–79 | 3 (33) | |
| 50–59 | 1 (11) | |
| 40–49 | 1 (11) | |
| Anatomical sites (n = 14) | Upper extremities | 6 (43) |
| Lower extremities | 8 (57) | |
| Category of skin tears observed (n = 14) | 3 | 6 (43) |
| 1a | 5 (36) | |
| 1b | 1 (7) | |
| 2a | 1 (7) | |
| 2b | 1 (7) | |
As summarised in Table 3, all skin tears were located on the patients' extremities; six (43%) were identified at the upper extremities, over hand, forearm and upper arm. The remainder were located at the lower extremities, over the participant's thigh, shin, knee and heel areas.
Only one skin tear (7%) was found to have a semi‐permeable film applied. Thirteen skin tears (93%) did not have any wound dressing in situ. All skin tears were considered hospital‐acquired wounds as there was no documentation for any of the skin tears identified found in the nursing records within 24 hours of admission. Among the 14 skin tears identified, 10 (71%) tears were not documented within 48 hours prior to the survey. It is noted from the trend that skin tears of lesser severity were less likely to be reported and documented (Table 4).
Table 4.
Documentation and management of skin tears observed
| N (%) | ||
|---|---|---|
| Presence of dressing over skin tear (n = 14) | Yes | 1 (7) |
| No | 13 (93) | |
| Documentation within 48 hours (n = 14) | Yes | 4 (29) |
| No | 10 (71) | |
Discussion
This pilot study identified a prevalence rate of 6·2%. Although slightly lower than that reported in Western Australia (8–11%) 30 and South Australia (10·69%) 31, it is clinically significant as it demonstrated that skin tears do exist within the organisation and have been a ‘hidden’ problem that needs to be adequately addressed.
This study also demonstrated that patients aged 80–89 years had the greatest number of skin tears. These findings are similar to the findings of McGough‐Csarny and Kopac, which reported a higher prevalence of skin tears among those aged 85 years or older, classified as an ‘old‐old’ group 5. Skin tears were noted to increase with age in this study, and this was supported by Lloyd‐Jones 25 literature, which stated that the thinning of the epidermis made skin tear occurrence more evident in those aged 70 years and above. The survey findings revealed that the majority of the skin tears were found on the patients' extremities. This is in line with the findings of Edwards et al. 1, the 60% of the nursing home residents with skin tears reported involved the lower extremities. This survey found no skin tears to be located on those uncommon anatomical sites such as the head, trunk and sacral area as reported by Malone et al. 11 and McGough‐Csarny and Kopac 5.
The largest category of skin tears identified were STAR Category 3, which aligned with the hospital‐acquired skin tear findings reported in the WoundWest surveys from year 2007 to 2009 7. All skin tears identified were considered hospital‐acquired because there was no documentation in the patient's nursing records within 24 hours of admission. It was possible that the nurses failed to perform routine skin inspections and identify the existence of skin tears upon admission. A full body skin assessment should be conducted on admission to assess each patient's skin condition and identify existing skin tears using a standardised classification tool in conjunction with the pressure ulcer risk assessment practice.
The importance of the utilisation of common language in skin tear classification enables the best practice in any health care organisation 3, 17, 27, 35. LeBlanc and Baranoski 3 and Carville et al. 27 stressed that a validated skin tear classification tool is a prerequisite for any future prevalence, incidence and research study. Presently, there is no skin tear risk assessment tool and classification tool available in the institution. The lack of a skin tear classification tool and skin tear incidence‐reporting system could be assumed to lead to the under‐reporting of these injuries. This pilot study has demonstrated the feasibility of using the STAR Skin Tear Classification Tool in the assessment and documentation of skin tears.
White identified that nurses tended not to report skin tear injuries unless the wounds are ‘severe’, ‘large’, ‘problematic’ or associated with a head injury or fall 28. Data from our survey showed that little documentation was found when the skin tear injury was less severe according to the STAR categorisation. Although no actual measurements were recorded on the skin tears identified, the majority of the skin tears were relatively small in size and appeared to be 2 cm or less.
Unfortunately, only one skin tear was found to have a semi‐permeable film being applied. This might be because of nurses disregarding the significance of skin tears or that the wounds were relatively small and were perceived not to warrant much attention. It is essential that the organisation works within agreed clinical governance frameworks to ensure that evidence‐based guidelines or management algorithms be produced to support optimal clinical practice. Clinical guidelines are known to be able to aid nurses to provide quality care and evaluate the care against best‐recommended practice 36.
Limitations
This is a pilot study with a small sample size. A hospital‐wide survey would need to be conducted to establish the true prevalence of skin tears. Future studies are required to investigate further relationships between skin tear risk factors, patient's comorbidities, nutritional status and cognitive and functional status and the causes and locations of the skin tears.
Conclusion
The WoundWest survey methodology was adopted for this survey and used to conduct the first skin tear survey in Singapore. The results revealed the prevalence and current nursing management of skin tears within two medical acute wards in Singapore General Hospital, and they will assist in the implementation of skin tear prevention and management strategies in the two pilot wards.
The survey findings indicate that skin tears were a problem that was not being properly documented and addressed. Provision of a comprehensive skin tear educational programme for nurses and carers, adoption of a validated skin tear classification tool and conduction of regular hospital‐wide prevalence audit surveys would facilitate benchmarking and communication as well as the development of evidence‐based skin tear prevention and management strategies.
References
- 1. Edwards H, Gaskill D, Nash R. Treating skin tears in nursing home residents: a pilot study comparing four types of dressings. Int J Nurs Pract 1998;4:25–32. DOI: 10.1111/j.1440-172X.1998.00066.x. [DOI] [PubMed] [Google Scholar]
- 2. LeBlanc K, Baranoski S. Prevention and management of skin tears: clinical management extra. Adv Skin Wound Care 2009;22:325–32. [DOI] [PubMed] [Google Scholar]
- 3. LeBlanc K, Baranoski S. Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears©. Adv Skin Wound Care 2011;24:2–15. URL www.ovidsp.tx.ovid.com. [DOI] [PubMed] [Google Scholar]
- 4. Hampton S. How to preserve skin intergrity and prevent skin tears. Nursing & Residential Care 2010;12:284–7. URL www.internurse.com. [Google Scholar]
- 5. McGough‐Csarny J, Kopac CA. Skin tears in institutionalized elderly: an epidemiological study. Ostomy Wound Manage 1998;44(3A):14–25. URL http://ecu.vdxhoast.com/vdx/zengine. [PubMed] [Google Scholar]
- 6. McTigue T, D'Andrea S, Doyle‐Munoz J, Forrester DA. Efficacy of a skin tear education program: improving the knowledge of nurses practicing in acute care settings. J Wound, Ostomy Continence Nurs 2009;36:486–92. DOI: 10.1097/WON.0b013e3181b35ebd. [DOI] [PubMed] [Google Scholar]
- 7. Mulligan, S. , Scott, L. , Prentice, J. , Carville, K. , & Santamaria, N . (2009). WoundWest wound prevalence survey 2009: state‐wide report overview. [Internet]. Ambulatory Care Services, Department of Health 2009: Perth, Western Autralia. URL http://www.health.wa.gov.au/woundswest/docs/WWWPS_09_state_overview.pdf
- 8. Benbow M. Skin tears. Br J Community Nurs 2009;23:14. [Google Scholar]
- 9. Oddo D. Skin tears. In: Brown P, editor. Quick refence to wound care, 3rd edn. Sudbury: Jones and Bartlett Publishers, 2009:175–81. [Google Scholar]
- 10. Carville K. Wound care: shining light on skin tears [online]. Australian Ageing Agenda, 2008:64–5. URL http://search.informit.com.au/documentSummary;dn=842520781939399;res=IELFSC>. [Google Scholar]
- 11. Malone ML, Rozario N, Gavinski M, Goodwin J. Skin tears in the institutionalized elderly. J Am Geriatr Soc 1991;39:591–5. [DOI] [PubMed] [Google Scholar]
- 12. Baranoski S. Meeting the challenge of skin tears. Adv Skin Wound Care 2005;18:74–5. URL http://www.ovidsp.tx.ovid.com. [DOI] [PubMed] [Google Scholar]
- 13. Meuleneire F. Using a soft silicone‐coated net dressing to manage skin tears. J Wound Care 2002;11:365–69. [DOI] [PubMed] [Google Scholar]
- 14. Clarke T, Kelleher M, Fairbrother G. Starting a care improvement journey: focusing on the essentials of bedside nursing care in an Australian teaching hospital. J Clin Nurs 2010;19(13/14):1812–20. DOI: 10.1111/j.1365-2702.2009.03173.x. [DOI] [PubMed] [Google Scholar]
- 15.Department of Statistic Singapore. Population trends 2015. [Internet]. Singapore; 2015. (ISSN 1793–2424). URL http://www.singstat.gov.sg/docs/default‐source/default‐document‐library/publications/publications_and_papers/population_and_population_structure/population2015.pdf [accessed on 3 October 2015].
- 16.Ministry of Community Development, Youth and Sports [MCYS]. Committee on ageing issues Report on the Ageing Population. [Internet]. Singapore; 2006. (MCYS 22‐01A‐01). URL http://app.msf.gov.sg/Portals/0/Summary/research/CAI_report.pdf [accessed on 27 October 2015].
- 17. Payne RL, Martin MC. Defining and classifying skin tears: need for a common language: a critique and revision of the Payne‐Martin classification system for skin tears. Ostomy Wound Manag 1993;39:16–20. [PubMed] [Google Scholar]
- 18. Authority PPS. Skin tears: the clinical challenge. PA‐PSRS Patient Saf Advis 2006;3:1–8. [Google Scholar]
- 19.International consensus. Optimising wellbeing in people living with a Wound: An Expert Working Group Review. [Internet]. London: Wound International, 2012. URL http://www.woundsinternational.com/media/issues/554/files/content_10309.pdf [accessed on 20 October 2015].
- 20. Duthie EH, Katz PR, Malone ML. Practice of geriatrics, 4th edn. Philadelphia: Saunders Elsevier, 2007. [Google Scholar]
- 21. Vuolo J. Wound care made incredibly easy, 1st edn. London: Lippincott Williams & Wilkins, 2009. [Google Scholar]
- 22. Tiramas ML. The skin. In: Tiramas PS, editor. Physiological basis of aging and geriatrics, 4th edn. New York: Informa Healthcare, 2007:345–52. [Google Scholar]
- 23. Lloyd‐Jones M. Treatment of skin tears: revisiting wound assessment. Pract Nurs 2010;21:588–90. [Google Scholar]
- 24. White M, Karam S, Cowell B. Skin tears in frail elders: a practical approach to prevention. Geriatr Nurs 1994;15:95–9. [DOI] [PubMed] [Google Scholar]
- 25. Lloyd‐Jones M. The prevention and management of skin tears. Nurs Residential Care 2009;11:117–22. [Google Scholar]
- 26. Mulligan S, Scott L, Prentice J, Strachan V, Elmes R, Carville K, Santamaria N. Woundwest wound prevalence survey 2008 state‐wide report overview. Perth: Ambulatory Care Services, Department of Health 2008, 2008. [Google Scholar]
- 27. Carville K, Lewin G, Newall N, Haslehurst P, Michael R, Santamaria N, Roberts P. STAR: a consensus for skin tear classification. Prim Inten 2007;15:18. [Google Scholar]
- 28. White W. Skin tears: a descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Prim Inten 2001;9:138–49. [Google Scholar]
- 29. Baranoski S. Skin tears. Nurs Manage 2001;32:25–31; quiz 31–22. [PubMed] [Google Scholar]
- 30. Government of Western Australia Department of Health . (2009). WoundsWest wound survey 2009: Key results at a glance. URL http://www.health.wa.gov.au/woundswest/docs/Wound_survey_2009.pdf
- 31. McErlean B, Sandison S, Muir D, Hutchinson B, Humphreys W. Skin tear prevalence and management at one hospital. Prim Inten 2004;12:83–6. [Google Scholar]
- 32. Baranoski S, Ayello EA. Wound care essentials: practice principles, 3rd edn. Philadelphia: Lippincott Williams & Wilkins, 2012. [Google Scholar]
- 33. McTigue T, D'Andrea S, Doyle‐Munoz J, Forrester DA. Efficacy of a skin tear education program. J Wound Ostomy Continence Nurs 2009;36:486–92. [DOI] [PubMed] [Google Scholar]
- 34.Skin Tear Audit Research (STAR). Silver Chain Nursing Association and School of Nursing and Midwifery, Curtin University of Technology [revised 4 February 2010].
- 35. Labish C, O'Connel‐Gifford E. Improving skin tear outcomes using a topical nourishing skin care cream… Scientific and clinical abstracts from the 40th Annual Wound, Ostomy and Continence Nurses Annual Conference. J Wound, Ostomy Continence Nurs 2008;35(3S):S15–6. [Google Scholar]
- 36. Courtney M, McCutcheon H. Using evidence to guide nursing practice. New South Wales: Elsevier, 2010. [Google Scholar]


