Dear Editors,
Radiofrequency (RF) is chromophore independent and depends on the electrical properties of the target tissue and thus is expected to have good safety profiles for all skin types. For this reason, over the last decade, RF has been applied in many skin‐tightening technologies by delivering volumetric heating to dermal structures without disrupting the epidermis 1. In addition, RF has revolutionised the fields of scarring 2. Theoretically, RF's mechanisms of action include delivering uniform heat at a controlled depth to the dermal layers, resulting in immediate collagen shrinkage and subsequent collagen remodelling. Some authors have found that a dermal tissue temperature of 72°C generated an RF thermal zone pattern in the reticular dermis. This zone was observed for 4 weeks post‐treatment and was then replaced by new dermal tissue by 10 weeks post‐treatment, with concordant increases in HSP47 expression 1. Recently, a newly developed single microneedle radiofrequency (SMNR) modality that involves microneedle electrodes emitting and directly delivering RF waves at the dermal level, while sparing the epidermis, was developed. Given this technology, we tried to treat small pox scars by using this treatment strategy twice over 6 months.
A 65‐year‐old Korean man visited the authors' hospital because he suffered for several decades from depressed facial scars resulting from smallpox (Figure 1A). Anaesthesia was administered by applying a topical anaesthetic cream (EMLAs®; AstraZeneca, Wilmington, DE) for 30 minutes with occlusion. The treatment was given by SMNR (AGNES™; Gowoonsesang Cosmetics Co., Seoul, Korea) every 3 months over half a year, for a total of two treatments. The treatment parameters were as follows: needle depths ranged from 1·2 mm (C‐type needle) and exposure times ranged from 100 ms using a power level of 3. The patient was instructed to apply emollients several times a day for the first few days after each treatment and to avoid the use of any alternative therapeutic agent during the treatment course. The patient did not report any pain or discomfort during the treatment. No side effects were evident except for some slight oedema that resolved within 48 hours. Initial noticeable improvement was noted after 3 months of treatment (Figure 1B), with slight elevation, and the lesion showed marked improvement after 6 months (Figure 1C). When the treatment course was finished, the patient was satisfied with its outcome.
Figure 1.
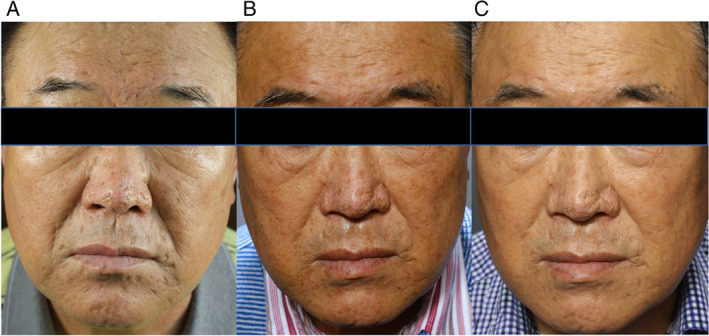
Patient's smallpox scar at baseline (A), 3 months (B) and 6 months after single microneedle radiofrequency treatments (C).
Recently, fractional resurfacing lasers have been widely used to treat scars because they prevent patient downtime, exudation, crusting and longstanding erythema compared to invasive skin‐resurfacing procedures, such as CO2 and Er:YAG laser. However, these modalities require more procedures to provide the same level of benefit accomplished by ablative resurfacing 3.
To this end, minimally invasive RF microneedle devices have recently been developed to overcome such problems by creating RF thermal zones with minimal epidermal injury. For example, a microneedling fractional radiofrequency device (MFRD) has been shown to be clinically efficient in managing atrophic depressed scars. Its insulated microneedles make it possible to prevent direct damage to the epidermis 2.
As MFRD delivers bipolar RF energy between the edges of its multi‐needles, RF energy from MFRD disperses in proportion to the number of its microneedle tips. Consequently, affected area and amount of electric fluence (J/cm2) from the multi‐needle bipolar RF system are limited. In contrast to MFRD, SMNR produces focused monopolar RF energy from its single‐needle tip and delivers a much higher electric fluence in same energy setting (J). Furthermore, this single‐needle tip has a shorter insulated part than MFRD (<0·5 mm versus 2·7 mm), which makes it possible to transfer RF energy to more superficial tissue, such as superficial dermis.
Although the insulated microneedle tip prevents epidermal damage, there is still a possibility of superficial burn in case the insulated part is worn out. This possibility can be reduced when practitioner use a zoom camera on the device that can magnify the needle tip in the field.
After using this SMNR, our patient showed comparable or better clinical results with high efficiency. Furthermore, other benefits of using this technique include shortened recovery times, improved outcomes in removing scars, low complication rates and high patient satisfaction.
The likely mechanism of SMNR reconstructing a depressed scar is inducing a thermal zone in the dermal layer, which in turn initiates the natural healing process. This presumably involves collagen remodelling, leading to the desired result. Other treatment modalities that have been used for scar correction also suggest this mechanism 3.
Another the potential benefit of SMNR is the ‘microneedling effect’. This effect was initially introduced for scar management as a dermabrasion or derma‐roller. This technique involves puncturing the skin with small needles to breakdown the damaged collagen and to induce new collagen deposition 4. During the procedure, tiny wounds are created in the papillary dermis resulting in the release of growth factors, which stimulate the formation of new collagen. Scarring the skin with these microneedles leads to micro‐trauma to the superficial dermis without eroding the epidermis. The epidermis, particularly the stratum corneum, remains intact except for the minute holes, which heal rapidly. Also, some authors reported that injuries less than 2–3 µm does not create a classical bleeding wound, as is the case with non‐traumatic microneedles 5. These reasons are likely explanations for the profound effect and minimal discomfort of the SMNR device after just two treatments.
Although we were not able to determine the precise mechanism of scar reconstruction by histological examination, the present study may support the clinical efficacy of SMNR in reducing scars produced by smallpox. This technique might be applied in various fields of dermatology with excellent clearance in an easy and safe manner. Also, future studies should be conducted to evaluate the optimum number and frequency of sessions and to compare with other scar treatment modalities.
Acknowledgements
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number : HI16C0666). The authors declare that they have no conflicts of interest.
References
- 1. Narurkar VA. Lasers, light sources, and radiofrequency devices for skin rejuvenation. Semin Cutan Med Surg 2006;25:145–50. [DOI] [PubMed] [Google Scholar]
- 2. Cho SI, Chung BY, Choi MG, Baek JH, Cho HJ, Park CW, Lee CH, Kim HO. Evaluation of the clinical efficacy of fractional radiofrequency microneedle treatment in acne scars and large facial pores. Dermatol Surg 2012;38:1017–24. [DOI] [PubMed] [Google Scholar]
- 3. Yoo KH, Ahn JY, Kim JY, Li K, Seo SJ, Hong CK. The use of 1540 nm fractional photothermolysis for the treatment of acne scars in Asian skin: a pilot study. Photodermatol Photoimmunol Photomed 2009;25:138–42. [DOI] [PubMed] [Google Scholar]
- 4. Kim SE, Lee JH, Kwon HB, Ahn BJ, Lee AY. Greater collagen deposition with the microneedle therapy system than with intense pulsed light. Dermatol Surg 2011;37:336–41. [DOI] [PubMed] [Google Scholar]
- 5. Dogra S, Yadav S, Sarangal R. Microneedling for acne scars in Asian skin type: an effective low cost treatment modality. J Cosmet Dermatol 2014;13:180–7. [DOI] [PubMed] [Google Scholar]


