Abstract
Globally, wound care costs the health care system 2–3% of the total expenditure on health, which equates to several billion dollars annually. To date, there are little data on the cost and healing rates of various wounds. This has been partly because of the difficulty in tracking wound management as the majority of wound care data has been focused on retrospective data from hospitals, general practice clinics and aged care facilities. This study reports on wound healing and cost of wounds collected from a larger project using the mobile wound care (MWC) electronic documentation system, which has been described elsewhere. The study involved 2350 clients from four health service districts in the Gippsland region in rural Australia who received treatments as part of the MWC research project (2010–2012), with a total of 3726 wounds identified (so an average of 1·6 wounds per client). By the end of the data collection period, 81% of these wounds had healed. A significant drop in healing time, cost of consumables and number of visits was found across the 3‐year period.
Keywords: Australia, Comorbidities, Mobile wound care, Wound costs, Wound healing
Background
Wound care costs the Australian Health system around $2·6 billion a year and affects almost 2% of the Australian population 1, 2. In the UK, the NHS costs of caring for patients with a chronic wound are conservatively estimated at £2·3–£3·1 billion per year (at 2005–2006 costs), which are around 3% of the total estimated out‐turn expenditure on health (£89·4 billion) for the same period 3, 4, 5. In the USA, a study reported a conservative estimate of more than $50 billion per year and that the prevalence of chronic non‐healing wounds is 2% of the general population 6, 7. These data indicate that wound healing is an ongoing major burden on the total health care system worldwide 8, 9, 10, 11.
To date, there are little data on the treatment costs and the healing rates of various wounds 11, 12, 13, 14. This has been partly because of the difficulty in tracking wound management as the majority of wound care data have been focused on retrospective data from hospitals, general practice clinics, community care services and residential aged care facilities. Most studies reporting on treatment costs and healing of wounds focus on either the effectiveness of a particular wound dressing or an intervention programme, often targeting a limited subset of the whole population and excluding palliative care patients or patients with anticipated amputations 15, 16, 17.
To obtain a more accurate idea of wound care costs and how treatment affects the overall expenditure, emphasis is currently placed on the speed at which healing occurs 17. By shortening the time taken to achieve complete healing, it is possible to terminate the need for ongoing interventions and reduce the expenditure 18, 19.
This study reports on wound prevalence, healing time, cost of care consumables and number of visits by district nurses providing treatment for wounds across four health service districts in the Gippsland Region, Victoria, Australia. The data were extracted from a larger project using the mobile wound care (MWC) electronic documentation system, which has been described elsewhere 20, 21.
Method
The current project was instigated by the Regional Clinical Nurse Consultant, Latrobe Community Health Service, in Gippsland and was funded by the Victorian Department of Health (DH) Strengthening Wound Management Practice initiative which was implemented across regional Victoria. The aim of the Wound management practice initiative was to target the management and treatment of chronic conditions and included the provision of extensive wound care training for district nursing staff in the region. The full methodology was published elsewhere 21. Briefly, de‐identified data were analysed using the MWC database between 12 April 2010 and 13 May 2012. Data were collected and recorded by district nurses from seven data collection sites across Gippsland in three main categories: patient, wound and treatment variables.
Comorbidities and factors affecting healing were collected separately. Nurses were able to enter the relevant comorbidities and factors affecting healing associated with the patients' medical history according to the list in the MWC database.
Statistical analysis
Data on the MWC healing time and costs were positively skewed – that is, numerous observations were many times larger than the average healing time and costs. These outliers were clinically significant but presented problems in terms of analysis. It was, therefore, inappropriate to analyse such skewed data using traditional methods (standard deviations and confidence intervals), which assume that the data were normally distributed. Bootstrapping is a technique that enables statistical analysis of our highly skewed data by producing a more appropriate (robust) measure of the confidence interval 22.
Bootstrapping for this data was calculated in two simple steps. Firstly, 1000 random samples were taken from within the data set and the average healing time for each of these samples was calculated. Secondly, using these 1000 samples, the 95% confidence interval was calculated with the upper and the lower limits of the confidence interval corresponding to the 2·5th and 97·5th percentile of the ordered 1000 sample results. Bootstrapped confidence intervals (BCa 95% CI) provide more stable (robust) results than alternative methods, and enable statistical comparisons between different subgroups (e.g. wound types, demographics, agencies) to be readily made. All the wound care data collected for analysis are shown in Figure 1.
Figure 1.
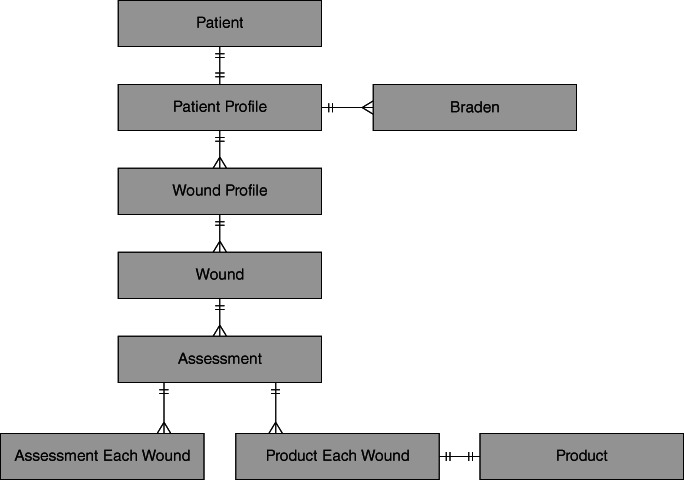
Data collected from the MWC database.
Results
There were 3726 wounds documented from 2350 clients, resulting in an average of 1·6 wounds per client. The majority of the wounds (56%) were acute wounds and were described as surgical, crush and trauma. Another 12·9% were associated with leg ulcers (venous, arterial, mixed and neuropathic), 9·4% were pressure ulcers (stage 1–4 according to guidelines at the time) and 7·5% were skin tears (categories 1–3). Other types of wounds caused by malignancy, fistula, skin disease, drain tube and irradiation totalled to 14%, as shown in Table 1.
Table 1.
Prevalence of wound aetiologies
| Aetiology | No. of wounds | % |
|---|---|---|
| Acute – surgical/crush/trauma | 2089 | 56·1 |
| All leg ulcers | 482 | 12·9 |
| Arterial leg ulcer | 43 | 1·2 |
| Mixed leg ulcer | 50 | 1·3 |
| Neuropathic/diabetic | 98 | 2·6 |
| Undefined leg ulcer | 176 | 4·7 |
| Venous leg ulcer | 115 | 3·1 |
| All pressure ulcers | 349 | 9·4 |
| Pressure ulcer – stage 1 | 81 | 2·2 |
| Pressure ulcer – stage 2 | 153 | 4·1 |
| Pressure ulcer – stage 3 | 84 | 2·3 |
| Pressure ulcer – stage 4 | 31 | .8 |
| All skin tears | 281 | 7·5 |
| Skin tear category 1a | 86 | 2·3 |
| Skin tear category 1b | 52 | 1·4 |
| Skin tear category 2a | 43 | 1·2 |
| Skin tear category 2b | 43 | 1·2 |
| Skin tear category 3 | 57 | 1·5 |
| Other | 190 | 5·1 |
| Chronic – other than leg ulcers or p/u | 131 | 3·5 |
| Malignancy | 75 | 2·0 |
| Fistula/abscess/pilonidal sinus | 73 | 2·0 |
| Skin disease | 27 | .7 |
| Drain tube | 16 | .4 |
| Irradiation | 13 | .3 |
| Total | 3726 | 100·0 |
Of the total 3726 wounds, 3009 healed during the course of the project, which shows a healing rate of 81%. This analysis showed a consistent drop in the healing time of all wounds across the 3 years of the project, dropping from 75·5 days in year 1 to 58·3 days in year 2, and finally to 43·3 days in year 3 as shown in Table 2. The average healing times per aetiology is shown in Table 3. The highest healing times were reported for arterial leg ulcers with an average of 143 days and the lowest healing times were obtained from category 1a skin tears of 29 days. This improvement was also seen within individual aetiologies such as acute/surgical/trauma, all leg ulcers, all pressure ulcers, stage 2 pressure ulcers, skin tears and some chronic wounds as shown in Table 3.
Table 2.
Healing time by aetiology
| Aetiology | n | Healing time | BCa 95% CI | ||
|---|---|---|---|---|---|
| Mean | Standard deviation | Lower | Upper | ||
| Arterial leg ulcer | 29 | 142·8 | 113·8 | 106·2 | 184·9 |
| Chronic – other than leg ulcers or p/u | 87 | 128·2 | 140·3 | 101·5 | 161·1 |
| Malignancy | 65 | 125·1 | 139·2 | 94·0 | 157·9 |
| Mixed leg ulcer | 37 | 107·9 | 94·8 | 81·9 | 138·4 |
| Venous leg ulcer | 94 | 106·5 | 104·4 | 87·3 | 125·7 |
| Neuropathic/diabetic | 77 | 100·8 | 86·7 | 83·7 | 120·8 |
| Pressure ulcer – stage 4* | 18 | 99·6 | 72·9 | 68·2 | 133·7 |
| Pressure ulcer – stage 3 | 63 | 96·0 | 96·3 | 74·7 | 119·5 |
| Pressure ulcer – stage 2 | 127 | 84·2 | 95·9 | 67·5 | 102·8 |
| Undefined leg ulcer | 133 | 78·4 | 81·7 | 65·9 | 92·4 |
| Skin disease | 20 | 74·4 | 86·9 | 46·5 | 106·5 |
| Other | 149 | 62·0 | 81·0 | 51·7 | 72·6 |
| Pressure ulcer – stage 1 | 72 | 62·0 | 66·7 | 48·5 | 77·2 |
| Fistula/abscess/pilonidal sinus | 61 | 55·1 | 73·5 | 39·4 | 73·7 |
| Acute – surgical/crush/trauma | 1732 | 47·9 | 59·8 | 45·3 | 51·1 |
| Skin tear category 2a | 38 | 44·3 | 69·4 | 27·2 | 65·0 |
| Skin tear category 2b | 30 | 42·5 | 38·1 | 30·4 | 56·4 |
| Skin tear category 3 | 45 | 41·7 | 39·0 | 32·2 | 53·8 |
| Irradiation* | 10 | 35·5 | 30·5 | 17·4 | 55·0 |
| Drain tube* | 14 | 34·1 | 39·9 | 18·4 | 60·0 |
| Skin tear category 1b | 41 | 31·2 | 29·9 | 23·1 | 40·7 |
| Skin tear category 1a | 67 | 29·2 | 26·2 | 23·3 | 35·5 |
| Total healed wounds | 3009 | 61·4 | 77·7 | 58·7 | 64·0 |
CI, confidence interval.
Indicates sample size is less than 20.
Table 3.
Progress over the study in healing time within aetiologies
| Acute/surgical/trauma | All leg ulcers | All pressure ulcers | Pressure ulcer stage 2 | All skin tears | Chronic other than leg ulcers or pilonidal sinus | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Heal time (days) | Significant (2 tailed) | n | Heal time (days) | Significant (2 tailed) | n | Heal time (days) | Significant (2 tailed) | n | Heal time (days) | Significant (2 tailed) | n | Heal time (days) | Significant (2 tailed) | n | Heal time (days) | Significant (2 tailed) | |
| All years | 1732 | 47·9 | 370 | 98·2 | 280 | 82·1 | 127 | 84·2 | 221 | 36·5 | 87 | 128·2 | ||||||
| Year 1 | 591 | 56·1 | .000 | 171 | 108·2 | .003 | 110 | 96·8 | .013 | 48 | 121·7 | .001 | 88 | 45·4 | .025 | 41 | 160·5 | .035 |
| Year 2 | 686 | 47·2 | 126 | 104·2 | 113 | 81·9 | 58 | 69·7 | 93 | 28·8 | 29 | 124·4 | ||||||
| Year 3 | 455 | 38·5 | 73 | 64·5 | 57 | 54·4 | 21 | 38·5 | 40 | 34·9 | 17 | 56·9 | ||||||
There were 57 cases where the cost of treatment consumables was not recorded, leaving out the data on 2952 of the 3009 wounds. These costs relate to any product, solution, instrument, tape or dressing used for wound healing. Costs ranged from $0 (i.e. no cost treatments, as it was provided by other systems) to $5318 (Table 4). Only 87 wounds (3%) were externally funded or self‐funded and the remaining wounds were funded by the organisations. Analysis of the cost of treatment consumables also showed an overall reduction, starting at $149 in year 1, rising slightly to $159 in year 2, before dropping sharply to $99 in the final year as shown in Table 5.
Table 4.
Cost of wounds progress through study period
| Progress through project | n | Cost of treatment | BCa 95% CI | df | Significant | ||
|---|---|---|---|---|---|---|---|
| Mean ($) | Standard deviation | Lower | Upper | ||||
| Year 1 | 1129 | 148·79 | 297·05 | 132·73 | 167·98 | 2 | .000 |
| Year 2 | 1136 | 158·70 | 270·24 | 143·43 | 174·30 | ||
| Year 3 | 687 | 98·91 | 157·87 | 87·52 | 111·15 | ||
| Total healed wounds | 2952 | 140·99 | 261·09 | 130·31 | 151·80 | ||
Table 5.
Cost of consumables by year of project
| Grouped aetiology | Acute – surgical/crush/trauma | All leg ulcers | All pressure ulcers | All skin ulcers | Chronic – other than leg ulcers or p/u | Drain tube | Fistula/abscess/pilonidal sinus | Irradiation | Malignancy | Other | Skin disease |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 1697 | 361 | 277 | 218 | 82 | 14 | 61 | 10 | 65 | 148 | 19 |
| Mean ($) | 130·67 | 185·88 | 162·68 | 45·96 | 260·96 | 27·29 | 241·86 | 87·24 | 186·71 | 141·82 | 92·32 |
| Non‐adherent dressings | 159·55 | 270·00 | 204·27 | 66·88 | 524·63 | 106·44 | 118·49 | 327·70 | 186·76 | 102·61 | |
| Odour absorbent | 842·41 | 556·01 | 964·50 | 305·20 | |||||||
| Miscellaneous | 410·38 | 466·79 | 320·85 | 74·66 | 533·17 | 824·95 | 251·92 | 509·80 | 53·61 | ||
| Bandages | 166·43 | 255·30 | 213·56 | 48·93 | 438·25 | 182·08 | 347·56 | 243·84 | 122·39 | ||
| Cleanser | 147·89 | 209·53 | 206·70 | 51·22 | 312·24 | 39·12 | 266·23 | 96·77 | 218·77 | 176·44 | 84·93 |
| Creams | 338·57 | 441·62 | 321·53 | 475·12 | 485·28 | 904·37 | 464·68 | 415·20 | 248·95 | ||
| No cost dressings | 170·82 | 223·96 | 199·22 | 73·71 | 333·58 | 18·83 | 278·03 | 97·74 | 223·95 | 206·68 | 101·65 |
| Instruments | 139·04 | 195·23 | 183·30 | 50·65 | 282·13 | 38·00 | 258·06 | 87·24 | 201·29 | 168·08 | 99·50 |
| Tapes | 199·88 | 228·31 | 208·00 | 78·20 | 412·66 | 360·68 | 95·81 | 350·13 | 236·62 | 133·14 | |
| TNPT | 1763·59 | 238·70 | 177·36 | ||||||||
| Alginate/hydrofibres | 232·44 | 410·07 | 485·02 | 72·63 | 740·81 | 386·47 | 146·67 | 417·80 | 350·43 | ||
| Antimicrobial | 263·62 | 296·96 | 324·98 | 104·39 | 518·98 | 86·63 | 505·72 | 238·99 | 407·54 | 276·98 | 151·30 |
| Dry dressings | 161·88 | 252·08 | 241·99 | 68·23 | 345·64 | 50·33 | 280·90 | 95·87 | 258·16 | 220·79 | 112·26 |
| Films | 178·22 | 243·48 | 215·85 | 55·06 | 460·83 | 41·05 | 159·59 | 202·88 | 229·13 | ||
| Foams | 173·00 | 219·97 | 178·58 | 53·04 | 274·70 | 37·82 | 148·40 | 143·60 | 260·84 | 208·84 | 84·94 |
| Hydrocolloids honey | 342·02 | 280·25 | 313·87 | 34·01 | 1092·33 | 129·92 | 238·99 | 530·59 | 900·77 | 83·85 | |
| Hydrogels | 259·07 | 341·22 | 269·19 | 118·87 | 359·98 | 673·92 | 104·65 | 398·01 | 267·35 | 23·20 | |
| Hypertonic gauze | 332·18 | 242·61 | 351·07 | 44·72 | 604·99 | 514·51 | 238·99 | 415·33 | 147·80 | ||
| Island dressings | 159·81 | 256·00 | 178·48 | 55·32 | 497·29 | 50·23 | 353·43 | 45·51 | 227·19 | 237·81 | 81·25 |
| Wipes | 298·40 | 293·98 | 273·10 | 27·66 | 587·52 | 481·74 | 238·99 | 422·41 | 290·09 | 153·46 |
TNPT, topical negative pressure therapy.
Analysis of the number of visits showed a similar pattern, starting at an average of 13 visits, rising slightly to 13·6 visits in year 2, and then dropping to 10·7 visits in year 3 as shown in Table 6.
Table 6.
Number of visits by aetiology
| Aetiology | No. of visits | BCa 95% CI | |||
|---|---|---|---|---|---|
| n | Mean | Standard deviation | Lower | Upper | |
| Pressure ulcer – stage 4 | 18 | 27·5 | 34·6 | 14·6 | 27·1 |
| Arterial leg ulcer | 29 | 21·7 | 22·7 | 13·5 | 29·4 |
| Malignancy | 65 | 20·5 | 27·3 | 13·3 | 42·0 |
| Fistula/abscess/pilonidal sinus | 61 | 20·5 | 35·9 | 4·1 | 6·9 |
| Pressure Ulcer – stage 3 | 63 | 18·9 | 20·4 | 4·0 | 5·4 |
| Venous leg ulcer | 94 | 18·2 | 24·5 | 10·7 | 16·4 |
| Chronic – other than leg ulcers or p/u | 87 | 18·1 | 25·5 | 14·1 | 23·1 |
| Irradiation | 10 | 15·0 | 9·5 | 7·5 | 13·5 |
| Neuropathic/diabetic | 77 | 13·7 | 12·0 | 6·0 | 10·6 |
| Undefined leg ulcer | 133 | 13·3 | 18·1 | 9·3 | 18·1 |
| Mixed leg ulcer | 37 | 13·2 | 13·3 | 13·6 | 23·5 |
| Other | 149 | 13·0 | 16·7 | 15·5 | 29·1 |
| Pressure ulcer – stage 2 | 127 | 12·8 | 14·3 | 11·1 | 16·7 |
| Acute – surgical/crush/trauma | 1732 | 12·0 | 13·2 | 11·4 | 12·7 |
| Skin disease | 20 | 10·3 | 6·6 | 9·1 | 20·9 |
| Skin tear category 2b | 30 | 8·8 | 7·8 | 4·0 | 7·7 |
| Pressure ulcer – stage 1 | 72 | 8·1 | 9·4 | 10·7 | 15·4 |
| Skin tear category 3 | 45 | 6·9 | 6·5 | 4·7 | 9·0 |
| Skin tear category 2a | 38 | 6·6 | 7·4 | 5·2 | 9·0 |
| Drain tube* | 14 | 5·6 | 3·0 | 10·7 | 15·6 |
| Skin tear category 1b | 41 | 5·4 | 5·1 | 6·3 | 11·4 |
| Skin tear category 1a | 67 | 4·7 | 3·0 | 14·4 | 23·8 |
| Total healed wounds | 3009 | 12·7 | 16·1 | 12·2 | 13·3 |
Indicates sample size is less than 20.
Discussion
The information collected through the MWC system and outlined here in terms of wound prevalence, healing times and wounds costs for different treatment types provides the evidence base for future practice in the region and beyond.
This study reported on wound healing times and costs of different wound aetiologies collected using an electronic wound system. To our knowledge, this is the first Australian study to report on these outcomes. Prior to MWC, no data existed regionally, statewide or nationally as to the type or even numbers of wounds that were treated as part of the Home and Community Care services. The data from the first year of the MWC research project indicated that just over 80% of all wounds came from just four main aetiologies: skin tears, leg ulcers, pressure ulcers and acute wounds. This allowed the regional training to be specifically tailored to provide education around the management of these specific wound types. This has resulted in an overall decrease in healing times and costs associated with wounds over the 3‐year study period.
The slight increases in costs and number of visits in the second year are likely to be because of MWC‐based improvements in record keeping over time, leading to year 2 being a more accurate measure of costs and visits than the first year. In addition, the increased focus on wound care may have led to initial increases in costs and visits, which levelled off and then started to decline significantly by the final year of the project. A special attention was given to the ongoing training of the wound nurses beyond the life of the project to ensure appropriate wound assessment and management as per the organisations' guidelines. This will potentially ensure the sustainability of the benefits of the MWC project.
The MWC project resulted in considerable upskilling in terms of computer literacy, which varied widely across organisations at the commencement of the project. This was partly because of some organisations making data entry the responsibility of ward clerks or administrative personnel, often because of the limited access to information technology (IT) facilities referred to as a barrier above. In three sites, the MWC research commenced simultaneously or subsequently to the introduction of other data entry programmes used for funding and staff allocation. Ongoing IT support and follow up resulted in keeping all nurses involved in the project. Having nurses enter their own data reduces the likelihood of data error caused as a result of duplicate handling and transcription problems.
Another significant advantage of the early outcomes of access to these data was greater targeting of the wound management training being provided to the region as part of the wider Strengthening Wound Management Practice Regional Victoria initiative.
The limitation of this study includes the lack of involvement of general practice clients in the Gippsland areas as many clients consult their general practitioners for their wounds rather than going to hospitals or community health services. Another limitation was the additional time requirement of data entry demanded of nurses involved in research, the demand of learning to use a new IT tool and the reliance on the nurses to enter the data. Nonetheless, the large number of wounds collected in the database may have overcome this latter limitation.
Conclusion
The findings after 3 years of the MWC research project are clear, with significant decreases in healing time, costs of treatment and number of visits. In addition to the recorded outcomes, there were also major benefits to the participating organisations in terms of skill development and greater collaboration across the region.
Acknowledgements
The Research Team would like to acknowledge and thank the following organisations and individuals who have contributed to the project: Contributing health services: Latrobe Community Health Service Ltd; West Gippsland Healthcare Group; Central Gippsland Health Service; Bairnsdale Regional Health Service; the nursing Unit Managers of the District Nursing Services; the District Nursing Staff who entered the data daily for 3 years; Mölnlycke Health Care who supplied the key treatment consumables for the Skin Tear Pathway; HSAGlobal who provided the software along with training and support; Fujitsu who provided the computing platform on which the software operated in Year 1 and LCHS who provided the platform for years 2 and 3; Dr Matthew McGrail for his statistical support and the wound care clients. This project was funded by a grant from Latrobe Community Health Service and Department of Health, Victoria, Australia.
References
- 1. Australian Institute of Health and Welfare . Key indicators of progress for chronic disease and associated determinants: data report. Canberra: AIHW, 2011. [Google Scholar]
- 2. Santamaria N. Woundswest: identifying the prevalence of wounds within western Australia's public health system. EWMA J 2009;9:13–8. [Google Scholar]
- 3. Kerstein M. Unexpected economics of ulcer care protocols. South Med J 2004;97:135–6. [DOI] [PubMed] [Google Scholar]
- 4. Posnett J, Franks PJ. The costs of skin breakdown and ulceration in the UK. In: Pownall M, editor. Skin breakdown–the silent epidemic. Hull: The Smith and Nephew Foundation, 2007. [Google Scholar]
- 5. Vowden K, Vowden P, Posnett J. The resource costs of wound care in Bradford and Airedale primary care trust in the UK [multicenter study]. J Wound Care 2009;18:93–4 96–8, 100 passim. [DOI] [PubMed] [Google Scholar]
- 6. Hurd T, Posnett J. Point prevalence of wounds in a sample of acute hospitals in Canada. Int Wound J 2009;6:287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodrigues I, Megies MF. Prevalence of chronic wounds in Quebec home care: an exploratory study. Ostomy Wound Manage 2006;52:46–57. [PubMed] [Google Scholar]
- 8. Srinivasaiah N, Dugdall H, Barrett S, Drew PJ. A point prevalence survey of wounds in north‐east England. J Wound Care 2007;16:413–6 418–9. [DOI] [PubMed] [Google Scholar]
- 9. Mahe E, Langlois G, Baron G, Girard L, Macrez A, Fargeot C, Crickx B. Results of a comprehensive hospital‐based wound survey. J Wound Care 2006;15:381–4. [DOI] [PubMed] [Google Scholar]
- 10. Strachan V, Prentice J, Newall N, Elmes R, Carville K, Santamaria N, Della P. WoundsWest Wound Prevalence Survey 2007. State‐wide Report Overview. Perth: Ambulatory Care Services, Department of Health. URL www.health.wa.gov.au/woundswest [accessed on 12 October 2014]
- 11. Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup F, Gurtner GC, Longaker MT. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 2009;17:763–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kuhn BA, Coulter SJ. Balancing ulcer cost and quality equation. Nurs Econ 1992;10:353–9. [PubMed] [Google Scholar]
- 13. Hess CT. Putting the squeeze on venous ulcers. Nursing 2004;34(Suppl Travel):8–13. [DOI] [PubMed] [Google Scholar]
- 14. Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. J Am Podiatr Med Assoc 2010;100:335–41. [DOI] [PubMed] [Google Scholar]
- 15. O'Brien JA, Cowman S. An exploration of nursing documentation of pressure ulcer care in an acute setting in Ireland. J Wound Care 2011;20:197–205. [DOI] [PubMed] [Google Scholar]
- 16. Rayner R. A review of the effectiveness of a nurse‐led rural community wound clinic. Prim Interv 2007;15:130–7. [Google Scholar]
- 17. Pieper B, Templin T, Dobal M, Jacox A. Home care nurses' ratings of appropriateness of wound treatments and wound healing. J Wound Ostomy Continence Nurs 2002;29:20–8. [DOI] [PubMed] [Google Scholar]
- 18. Thomas C. The art of skin and wound care documentation. Home Healthc Nurse 2005;23:502–13. [DOI] [PubMed] [Google Scholar]
- 19. Tapp RA. Inhibitors and facilitators to documentation of nursing practice. West J Nurs Res 1990;12:229–40. [DOI] [PubMed] [Google Scholar]
- 20. Khalil H et al. Implementation of a successful electronic wound documentation system in rural Victoria, Australia: a subject of collaboration and community engagement. Int Wound J 2014;11:314–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walker J et al. Identifying wound prevalence using the Mobile Wound Care program. Int Wound J 2014;11:319–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yung YF, Bentler PM. Bootstrapping techniques in analysis of mean and covariance structures. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: issues and techniques. Hillsdale: Lawrence Erlbaum, 1996:195–226. [Google Scholar]


