Abstract
Pilonidal sinus surgery could, as of now, be considered a surgery tailored more to the surgeon than to the patient. In an attempt to give to surgeons an objective instrument of decision, we have evaluated which variables could be considered predictive of postoperative complications after pilonidal sinus surgery. A prospective electronic database of all patients treated for sacrococcygeal pilonidal disease was analysed. Sex, age, obesity, smoking, recurrent disease, the presence of multiple orifices and the distance between the most lateral orifice and midline were recorded and correlated with the occurrence of postoperative complications (infection and recurrence); 1006 patients were evaluated. Excision with primary mid‐line closure was performed on all the patients. Mean follow‐up was 7·3 ± 3·6 years. A total of 158 patients with postoperative complications (infection and/or recurrence) were recorded during this period. A multivariate analysis showed that, after adjusting for major clinical and demographic characteristics, only a recurrent disease [odds ratio (OR): 3·41, 95% confidence interval (CI): 1·89–6·15, P < 0·001] and the distance of lateral orifice from midline (OR: 26·3, 95% CI: 12·2–56·7, P < 0·001) were independent predictors of overall postoperative complications. Focussing on the distance from midline, the receiver operative characteristic (ROC) analysis showed that the distance of lateral orifice from midline predicted 79·2% of complications and the Youden's test identified the best cut‐off as 2·0 cm for this variable. An evidence‐based tool for deciding on the type of surgical intervention could be developed and validated by further ad hoc prospective studies evaluating our results in comparison to other different types of surgical techniques. Our results support the use of these variables as an effective way to tailor pilonidal sinus surgery to the patient, so as to obtain the best results in patient care.
Keywords: Infection, Pilonidal, Recurrence, Sacrococcygeal, Sinus
Introduction
In 1990, Allen‐Mersh conducted an extensive review of over 90 papers dealing with the treatment of pilonidal sinus 1. He concluded that ‘the choice of a particular surgical approach is dependent only on the surgeon's familiarity with the procedure’. This remark holds true even 20 years later.
Although many surgical methods have been proposed, no clear consensus as to the optimal treatment has been reported so far in the literature. Although known to provide faster healing and faster return to work, the primary closure technique appears to be associated with important problems such as a high recurrence rate and a high infection rate 2.
Pilonidal sinus surgery could, as of now, be considered a surgery tailored more to the surgeon than to the patient.
The choice of surgical technique is left to the discretion of the surgeon, with the surgeon's clinical judgement and experience being major factors in the decision‐making process.
In an attempt to give to surgeons an objective instrument of decision, we have evaluated which variables could be considered predictive of postoperative complications after pilonidal sinus surgery.
Methods
A prospective electronic database of all patients treated for sacrococcygeal pilonidal disease between September 1998 and December 2011 at ‘Federico II’ University in Naples was analysed. Local ethics committee approval and written informed consent signatures were obtained.
Patients with primary and recurrent diseases were included in the study, excluding those who presented with recurrent disease after a previous off‐midline surgery and those who refused to participate in the study; all patients lost during the follow‐up were also excluded. If signs of inflammation in the surrounding tissues were detected, antibiotic treatment was given, and the excision was undertaken 2 or 3 weeks later when the inflammatory process had been controlled.
All the surgeries were performed using the same surgical technique. The surgeries were performed under local anaesthesia with administration of 30–60 ml of mepivacaine (Carbosen, 20 mg/ml; Galenica Senese, Siena, Italy). The patient was placed in the prone position, with the hips slightly flexed. The buttocks were retracted with adhesive tape. The sacral area was shaved and disinfected with povidone–iodine. The sinuses were injected with a few millilitres of methylene blue in order to stain all the sinuses and their branches. A significant reduction in the recurrence rate can be achieved with a single careful injection of the dye into the sinus at the start of the operation 3. A limited excision was performed, including all the marked tissues. An elliptical excision was marked around the sinuses with its long axis midline‐oriented. The skin incision was deepened down to the presacral fascia with diathermy, but the fascia was not included in the excision. Haemostasis was carefully achieved with electro‐cauterization. A series of strong resorbable deep sutures (Polyglactin 910) were passed at intervals of 1 in and at about half‐way between the skin and the presacral fascia. Each deep suture was passed through the midline of the presacral fascia. Non‐absorbable interrupted sutures were used for skin closure.
The patients were examined during follow‐up with a standard physical examination after 1 week, after 1 month, and every 3 months thereafter for at least 1 year; the patients lost during the follow‐up were excluded from the study.
Sex, age, obesity, smoking, recurrent disease, the presence of multiple orifices and the distance between the most lateral orifice and midline were recorded and correlated with the occurrence of postoperative complications (infection and recurrence).
Statistical analysis
Statistical analysis was performed with the SPSS 16 system (SPSS Inc., Chicago, IL). Continuous data were expressed as means ± standard deviation (SD); categorical variables were expressed as %. The t‐test was performed to compare continuous variables. The chi‐square test was employed to analyse categorical data. When the minimum expected value was less than five, the Fisher's exact test was used.
Receiver operative characteristic (ROC) curve analysis (with Youden's test) was used to define the best cut‐off value for distance between lateral orifice and midline in the prediction of postoperative complications.
To adjust for major clinical and demographic variables and to evaluate the risk for postoperative complications, a logistic regression analysis (stepwise method) was adopted. Multi‐collinearity effect in multi‐variable regression models was excluded by a stepwise approach, with each variable included for P < 0·05 and excluded for P > 0·1. All the results are presented as two‐tailed values with statistical significance if P values are less than 0·05.
Results
A total of 1230 patients with a diagnosis of pilonidal sinus underwent surgical excision over a 12‐year period. Seventy‐two patients were excluded because of the presence of at least one exclusion criteria: Forty‐one did not provide their consent to be included in a prospective study and 31 had recurrent disease after an off‐midline closure. Of the remaining 1068 patients included in our analysis, 62 patients were lost during follow‐up. Thus, 1006 patients were attended to and evaluated.
All procedures were performed under local anaesthesia with acceptable results, and without requiring regional or general anaesthesia. Furthermore, all procedures were successful and a complete excision and midline closure was obtained. Only minimal intra‐operative bleeding occurred and all episodes were resolved by electro‐cauterization. No further intra‐operative complications occurred. No patient required any further therapy other than a dry dressing.
Mean follow‐up was 7·3 ± 3·6 and a total of 158 patients with postoperative complications (infection and/or recurrence) were recorded during this period.
In the univariate analysis (Table 1), sex, smoking, obesity, recurrent disease and distance from midline were predictive of postoperative complications (P always <0·001). However, the multi‐variate analysis showed that, after adjusting for major clinical and demographic characteristics, only a previous history of pilonidal sinus surgery [odds ratio (OR): 3·41, 95% confidence interval (CI): 1·89–6·15, P < 0·001] and a growing distance from midline (OR: 26·3, 95% CI: 12·2‐56·7, P < 0·001) were independent predictors of overall postoperative complications (infection and/or recurrence) (Figure 1). More specifically, both a previous history of pilonidal sinus surgery and a growing distance from midline predicted postoperative infection (OR: 2·15, 95% CI: 1·20–3·85, P = 0·01 and OR: 4·65, 95% CI: 2·71–7·98, P = 0·02).
Table 1.
Univariate analyses stratified according to the presence of postoperative complications
| No complications (848 patients) | Complications (158 patients) | P value | |
|---|---|---|---|
| Male gender (n patients) | 514 | 116 | 0·002 |
| Age (years) | 27·7 ± 3·4 | 26 ± 6·5 | 0·4 |
| Obesity (n patients) | 66 | 42 | 0·001 |
| Smoking (n patients) | 189 | 48 | 0·03 |
| Recurrent disease | 74 | 48 | <0·001 |
| Multiple orifices (n patients) | 142 | 105 | <0·001 |
| Distance of orifice from midline (cm) | 0·2 ± 0·6 | 1·7 ± 1·3 | <0·001 |
Figure 1.
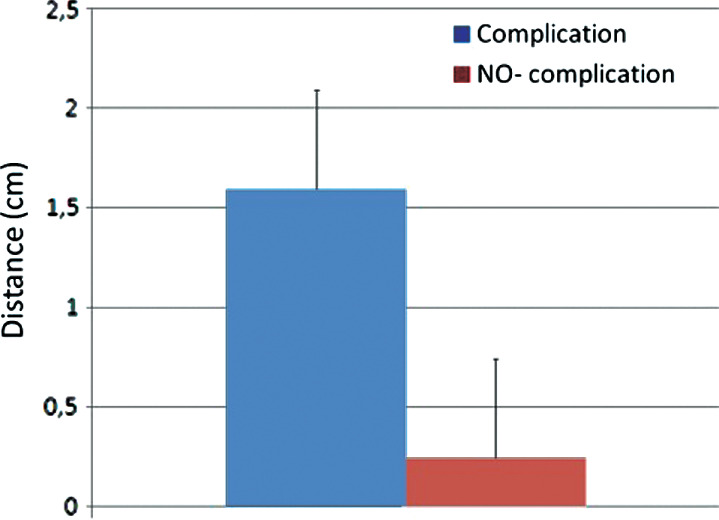
Mean distance of lateral orifice from midline stratified according to the presence of postoperative complications.
In contrast, a growing distance from midline was the only predictor of recurrence (OR: 6·54, 95% CI: 4·87–8·79, P < 0·001).
Focussing on the distance from midline, the ROC analysis (Figure 2) showed that the distance of lateral orifice from midline predicted 79·2% of complications and the Youden's test identified the best cut‐off as 2·0 cm for this variable. This cut‐off had a 73·1% positive predictive value and an 89·1% negative predictive value for the prediction of postoperative complication.
Figure 2.
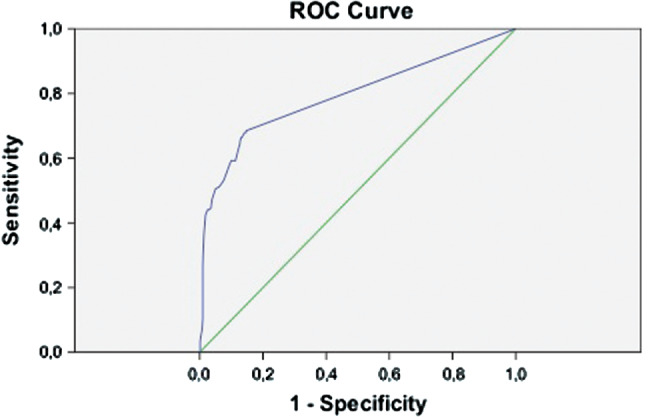
Receiver operative characteristic (ROC) analysis for prediction of postoperative complications by distance of lateral orifice from midline.
Interestingly, a separate multi‐variate analysis showed that the 2 cm cut‐off was able to predict both infection (OR: 6·57, 95% CI: 4·15–10·42, P < 0·01) and recurrence (OR: 115·9, 95% CI: 58·3–230·6, P < 0·01).
Discussion
To our best knowledge, this is the first attempt to use patient and sinus characteristics to accurately predict postoperative complications (infection and recurrence) and guide the surgeon in deciding which surgical technique to use.
The development of a sacrococcygeal pilonidal sinus, a common and well‐recognised disorder, is still a troublesome disease entity because of the high morbidity of most treatment options 4. Although many surgical methods have been proposed, no clear consensus regarding the optimal treatment has been reported in the literature.
Complete excision of the sinus is widely practised, but the treatment of the wound after excision remains controversial.
The surgical wound may be left open to heal (secondary intention), or the wound may be closed by primary closure to heal (primary intention).
Compared with secondary intention, primary closure is known to provide faster healing and faster return to work 4, 5, 6, 7, 8, 9, 10, 11. However, a high complication rate has been reported because of tissue tension. The main problems with the primary closure technique appear to be the high recurrence rate and the high infection rate. In fact, surgical site infection is not unexpected and ranges from 6% to 14% 4, 12, 13, 14, 15, 16, 17.
The problems related to midline closure have prompted surgeons to explore techniques to eliminate the tissue tension. In this setting, the aim of most off‐midline techniques is to use asymmetrical, oblique, elliptical, or lateral incisions in an attempt to keep scars out of the midline in order to overcome any tension and its related complications 4, 18, 19, 20, 21, 22, but these, unfortunately, leave deformed buttocks and visible ugly scars.
The cosmetic superiority of the midline scars and the importance of the buttocks as a major component of the concept of beauty in most cultures 9, 23 are very important considerations to be kept in mind.
The cosmetic aspect and aesthetic outcome of pilonidal sinus surgery, which are major goals for most patients, have rarely been studied in the literature. Whereas poor results have been obtained after off‐midline closure 23, 24, high cosmetic satisfaction has been shown after midline closure 2, 9, 25.
Though there is controversy about the best surgical technique, the ideal operation should provide patient care. Cosmetic appearance as well as the relief of clinical symptoms should be considered. Therefore, it would be very important to predict which patient can take aesthetic advantage of midline closure with the minimal risk of postoperative complications.
However, the current literature demonstrates that the choice of the ideal surgical technique is far from being effective.
This justifies the need for an evidence‐based decision‐making tool for everyday use that can provide accurate stratification and guidance in choosing the optimal surgical technique tailored to patient and sinus characteristics.
This would allow for deciding which patients can be treated by midline closure and which patients would benefit from off‐midline closure.
In this setting, our results may be of value as a decision‐making tool that can help surgeons reliably identify patients at high risk for postoperative complications (infection and recurrence) and apply the best surgical technique for each patient.
We found that recurrent disease and the distance of the lateral orifices from the midline are predictive of postoperative complications after excision and midline closure. Interestingly, this finding has been confirmed after adjusting all results for major clinical and demographic characteristics. Furthermore, according to Sievert H. et al. 26, the life‐style parameters of smoking and body weight do not predict postoperative complications, statistically.
Another innovative issue addressed in this study is the identification of a ‘best cut‐off’ for the prediction of postoperative complications. Indeed, with an ROC analysis we have identified a >2 cm distance of lateral orifice from the midline as a practical and easy‐to‐be‐used parameter to predict infection and recurrence.
From our results, we can state that midline closure should not be considered effective in cases of recurrent disease and/or distance of lateral orifices from midline >2 cm. As the positive predictive value was quite high (73·1%), we could determine the need for another surgical approach to avoid infection and recurrence after surgery if the distance from midline is >2 cm.
Ad hoc studies are needed to evaluate the effectiveness of off‐midline surgery or new minimally invasive techniques 27 in the sub‐group of patients with recurrent disease or the presence of a distance >2 cm between the most lateral orifice and the midline.
On the other hand, the very high negative predictive value (89·1%) clearly indicates that the <2 cm distance of lateral orifice from midline strongly rules out the occurrence of postoperative complications.
Conclusion
An evidence‐based tool for deciding on the type of surgical intervention could be developed and validated by further ad hoc prospective studies evaluating our results in comparison to different types of surgical techniques. Our results support the use of some variables (recurrent disease and the distance of the lateral orifices from the midline) as an effective way to tailor the pilonidal sinus surgery to the patient, in the attempt to obtain the best results in patient care.
Author contribution
MMi and FM were involved in designing the study. MMu, MMi, PB and GC acquired the data. MNDDM and MMi contributed the analysis and interpretation of data. MMi and MNDDM prepared the manuscript. FM and MMu performed critical revision.
References
- 1. Allen‐Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg 1990;77:123–32. [DOI] [PubMed] [Google Scholar]
- 2. Milone M, Musella M, Salvatore G, Leongito M, Milone F. Effectiveness of a drain in surgical treatment of sacrococcygeal pilonidal disease. Results of a randomized and controlled clinical trial on 803 consecutive patients. Int J Colorectal Dis 2011;26:1601–7. [DOI] [PubMed] [Google Scholar]
- 3. Doll D, Novotny A, Rothe R, Kristiansen JE, Wietelmann K, Boulesteix AL, Dusel W, Petersen S. Methylene blue halves the long‐term recurrence rate in acute pilonidal sinus disease. Int J Colorectal Dis 2008;32:181–7. [DOI] [PubMed] [Google Scholar]
- 4. Mahdy T. Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum 2008;51:1816–22. [DOI] [PubMed] [Google Scholar]
- 5. Erdem E, Sungurtekin U, Nessar M. Are postoperative drains necessary with the Limberg flap for treatment of pilonidal sinus? Dis Colon Rectum 1998;41:1427–31. [DOI] [PubMed] [Google Scholar]
- 6. Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg 2005;190:388–92. [DOI] [PubMed] [Google Scholar]
- 7. Maghsoudi H, Nezami N, Ghamari AA. Ambulatory treatment of chronic pilonidal sinuses with lateral incision and primary suture. Can J Surg 2011;54:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McCallum IJD, Peter MK, Julie B. Healing by primary closure versus open healing after surgery for pilonidal sinus systemic review and meta‐analysis. BMJ 2008;336:868–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. El‐Shaer WM. The modified gluteal sliding placation closure in the treatment of chronic pilonidal sinus. Int J Colorectal Dis 2010;25:887–94. [DOI] [PubMed] [Google Scholar]
- 10. Khaira HS, Brown JH. Excision and primary closure of piloni dal sinus. Ann R Coll Surg Engl 1995;77:242–4. [PMC free article] [PubMed] [Google Scholar]
- 11. Brasel KJ, Gottesman L, Vasilevsky CA, Members of the Evidence‐Based Reviews in Surgery Group . Meta‐analysis comparing healing by primary closure and open healing after surgery for pilonidal sinus. J Am Coll Surg 2010;211:431–4. [DOI] [PubMed] [Google Scholar]
- 12. Schoeller T, Wechselberger G, Otto A, Papp C. Definite surgical treatment of complicated recurrent pilonidal disease with a modified fasciocutaneous V‐Y advancement flap. Surgery 1997;121:258–63. [DOI] [PubMed] [Google Scholar]
- 13. Morell V, Brian LC. Surgical treatment of pilonidal disease: comparison of three different methods in fifty‐nine cases. Mil Med 1991;156:144–6. [PubMed] [Google Scholar]
- 14. Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Long‐term follow‐up. Am J Surg 1984;148:658–9. [DOI] [PubMed] [Google Scholar]
- 15. Milone M, Di Minno MN, Musella M, Maietta P, Ambrosino P, Pisapia A, Salvatore G, Milone F. The role of drainage after excision and primary closure of pilonidal sinus: a meta‐analysis. Tech Coloproctol 2013;17:625–30. [DOI] [PubMed] [Google Scholar]
- 16. Al‐Hassan HK, Francis IM, Negl EN. Primary closure or secondary granulation after excision of pilonidal sinus. Acta Chir Scand 1990;156:695–9. [PubMed] [Google Scholar]
- 17. Khatri V, Espinosa MH, Amin AK. Management of recurrent pilonidal sinus by simple V‐Y fasciocutaneous flap. Dis Colon Rectum 1994;37:1232–5. [DOI] [PubMed] [Google Scholar]
- 18. Bascom J. Pilonidal disease: origin from follicles of hairs and result of follicle removal as treatment. Surgery 1980;87:567–72. [PubMed] [Google Scholar]
- 19. Karydakis GE. Easy and successful treatment of piloni dal sinus after explanation of its causative process. ANZ J Surg 1992;62:385–9. [DOI] [PubMed] [Google Scholar]
- 20. Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg 1996;83:1452–5. [DOI] [PubMed] [Google Scholar]
- 21. Nessar G, Kayaalp C, Seven C. Elliptical rotation flap for pilonidal sinus. Am J Surg 2004;187:300–3. [DOI] [PubMed] [Google Scholar]
- 22. Bascom J, Bascom T. Utility of the cleft lift procedure in refractory pilonidal disease. Am J Surg 2007;193:606–9. [DOI] [PubMed] [Google Scholar]
- 23. Holmebakk T, Nesbakken A. Surgery for pilonidal disease. Scand J Surg 2005;94:43–6. [DOI] [PubMed] [Google Scholar]
- 24. El‐Khadrawy O, Hashish M, Ismail K, Shalaby H. Outcome of the rhomboid flap for recurrent pilonidal disease. World J Surg 2009;33:1064–8. [DOI] [PubMed] [Google Scholar]
- 25. Milone M, Musella M, Maietta P, Bianco P, Taffuri C, Salvatore G, Milone F. Intradermal absorbable sutures to close pilonidal sinus wounds: a safe closure method? Surg Today 2013. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26. Sievert H, Evers T, Matevossian E, Hoenemann C, Hoffmann S, Doll D. The influence of lifestyle (smoking and body mass index) on wound healing and long‐term recurrence rate in 534 primary pilonidal sinus patients. Int J Colorectal Dis 2013;28:1555–62. DOI: 10.1007/s00384-013-1731-8. [Epub 2013 June 20]. [DOI] [PubMed] [Google Scholar]
- 27. Milone M, Musella M, Di Spiezio SA, Bifulco G, Salvatore G, Sosa Fernandez LM, Bianco P, Zizolfi B, Nappi C, Milone F. Video‐assisted ablation of pilonidal sinus: a new minimally invasive treatment‐A pilot study. Surgery 2014;155:562–6. [DOI] [PubMed] [Google Scholar]


