Abstract
The prerequisite for a successful vitiligo epidermal grafting surgery is the stable status of the disease. We used Wood's lamp to assess vitiligo activity to determine the disease stability, surgical grafting timing and the early recognition of re‐pigmentation after grafting. Amelanotic lesions with sharply demarcated borders are typically stable and are good candidates for grafting. The re‐pigmentation was first recognised under Wood's lamp as hypochromic islands, which progressed to normally pigmented islands. For patients more prone to relapse, follow up with Wood's lamp also provides more accurate surveillance.
Keywords: Epidermal grafting, Vitiligo, Wood's lamp
Introduction
The prerequisite for a successful vitiligo epidermal grafting surgery is the stable status of the disease. However, determining vitiligo disease stability is clinically challenging. Although several methods exist, including history taking on any new lesions in the last 2 years, examination of the Koebner phenomenon, calculating the Vitiligo Disease Activity Score (VIDASCORE) and mini‐grafting test, they are not immediate or accurate 1. In a study published in February 2017, Benzekri et al. proposed the active lesions were associated with hypomelanotic appearance with poorly defined borders 1. We use Wood's lamp to determine the surgical timing based on the disease stability to detect the initial re‐pigmentation after grafting, with more accurate surveillance on the following visits. Here, we present one segmental and one non‐segmental vitiligo patient for demonstration.
Case presentation
Case 1
A 13‐year‐old boy presented with segmental vitiligo occurring for 5 years over his left chest, abdomen, arm, axilla and back. He had previously been treated with narrowband ultraviolet B (NBUVB) intermittently, but this had ultimately accentuated the contrast between the lesions and normal skin (Figure 1A). An examination using Wood's lamp showed his lesions to be amelanotic, with sharply demarcated borders (Figure 1B), corresponding to the presentation of stable lesions as reported by Benzekri et al. 1.
Figure 1.
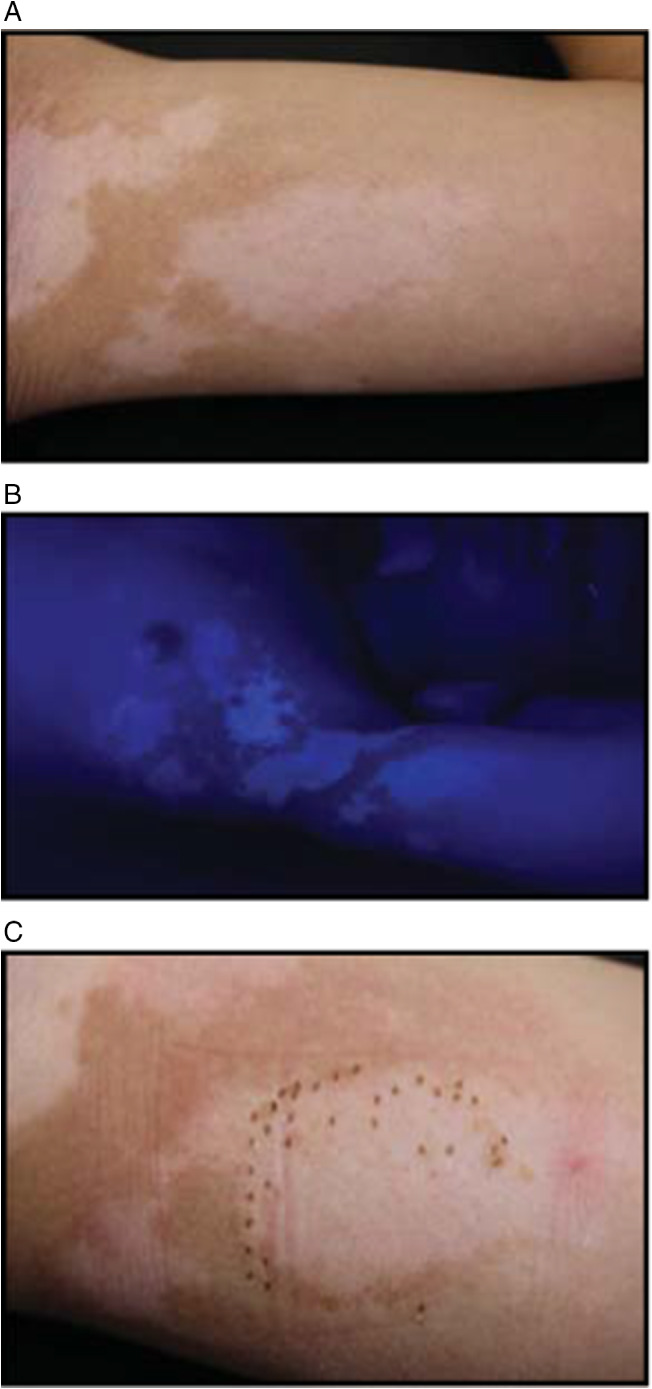
(A) Standard digital photograph taken before epidermal grafting. Previous phototherapy had accentuated the contrast between the normal pigmented skin and vitiligo lesions. (B) Photograph taken under Wood's lamp before epidermal grafting. Note the achromia and sharply defined borders, suggesting the stable status. (C) Standard digital photograph taken on postoperative day 21. Only 20% of grafts taken were noted because the patient did not refrain from exercise.
The recipient site he chose on the inner arm was prepared using an Erbium:YAG laser until pinpoint bleeding was just visible at the base. Using an automatic system (Cellutome™ Epidermal Harvesting System, Acelity, San Antonio, TX, USA), 128 epidermal micrografts were harvested from the inner thigh and were transferred to the recipient site with a non‐adherent dressing. The procedure lasted a total of 67 minutes. However, this patient had unexpected lower take rate, only about 20% on postoperative day (POD) 21, because he did not follow the instruction of refraining from exercise after the grafting (Figure 1C)
Surprisingly, the re‐pigmentation was still recognised on POD 45 under Wood's lamp, where four shades of achromic colours, hypochromic islands, pigmented islands and normal pigmented skin were mixed. The pigmented islands did not completely correspond to the initial grafts taken area (Figure 2A,B). On POD 105, the hypochromic islands had progressed to pigmented islands, even on the area where no grafts taken originally (Figure 2C,D). No Koebner phenomenon was noted in the donor or recipient sites.
Figure 2.

Standard digital photograph taken on (A) Postoperative day 45. Note the barely perceptible re‐pigmentation compared to Figure 1A without assistance with Wood's lamp. (C) Postoperative day 105. Photograph taken under Wood's lamp on (B) Postoperative day 45 and (D) Postoperative day 105. Note the sharply demarcated borders, suggesting the stable status (long arrows). Note the tetrachrome not shown by digital photography: achromic (triangle), hypochromic (broad arrows), pigmented (fine arrows) and the normal skin. The hypochromic islands had progressed to pigmented islands. The hypochromic islands may be the earliest sign of re‐pigmentation. Also note the fair re‐pigmentation in area with poor initial grafts taken.
Case 2
A 45‐year‐old gentleman presented with bilateral vitiligo lesions on his glabella, supra eyebrows and cheeks for 3 years (Figure 3A). He had epidermal grafting on his left cheek as he preferred the same protocol of case 1. The patient had nearly 100% grafts taken on postoperative week 3 and had about 75% re‐pigmentation 1 month after the grafting. However, on subsequent follow‐up visits, he had focal relapse on the glabella, which was more obviously detected under Wood's lamp. The previous grafted area on the left cheek did not appear to be apparently affected (Figure 3B). His disease became stable after 4 weeks of oral mini‐pulse steroid therapy, namely, oral dexamethasone 2·5 mg per day on 2 consecutive days, weekly, for 4 weeks. There was no relapse for 6 months postoperatively.
Figure 3.

Photographs taken under Wood's lamp. (A) Before epidermal grafting. (B) Three months after epidermal grafting. The grafted area on the left cheek appeared to be not apparently affected by the disease relapse on the glabella.
Discussion
Suction blister epidermal grafting yields good results among vitiligo surgeries but is cumbersome, time‐consuming and painful. We use Cellutome™, which applies negative pressure and heat, to harvest the epidermal micrografts. This system saves time, reduces pain and leaves no hyperpigmentation on donor sites 2. However, the prerequisite for success is still the stable status of the disease. History taking is most commonly used but is not accurate or reliable. Also, a grossly static but actually slowly progressing macule is easily overlooked, may be actually active and will not respond to grafting.
Falabella et al. first proposed the mini‐grafting test in 1995, that is, planting four to six punch minigrafts of 1·0–1·2 mm within achromic vitiligo lesions. A positive mini‐grafting test anticipates the success of the future, more extensive grafting and is probably the most accurate tool to determine disease stability 3. However, it is non‐immediate and time‐consuming. We use Wood's lamp to confirm the stability of the clinical disease preoperatively as the first critical step for vitiligo epidermal grafting. Amelanotic lesions with sharply demarcated borders are typically stable and are good candidates.
Janowska et al. observed the re‐pigmentation after use of the Cellutome™ only by a digital camera 2. Wood's lamp may help to detect early re‐pigmentation not only in the forms of pigmented islands but also in those of hypochromic islands, which is hypothesised as the first early sign of re‐pigmentation. Those hypochromic islands will likely be transformed to pigmented islands gradually over times. For example, in case 1, there were a few re‐pigmentations in the area from where the original grafts were taken. Such an early re‐pigmentation was barely perceptible without assistance with Wood's lamp. Some studies have converted Wood's lamp images to a greyscale image to increase the dynamic range 1, 4. Here, we found that re‐pigmentation is easily noted under Wood's lamp even without conversion, which is ultimately more feasible and time‐saving for daily practice.
The extent of re‐pigmentation relies not only on the grafts taken rate but the disease stability and the age of the patient. Unilateral (segmental/focal) vitiligo is the most stable form, and more than 80% respond well to grafting 3, 5. In contrast, only half of non‐segmental patients improve with surgical grafting 3, 5. In other words, younger (age < 20) patients with segmental disease can obtain better outcomes after grafting than those with non‐segmental disease and older age 5.
Moreover, since vitiligo can fluctuate anytime after the grafting, the use of Wood's lamp can survey the newly onset lesions more efficiently and accurately, especially when treating patients with non‐segmental vitiligo, like case 2.
In summary, we suggest using a non‐converted Wood's lamp in vitiligo grafting surgeries for pre‐operation disease stability confirmation, early detection of re‐pigmentation after grafting and for surveillance of the stability of the disease on follow up visits, especially for the patients with non‐segmental vitiligo. For segmental patients, even if initial grafts taken rate is lower than expected, favourable results are still possible.
Acknowledgement
Informed consent for the surgery was provided by the patient and his mother.
References
- 1. Benzekri L, Gauthier Y. Clinical markers of vitiligo activity. J Am Acad Dermatol 2017;76:856–62. [DOI] [PubMed] [Google Scholar]
- 2. Janowska A, Dini V, Panduri S, Macchia M, Oranges T, Romanelli M. Epidermal skin grafting in vitiligo: a pilot study. Int Wound J 2016;13(Suppl 3):47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Falabella R. Surgical approaches for stable vitiligo. Dermatol Surg 2005;31:1277–84. [DOI] [PubMed] [Google Scholar]
- 4. Bae JM, Han TY. A grayscale photograph with high dynamic range taken under a Wood's lamp for better recognition of vitiligo lesions. J Am Acad Dermatol 2017;76:e89–90. [DOI] [PubMed] [Google Scholar]
- 5. Gupta S, Kumar B. Epidermal grafting in vitiligo: influence of age, site of lesion, and type of disease on outcome. J Am Acad Dermatol 2003;49:99–104. [DOI] [PubMed] [Google Scholar]


