Abstract
Chronic venous diseases are the most common causes of leg ulcers. Compression treatment (CT) is a central component of venous leg ulcer (VLU) therapy along with prevention based on guidelines and clinical evidence. However, large‐scale data on the use of CT are rare. In particular, there have not yet been published nationwide data for Germany. We analysed data from a large German statutory health insurance (SHI) on incident VLU between 2010 and 2012. VLUs were identified by ICD‐10 diagnoses. The status of active disease was defined by wound‐specific treatments. Compression stockings and bandages were identified by SHI medical device codes. The overall estimated incident rate of active VLU of all insured persons was 0·34% from 2010 to 2012. Adapted to the overall German population, n = 229 369 persons nationwide had an incident VLU in 2010–2012. Among all VLU patients, only 40·6% received CT within 1 year, including 83·3% stockings, 31·8% bandages and 3·1% multi‐component compression systems. Compression rates showed significant differences by gender and age. Large regional variations were observed. Validity of data is suggested by high concordance with a primary cohort study. Although recommended by guidelines, there is still a marked under‐provision of care, with CT in incident VLUs in Germany requiring active measures.
Keywords: Compression treatment; Leg ulcers; Statutory health insurance; Regional variations; Wound care, health care research
Introduction
Chronic wounds are of considerable medical and economic interest in most countries 1. In Germany, they cause a large burden for the patients 2, 3, 4, 5, the medical system, the payers and society 6, 7.
About 37–80% of leg ulcers in the community are of vascular origin, particularly because of chronic venous insufficiency 8, 9. Compression therapy leads to significantly higher healing rates and reduced recurrence compared to non‐compression 9, 10, 11, 12. Thus, compression therapy in venous leg ulcers (VLUs) is a treatment of choice backed by scientific evidence and a Cochrane Review 9, 10. Accordingly, compression therapy for VLUs has been included in most international guidelines, such as the German treatment guideline on VLU 9, the British guideline as well as several the nursing guidelines 13, 14. Finally, the use of compression therapy has been shown to be of high cost effectiveness in VLUs 15. The lifetime costs from the full societal perspective for patients with VLUs plus compression were lower than for such persons without compression therapy.
In spite of the large evidence from studies 10, 16 and the high level of recommendation from guidelines concerning the benefit of compression therapy 9, clinical reports and health service studies indicate that the use of compression therapy of VLUs in routine care is not sufficient 8, 17, 18, 19, 20. Despite the effectiveness of compression therapy, published data show that there still is an underprovision of care with compression 16. The majority of patients with VLUs (between 50% and 60%) received no compression therapy, although a consistent and properly applied compression increases the probability of cure, and the risk of recurrence can be minimised. International studies show similar results, with a small proportion of patients receiving compression treatment (CT) 18, 19.
However, the published data are derived from local or regional surveys, estimations or clinical reports but not from large‐scale evaluations. Until now, there is a complete lack of countrywide data on the use of CT for VLUs in Germany.
The current study was conducted in order to obtain valid data on the use of compression therapy among patients with VLUs across the country. As compression stockings and bandages are reimbursed by the statutory health insurances (SHIs), their prescriptions are completely recorded in the German SHI claims datasets. Previous studies have shown that there is a high validity and feasibility in using these large and mostly unselected data for many health research questions 21, 22.
Methods
Study population and study cohort
About 90% of the German population is insured by 124 different SHI providers [in 2015 23]. Analysis of secondary data from a large German nationwide SHI, the Barmer GEK, included 9·1 million insured persons in 2012, corresponding to about 11% of the German population with SHI status.
The identification of an incident VLU was based on the following criteria:
Diagnosis of VLU: Individuals in outpatient or inpatient care with VLUs were identified by the International Classification of Diseases (ICD‐10) (venous: I83.0 ‘varicose of lower limb extremities with ulceration’, I83.2 ‘varicose of lower limb extremities with ulceration and infection’, I87.0 ‘post‐thrombotic syndrome with ulceration’). The health care delivery system in Germany is institutionally separated between public health services, outpatient care (ambulatory primary care) and inpatient care (hospital‐based care) 24. Persons with arterial occlusive diseases like arterial leg ulcers and mixed leg ulcers were excluded from analysis.
Status of incident disease: The incident cohort consists of all insured members in 2010 who did not show criteria of VLUs in 2008 and 2009 and who presented a target leg ulcer in the observed period from 2010 to 2012. For historical reasons, the German health care system administration is based on a quarter of the year. At least 1 day of insurance coverage in each quarter was defined as qualifying for the incident status. A detailed description of the methodology of how incident cases were identified is published elsewhere 25.
Status of active disease: Patients were considered as having active disease when there was at least one additional prescription of a specific wound‐relevant material.
Compression therapy was identified by specific SHI medical device codes [specific national standard identification codes by therapeutic appliances or product‐specific central Pharmaceutical Numbers (PZN)]. At least one prescription within the defined wound duration plus 12 months before the wound beginning and 12 months after wound healing was considered. The use of compression therapy before and after the active wound phase is also recommended in national and international guidelines 9, 13, 14.
In SHI, any clinical wound data and, hence, the wound duration – the period between the development and the wound healing – are not included. Therefore, the wound duration was assumed when defined specific wound‐relevant material in combination with a wound‐relevant diagnosis were coded (see also identification criteria 3). The ‘last’ prescription was defined as 12‐month free prescription observation period. The year 2013 served as a follow‐up observation period for the identification of the ‘last’ prescription.
Guidelines and ethics
The study was conducted according to national guidelines for the use of administrative and epidemiology databases 26, 27. Based on the guidelines, no approval of an ethics committee is required for such secondary data.
Statistical analysis
The frequency of compression therapy in patients with incident VLUs was analysed overall and by age, gender and regions, with a maximum observation period of 1 year. Differences by age and gender were calculated with a two‐way Chi‐square with a significance level of 0·05. Incidence rates are reported as percent values with their corresponding 95% confidence intervals (95% CI) and standardised according to the age and sex distribution of the German population in 2012 (Interpolated German General Population Statistics from 31 December 2012, provided by the German Federal Statistical Office) 28. For calculating standardised rates, we used the method of direct standardisation. All analyses were performed using statistical analysis systems SAS Version 9.2 (SAS Institute Inc. Cary, NC).
Results
Baseline characteristics – study cohort
From 2010 to 2012, n = 24 735 out of n = 748 644 [0·34% (95% CI 0·34–0·35)] persons insured in 2010 across the German states and regions were identified as having a wound‐relevant diagnosis‐free period between 2008 and 2009 and showing an incident VLU (Figure 1). The incidence rate in 2012 was 0·16% (n = 2011). The percentage of women was 63·7% and 36·3% men, with an average age of 74 years. Adapted to the overall German population, n = 204 793 persons nationwide had an incident VLU in the period 2010–2012 and n = 98 301 persons in 2012.
Figure 1.
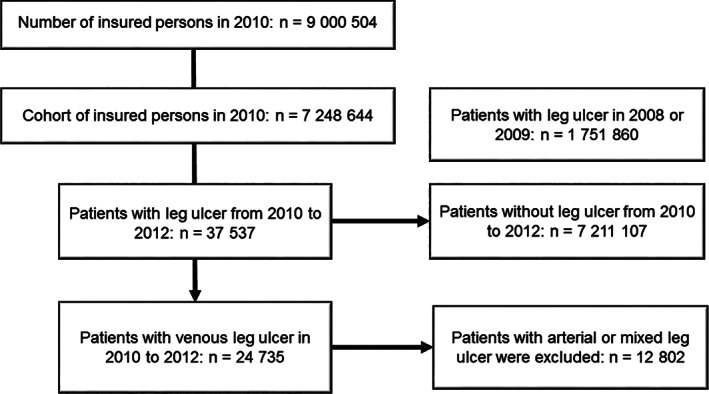
Sampling frame.
Prescription of CT
Across Germany, only 40·6% of all patients received at least one CT in the observed period (Figure 2). Among these, 83·3% were stockings, 31·8% were bandages and 3·1% were multi‐component compression systems (not additive – multiple treatments were observed).
Figure 2.
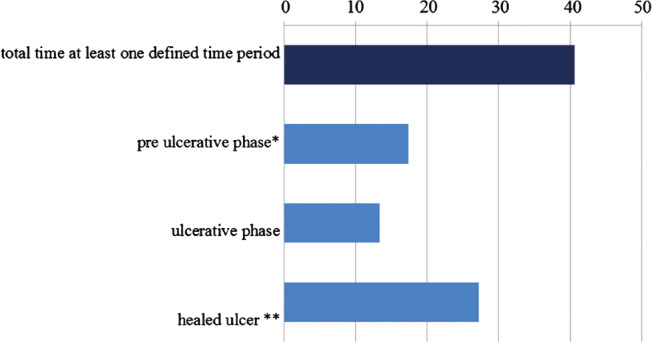
Proportion (%) of at least one compression therapy per patient with venous leg ulcer in Germany, 2010–2012 (n = 24 735 – not additive, multiple prescription per patient were observed).
CTs were differentiated by the respective wound phase and defined as (a) pre‐ulceration phase, (b) ulcerative phase and (c) healed ulcer. Of the persons with a VLU, 17·4% received compression therapy before the active wound phase; 13·4% had a prescription of compression therapy during the wound duration; and 27·3% after this period (Figure 2). Considering the time during and after the active wound phase combined, 33·6% of the patients received at least one type of wound compression therapy.
Rates of compression therapy showed significant differences between gender and age. More women (42·0%) than men (38·1%) received compression therapy compared to the patients with a VLU without compression therapy (P = 0·001). The percentage was higher in the age group between 30 and 50 years (≥46%) compared to higher age groups, above 70 years (≤38%).
Regional variations in Germany
Large variations on a state level of patients with VLUs receiving at least one compression therapy were found, with the greatest proportions prescribed in Bremen (48·0%) and Hamburg (46·5%) and the smallest numbers in Saarland (36·2%) and Bavaria (37·7%) (Figure 3).
Figure 3.
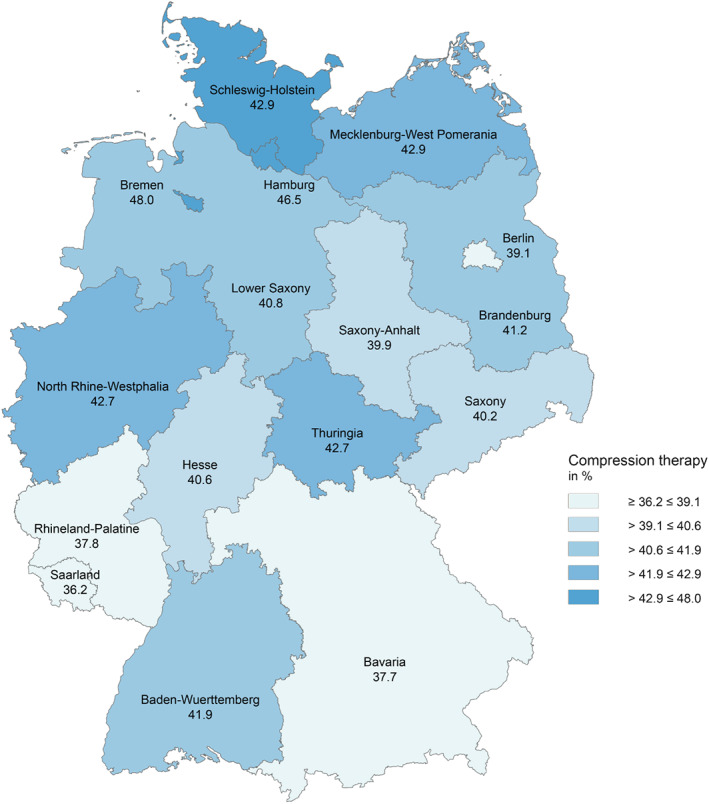
Regional differences of patients with venous leg ulcers receiving at least one compression therapy in Germany, 2009–2012 (n = 24 703).
Discussion
This study was conducted in order to obtain the first large‐scale data on the use of CT for VLUs in Germany. As compression therapy is a standard of care supported by clinical evidence and guideline recommendations, the overall rate of just 41% of patients with VLUs receiving compression therapy is far too low. Therefore, there is an undersupply with respect to compression therapy of patients with VLUs in Germany. The use of compression therapy in patients with VLUs can be regarded as a relatively reliable indicator of guideline‐based wound care, and it is to be charged as sufficiently valid at the level of SHI data. Thus, there is need for further action in order to establish stronger guideline‐compliant therapy with compression systems in the management of patients with VLUs.
The marked variation of compression therapy in different regions suggests disparities in the quality of care. It is remarkable that there is neither sufficient CT in the active wound phase nor in the phases before wound exacerbation or in the aftercare. As there is clear indication for CT in all three phases, the results reflect an unnecessarily high level of risk for wound development as well as recurrence.
Compression stockings provide the largest proportion of compression therapy with 83%. Multi‐component compression systems show higher healing rates than compression therapy with only one component, for example, short stretch compression bandages 10, 15, 29, and have been available since 2000 in Germany. Despite this strong evidence of effectiveness, the multi‐component systems show the lowest proportion of prescription. It can be assumed that multi‐component systems are unknown among the medical community, or their benefits are not sufficiently present. This insufficient knowledge was also confirmed in a German‐wide study by Protz et al. 20 Besides physician factors, patient factors could also be a reason for the low rates of compression therapy as some might have not refilled their prescriptions due to a lack of comfort and adherence.
To our knowledge, this is the first nationwide large, mostly unselected study reflecting real‐world conditions of care. The analysed administrative data are based on just one of several health insurance providers in Germany. Differences between the several SHI insurances members with respect to age, gender, socioeconomic status and morbidity may also differentially impact the utilisation of health care resources 30, 31, 32.
An expected limitation of the present analysis is the origin of data deriving from sick funds, which do not permit control of clinical parameters. However, the proportion of patients receiving CT in a previous analysis from the metropolitan area of Hamburg (47%) was in the same range as data from a primary cohort study (59%) by Herberger et al. in 2012 8, suggesting convergent validity. Concerning international studies, a low proportion of patients receiving CT (50–60%) was also described in England and France 18, 19.
Additionally, the proportion of multi‐component systems, stockings and compression bandages may have been under‐estimated because only those prescriptions were identified that were settled via pharmacies. Data of home‐care companies or medical supply stores were not available to the sick fund claim data. Therefore, the actual amount of prescribed compression therapy might be mildly higher. To date, no data on this proportion have been published. However, information obtained from internal sick fund sources indicates that this rate is below 20%. The ‘wound duration’ might differ from the actual wound duration. The observed time for obtaining compression therapy was extended. However, similar results on wound durations were also reported in other studies 33.
Contraindications for compression therapy can be peripheral occlusive arterial disease or sensory disturbances of the extremities 34. The rate of contraindications is expected to be low as patients with arterial or mixed leg ulcers in this cohort were ruled out. Thus, the optimal rate should be above 90% or more.
Conclusion
In total, the low rate of prescriptions for compression systems in VLU treatment indicates the need for action. Awareness concerning the essential indication for compression of patients at risk for VLU and the insight that CT for VLU is simple and safe must be actively increased among the medical community, the patients and the payers. An increase in the implementation deficit and knowledge of the compression therapy can shorten the healing time, positively affect the quality of life and reduce health care costs. For this reason, our results emphasise the importance of the intensified implementation of the German guideline on CT for VLUs 9. Furthermore, expert knowledge and therapy training among users and prescribers as well as patient training are necessary. Moreover, standardised trainings and large campaigns on the use of compression therapy for all care providers must be implemented.
Acknowledgements
We thank Barmer GEK for collaboration and allocation of data. We also gratefully acknowledge our team for support in publication management, Verena Heimann, Mario Gehoff and Christine Duval. KH, KP, GG have no conflicts of interest to declare. MA has received research grants and/or honoraries for consulting and/or scientific lectures for 3 M, Bayer Healthcare, Beiersdorf, Birken, Bode, B. Braun, BSN, BVmed, Coloplast, DAK, Diabet concept, Gerromed, GlaxoSmithKline, Johnson&Johnson, Lohmann&Rauscher, Medi, Medovent, Mölnlycke, Sanofi‐Aventis, Smith&Nephew, Spirig, Schülke&Mayr, Söring, Sorbion, Systagenix, Urgo.
References
- 1. European Wound Management Association (EWMA) . Position document: hard‐to‐heal wounds: a holistic approach [Internet]. 2008. URL http://ewma.org/fileadmin/user_upload/EWMA/pdf/Position_Documents/2008/English_EWMA_Hard2Heal_2008.pdf [accessed on 7 July 2015].
- 2. Herberger K, Rustenbach SJ, Haartje O, Blome C, Franzke N, Schäfer I, Radtke M, Augustin M. Quality of life and satisfaction of patients with leg ulcers‐results of a community‐based study. Vasa 2011;40:131–8. [DOI] [PubMed] [Google Scholar]
- 3. Augustin M, Herberger K, Rustenbach SJ, Schäfer I, Zschocke I, Blome C. Quality of life evaluation in wounds: validation of the Freiburg Life Quality Assessment‐wound module, a disease‐specific instrument. Int Wound J 2010;7:493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blome C, Baade K, Debus ES, Price P, Augustin M. The “Wound‐QoL”: a short questionnaire measuring quality of life in patients with chronic wounds based on three established disease‐specific instruments. Wound Repair Regen 2014;22:504–14. [DOI] [PubMed] [Google Scholar]
- 5. Augustin M, Blome C, Zschocke I, Schäfer I, Koenig S, Rustenbach SJ, Herberger K. Benefit evaluation in the therapy of chronic wounds from the patients' perspective‐development and validation of a new method. Wound Repair Regen 2012;20:8–14. [DOI] [PubMed] [Google Scholar]
- 6. Augustin M, Brocatti LK, Rustenbach SJ, Schäfer I, Herberger K. Cost‐of‐illness of leg ulcers in the community. Int Wound J 2014;11:283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Purwins S, Herberger K, Debus ES, Rustenbach SJ, Pelzer P, Rabe E, Schäfer E, Stadler R, Augustin M. Cost‐of‐illness of chronic leg ulcers in Germany. Int Wound J 2010;7:97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Herberger K, Rustenbach SJ, Grams L, Münter KC, Schäfer E, Augustin M. Quality‐of‐care for leg ulcers in the metropolitan area of Hamburg – a community‐based study. J Eur Acad Dermatol Venereol 2012;26:495–502. [DOI] [PubMed] [Google Scholar]
- 9. German Society of Phlebology . Guidelines on diagnosis and therapy of venous leg ulcers [Internet]. 2008. URL http://www.phlebology.de/leitlinien‐der‐dgp‐mainmenu/171‐diagnostik‐und‐therapie‐des‐ulcus‐cruris‐venosum [accessed on 7 July 2015].
- 10. O'Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012;11:CD000265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nelson EA, Bell‐Syer SEM. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev 2014;9:CD002303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Partsch H. Compression therapy in leg ulcers. Rev Vasc Med 2013;1:9–14. [Google Scholar]
- 13. Scottish Intercollegiate Guidelines Network (SIGN) . Management of chronic venous leg ulcers – a national clinical guideline [Internet]. Edinburgh: NHSScotland, 2010. URL http://www.sign.ac.uk/pdf/sign120.pdf [accessed on 7 July 2015]. [Google Scholar]
- 14. Royal College of Nursing . The management of patients with venous leg ulcers – clinical practice Guidelines [Internet]. Wales: RCN, 2000. URL http://www.rcn.org.uk/__data/assets/pdf_file/0004/107941/001269.pdf [accessed on 7 July 2015]. [Google Scholar]
- 15. Korn P, Patel ST, Heller JA, Deitch JS, Krishnasastry KV, Bush HL, Kent KC. Why insurers should reimburse for compression stockings in patients with chronic venous stasis. J Vasc Surg 2002;35:950–7. [DOI] [PubMed] [Google Scholar]
- 16. Nelson EA. Bell‐Syer SE compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev 2012;8:CD002303. [DOI] [PubMed] [Google Scholar]
- 17. Rabe E, Hertel S, Bock E, Hoffman B, Jockel K‐H, Pannier F. Therapy with compression stockings in Germany – results from the Bonn Vein Studies. J Dtsch Dermatol Ges 2013;11:257–61. [DOI] [PubMed] [Google Scholar]
- 18. Srinivasaiah N, Dugdall H, Barrett S, Drew PJ. A point prevalence survey of wounds in north‐east England. J Wound Care 2007;16:413–6, 418–9. [DOI] [PubMed] [Google Scholar]
- 19. Chaby G, Senet P, Ganry O, Caudon A, Thuillier D, Debure C, Meaume S, Truchetet F, Combemale P, Skowron F, Joly P, Lok C. Prognostic factors associated with healing of venous leg ulcers: a multicentre, prospective, cohort study. Br J Dermatol 2013;169:1106–13. [DOI] [PubMed] [Google Scholar]
- 20. Protz K, Heyer K, Dörler M, Stücker M, Hampel‐Kalthoff C, Augustin M. Compression therapy: scientific background and practical applications. J Dtsch Dermatol Ges 2014;12:794–801. [DOI] [PubMed] [Google Scholar]
- 21. Hoffmann F. Review on use of German health insurance medication claims data for epidemiological research. Pharmacoepidemiol Drug Saf 2009;18:349–56. [DOI] [PubMed] [Google Scholar]
- 22. Swart E, Ihle P, Geyer S, Grobe T, Hofmann W. GPS – good practice secondary data analysis. Working Group for the Survey and Utilization of Secondary Data (AGENS) of the German Society for Social Medicine and Prevention (DGSMP). Gesundheitswesen 2005;67:416–21. [DOI] [PubMed] [Google Scholar]
- 23. GKV‐Spitzenverband, National Association of Statutory Health Insurance Funds . Kennzahlen der gesetzlichen Krankenversicherung [Internet]. 2015. URL www.gkv‐spitzenverband.de/media/grafiken/gkv_kennzahlen/kennzahlen_gkv_2015_q1/GKV_Kennzahlen_Booklet_Q1‐2015_300dpi_2015‐06‐29.pdf [accessed on 7 July 2015].
- 24. Busse R, Blumel M. Germany: health system review. Health Syst Transit 2014;16:1–296. [PubMed] [Google Scholar]
- 25. Heyer K, Herberger K, Protz K, Glaeske G, Augustin M. Epidemiology of chronic wounds in Germany: analysis of statutory health insurance data. Wound Repair Regen 2015. DOI: 10.1111/wrr.12387 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26. Swart E. Health care utilization research using secondary data. In: Janssen C, Swart E, Von Lengerke T, editors. Health care utilization in Germany – theory, methodology, and results. New York, NY: Springer Science + Business Media, 2014:63–8. [Google Scholar]
- 27. German Society for Epidemiology . Guidelines and recommendations to assure good epidemiologic practice (GEP) [Internet]. 2008. URL http://dgepi.de/fileadmin/pdf/GEP_LL_english_f.pdf [accessed on 7 July 2015].
- 28. Statistisches Bundesamt Destatis . Bevölkerungsstand [Internet]. 2012. URL www.destatis.de [accessed on 7 July 2015].
- 29. O'Meara S, Tierney J, Cullum N, Bland MJ, Franks PJ, Mole T, Scriven M. Four layer bandage compared with short stretch bandage for venous leg ulcers: systematic review and meta‐analysis of randomised controlled trials with data from individual patients. BMJ 2009;338:b1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoffmann F, Icks A. Structural differences between health insurance funds and their impact on health services research: results from the Bertelsmann Health‐Care Monitor. Gesundheitswesen 2012;74:291–7. [DOI] [PubMed] [Google Scholar]
- 31. Schnee M. Socio‐economic structures and morbidity in statutory health insurance companies. In: Böcken J, Braun B, Amhof R, editors. Gesundheitsmonitor 2008. Gütersloh: Verlag Bertelsmann Stiftung, 2008:88–104. [Google Scholar]
- 32. Jaunzeme J, Eberhard S, Geyer S. How “representative” are SHI (statutory health insurance) data? Demographic and social differences and similarities between an SHI‐insured population, the population of Lower Saxony, and that of the Federal Republic of Germany using the example of the AOK in Lower Saxony. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013;56:447–54. [DOI] [PubMed] [Google Scholar]
- 33. Läuchli S, Bayard I, Hafner J, Hunziker T, Mayer D, French L. Healing times und the need for hospitalization for leg ulcers of different etiologies. Hautarzt 2013;64:917–22. [DOI] [PubMed] [Google Scholar]
- 34. Wienert V, Gerlach H, Gallenkemper G, Kahle B, Marshall M, Rabe E. Medical compression stockings: guideline of the German Society of Phlebology. Vasomed 2007;19:65–71. [DOI] [PubMed] [Google Scholar]


