Abstract
Skin tears cause pain, increased length of stay, increased costs, and reduced quality of life. Minimal research reports the association between skin tears, and malnutrition using robust measures of nutritional status. This study aimed to articulate the association between malnutrition and skin tears in hospital inpatients using a yearly point prevalence of inpatients included in the Queensland Patient Safety Bedside Audit, malnutrition audits and skin tear audits conducted at a metropolitan tertiary hospital between 2010 and 2015. Patients were excluded if admitted to mental health wards or were <18 years. A total of 2197 inpatients were included, with a median age of 71 years. The overall prevalence of skin tears was 8.1%. Malnutrition prevalence was 33.5%. Univariate analysis demonstrated associations between age (P ˂ .001), body mass index (BMI) (P < .001) and malnutrition (P ˂ .001) but not gender (P = .319). Binomial logistic regression analysis modelling demonstrated that malnutrition diagnosed using the Subjective Global Assessment was independently associated with skin tear incidence (odds ratio, OR: 1.63; 95% confidence interval, CI: 1.13‐2.36) and multiple skin tears (OR 2.48 [95% CI 1.37‐4.50]). BMI was not independently associated with skin tears or multiple skin tears. This study demonstrated independent associations between malnutrition and skin tear prevalence and multiple skin tears. It also demonstrated the limitations of BMI as a nutritional assessment measure.
Keywords: malnutrition, nutrition status, risk factor, skin tear, skin tears
1. INTRODUCTION
Skin tears are a significant health issue, with skin tear prevalence from 3.3% to 24% across populations, including acute care, home care, and long‐term care.1, 2 Increased pain, chronic wound development, hospital length of stay, economic costs, reduced mobility, and reduced overall quality of life are associated with skin tears.3, 4 However, skin tears appear to be an understated, under‐researched injury, and the cost of skin tears on patients and the broader health care system appear undervalued.5, 6
Skin tears can occur at any life stage and on any part of the body; most are commonly found in neonates and older adults in the extremities.7, 8 Blunt trauma during transfers, bathing, or falls are acknowledged as primary contributors; however, in up to 50% of cases, the aetiology of skin tears is unknown.9, 10, 11 Multiple risk factors for the development of skin tears have been identified, including advanced age, history of skin tears, assistance with activities of daily living, impaired cognition, and dry or bruised skin.1, 2, 12 In addition, many older adults have comorbidities that can contribute to polypharmacy, an identified skin tear risk factor, as well the taking of medications such as steroidal and non‐steroidal anti‐inflammatory drugs, which can compromise skin integrity.2, 8
Research has found the prevalence of protein energy malnutrition (malnutrition) within hospitalised individuals within Australia (and internationally) to be typically 20% to 35%.5, 13, 14, 15, 16 The relationship between pressure injuries and malnutrition has been well established within acute, long‐term, and home care settings; malnutrition is identified as the most strongly associated nutritional risk factor for development and severity.17, 18, 19, 20 The association between malnutrition in pressure injuries is thought to be multifactorial, with an increase in bony prominences in malnourished patients and poorer skin integrity (tensile strength, nutrient delivery, oxygenation, loss of underlying fat, and dermal thickness,). However, there is minimal literature exploring the association of skin tears and malnutrition, with only 1 study reviewing key macro‐ and micronutrients.21, 22, 23, 24, 25 Small studies in specific populations suggest an association between skin tears and rudimentary measures of nutritional status, such as malnutrition nutrition screening tools, low body mass index (BMI), or feeding protocols.5, 9, 26 In the absence of comprehensive supporting evidence, international consensus recommendations/treatment guidelines note the need to optimise nutrition and hydration for the prevention of skin tears.25, 27, 28, 29 Consequently, there is a need to explore this association using robust measures of nutritional status and to account for potential confounding factors.
Although there is no gold standard for malnutrition diagnosis, diagnostic accuracy studies and international guidelines recognise the Subjective Global Assessment (SGA) as a valid, reliable, sensitive, and specific measure to determine nutritional status in hospital inpatients, and it has been used in similar studies related to pressure injuries.20, 30, 31, 32, 33, 34 To assess nutrition status, the SGA involves an individual assessment of weight history, dietary intake, gastrointestinal symptoms, and functional capacity, combined with a physical assessment of subcutaneous fat, muscle wasting, presence of oedema, and ascites related to malnutrition.34 This measure is suggested to have higher concurrent and predictive validity then other measures applied in older hospitalised inpatients.30
Inadequate nutrition and hydration has been suggested as a modifiable intrinsic risk factor for skin tears in multiple studies.25, 35, 36 Demonstration of an independent relationship between malnutrition and skin tears may support clinical practice interventions. These interventions may inform changes to reduce the prevalence and incidence of skin tears and improve the management of skin tears in the hospital setting. Therefore, this study aims to determine if there is an association between malnutrition and skin tears in hospital inpatients.
2. METHODS
A cross‐sectional study design was used to evaluate pooled data from 6 single‐day annual point prevalence audits. A convenience sample of all audits conducted between 2010 and 2015 across all wards of a 600‐bed metropolitan tertiary hospital in Brisbane, Australia, was available for evaluation. All hospital inpatients ≥18 years of age were invited to participate in each yearly audit. Demographic and clinical information data (age, gender, ward location, height, weight, nutritional status, and BMI) were collected using standard templates by trained staff for all admitted inpatients hospital‐wide on a single day. The Queensland Patient Safety Bedside Audit (QBA) was conducted by trained auditors; malnutrition audit data (SGA, height, and weight) were collected by trained dieticians; and skin tear data were collected by trained nurses and then confirmed and classified by specialised wound management nursing staff. Dieticians undertook SGA workshops and inter‐rater reliability training prior to the audit day (ranging from 75% to 100%). Weight and SGA rating data were collected only if it had been recorded within a week of the date of audit to ensure accuracy.
Patients with missing variables, for example, those who did not consent to participate in the malnutrition assessment, were included in the final sample. Missing data were obtained from patient medical records retrospectively, using weight/height/SGA data documented within 7 days on either side of audit day, as part of a previous ethics‐approved study.
Nutrition status was diagnosed using SGA, with patients classified as well nourished (SGA A), mild‐moderately malnourished (SGA B), or severely malnourished (SGA C). Patients “at risk” or “suspected” of malnutrition without adequate supporting evidence were categorised as “A” due to the need to avoid over‐diagnosis of malnutrition in a case‐based reimbursement funding environment. Patients classified as SGA B or C were then grouped into a “malnourished” category for regression analysis. Patient weight and height were documented on the day of or prior to the audit day and were used to calculate BMI. BMI categories were defined using the World Health Organisation classifications (underweight <18.5 kg/m2, healthy weight 18.5‐24.99 kg/m2, overweight 25‐29.99 kg/m2, obese 30‐39.99 kg/m2, and morbidly obese >40 kg/m2).37
While there is no current international skin tear classification system accepted and used universally, there are 3 widely used systems: Payne‐Martin, Skin Tear Classification System (STAR), and International Skin Tear Advisory Panel (iSTap).27, 38, 39 This facility categorises skin tears using the STAR classification system, which defines a skin tear within 5 skin tear categories: 1a: A skin tear where the edges can be realigned to the normal anatomical position (without undue stretching), and the skin or flap colour is not pale, dusky, or darkened; 1b: A skin tear where the edges can be realigned to the normal anatomical position (without undue stretching), and the skin or flap colour is pale, dusky, or darkened; 2a: A skin tear where the edges cannot be realigned to the normal anatomical position, and the skin or flap colour is not pale, dusky, or darkened; 2b: A skin tear where the edges cannot be realigned to the normal anatomical position, and the skin flap or colour is pale, dusky, or darkened; and 3: A skin tear where the skin flap is completely absent.39
2.1. Statistical analysis
Data were analysed using IBM SPSS Statistics for Windows (Version 23, IBM Corp., Armonk, New York). Data analysed included: number of patients in each year's audit, number of patients consenting to be included in audit and data publications, patient demographics (age, gender), number of skin tears, number of skin tears per patient, location of skin tears, skin tear classification, nutrition status, and BMI. Descriptive statistics were entered to describe sample demographics (including median, range, frequency, and percentages). Independent variables (age, gender, location of skin tear, classification of skin tear, nutritional status, BMI category) were assessed by the Pearson's χ 2 test, and for smaller samples (expected cell counts were less than 5), Fisher's exact test was conducted. Logistic regression analysis was conducted to adjust for statistically significant continuous (age, BMI) and categorical variables (gender, nutrition status) and to determine the association of effects with skin tears as the dependent variable reporting odds ratios (ORs) and 95% confidence intervals (95% CIs). Significance was assessed using a P value of .05.
2.2. Ethics
Ethical approval was granted by The Prince Charles Hospital Research, Ethics and Governance Committee, Approval number [HREC/17/QPCH/71].
3. RESULTS
A total of 2197 inpatients were included across 6 single‐day audits conducted between 2010 and 2015. Demographic characteristics demonstrate a predominantly male, older inpatient population (Table 1).
Table 1.
Demographics and characteristics of documented skin tears
| % (n) | ||
|---|---|---|
| Gender (n = 2197) | Male | 54.6% (1200) |
| Female | 45.4% (997) | |
| Age (n = 2197) | Range (18‐99) | — |
| Median (71) | — | |
| Skin tear documented (n = 2197) | No skin tear | 91.9% (2020) |
| Skin tear | 8.1% (177) | |
| Skin tears per patient (n = 177) | 1 Skin tear | 5.0% (109) |
| >1 Skin tear | 3.1% (68) | |
| Skin tear category (n = 330) | 1a | 6.4% (21) |
| 1b | 16.4% (54) | |
| 2a | 3.6% (12) | |
| 2b | 34.8% (115) | |
| 3 | 38.8% (128) | |
| Skin tear location (n = 330) | Upper extremities | 49.4% (163) |
| Lower extremities | 47.6% (157) | |
| Back/trunk | 1.5% (5) | |
| Head | 0.6% (2) | |
| Other | 0.9% (3) | |
| Nutrition status (n = 2003) | Well nourished (SGA A) | 66.5% (1331) |
| Mild/moderately malnourished (SGA B) | 27.8% (556) | |
| Severely malnourished (SGA C) | 5.8% (116) | |
| BMI category (n = 2130) | Underweight (<18.5 kg/m2) | 7.7% (163) |
| Healthy (18.5‐24.9 g/m2) | 36.7% (782) | |
| Overweight (25‐29.9 kg/m2) | 27.3% (581) | |
| Obese (30‐40 kg/m2) | 23.8% (506) | |
| Morbidly obese (>40 kg/m2) | 4.6% (98) | |
Abbreviations: BMI, body mass index; SGA, Subjective Global Assessment.
3.1. Skin tear and malnutrition prevalence
The overall average point prevalence of patients with skin tears within the hospital setting was 8.1%, averaged over the 6‐year period, with no apparent trends in prevalence (5.5% in 2010, 9.3% in 2011, 9.9% in 2012, 6.1% in 2013, 7.7% in 2014, 9.6% in 2015; χ 2 = 8.66; df = 5; P = .124). Malnutrition was diagnosed in 33.5% of patients audited across the 6‐year period, with a significant reduction in the point prevalence of malnutrition across these years (45.6% in 2010, 35.2% in 2011, 33.4% in 2012, 30.3% in 2013, 30.1% in 2014, 26.5% in 2015; χ 2 = 32.70; df = 5; P < .001). Although there was a clear association between malnutrition diagnosed using the SGA and BMI (χ 2 = 413.221, df = 4, P < .001), it is important to note that malnourished patients were observed across all BMI categories (Figure 1).
Figure 1.
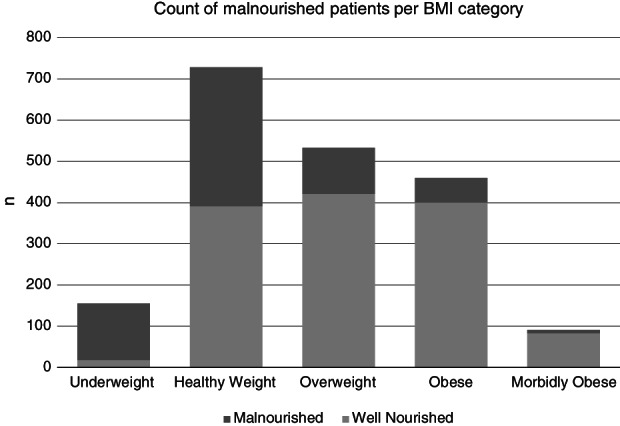
Count of malnourished patients per body mass index (BMI) category
Table 2 demonstrates the association between independent variables of interest and skin tears.
Table 2.
Association between skin tears and independent variables of age, gender, BMI, and malnutrition
| Independent variable | Skin tears | Multiple skin tears | ||||
|---|---|---|---|---|---|---|
| No | Yes | P | No | Yes | P | |
| Age, median (range; IQR) | 69 (18‐99; 25) | 81 (26‐99; 14) | a < .001 | 70 (18‐99; 25) | 81 (58‐98; 14) | a < .001 |
| Female, n (%) | 923 (45.7%) | 74 (41.8%) | χ2 (1) .991; .319b | 977 (45.9%) | 20 (29%) | χ2 (1) 7.725; .005b, c |
| BMI, median (range; IQR) | 25.96 (9.79‐107.15; 8.87) | 23.73 (12.31‐50.87; 6.94) | a < .001 | 25.80 (9.79‐107.15; 8.86) | 23.90 (15.61‐50.87; 6.95) | a.006 |
| BMI category, n (%) | χ2(4) 26.299; <.001b | χ2(4) 8.868; .064b | ||||
| <18.5 | 142 (7.3%) | 21 (11.9%) | 155 (7.5%) | 8 (11.6%) | ||
| 18.5‐24.9 | 699 (35.8%) | 83 (47.2%) | 749 (36.3%) | 33 (47.8%) | ||
| 25‐29.9 | 533 (27.3%) | 48 (27.3%) | 563 (27.3%) | 18 (26.1%) | ||
| >30 | 483 (24.7%) | 23 (13.1%) | 497 (24.1%) | 9 (13.0%) | ||
| >40 | 97 (5.0%) | 1 (0.6%) | <.001 | 97 (4.7%) | 1 (1.4%) | |
| Nutrition status, n (%) | χ2(2) 34.499; <.001b | χ2(2) 22.930; <.001b | ||||
| SGA A | 1253 (68.3%) | 78 (46.2%) | 1307 (67.3%) | 24 (38.7%) | ||
| SGA B | 479 (26.1%) | 77 (45.6%) | 523 (26.9%) | 33 (53.2%) | ||
| SGA C | 102 (5.6%) | 14 (8.3%) | 111 (5.7%) | 5 (8.1%) | ||
Abbreviations: BMI, body mass index; SGA, Subjective Global Assessment; IQR, Interquartile range.
Mann‐Whitney U‐test.
Pearson χ 2 test.
One cell (10.0%) has expected count less than 5. The minimum expected count is 3.17.
Logistic regression analysis of risk factors associated with skin tears is shown in Table 3. Variance Inflation Factor (VIF) values demonstrated no multicollinearity between variables included in the final logistic regression model. After adjusting for age, gender, and BMI, the logistic regression analysis model demonstrated a statistically and clinically significant relationship between malnutrition and skin tears (Table 3). Increasing age also demonstrated a small but statistically significant positive association with skin tears after adjusting for covariates. BMI was not independently associated with skin tears after adjusting for age, gender, and malnutrition. A second logistic regression model demonstrated that malnutrition was the only covariate associated with the increased risk of multiple skin tears; this model was also significant (Table 3).
Table 3.
Risk factors associated with skin tears by a multiple logistic regression (n = 1967)
| Risk factor | Skin tearsc | Multiple skin tearsd | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |||
| Malnutritiona | 1.61 | 1.11 | 2.34 | .011 | 2.48 | 1.37 | 4.50 | .003 |
| Age | 1.06 | 1.05 | 1.08 | <.001 | 1.06 | 1.03 | 1.08 | <.001 |
| Male | 1.47 | 1.05 | 2.07 | .025 | 2.41 | 1.38 | 4.21 | .002 |
| BMIb | 0.97 | 0.94 | 1.00 | .066 | 0.99 | 0.94 | 1.04 | .754 |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio.
Mild/moderately or severely malnourished.
Underweight.
The overall model was significant (χ 2(4): 133.79; P < .001).
The overall model was significant (χ 2(4): 59.03; P < .001).
3.2. Malnutrition, location, and classification of skin tear
No significant relationship between malnutrition and the location of skin tears was identified (Fisher's exact test: df = 4, P = .673); however, there was only a limited number of patients with skin tears on the head (n = 1), back/trunk (n = 3), and other (n = 2). There was no association between skin tear classification and malnutrition (χ 2 = 2.159, df = 4, P = .707).
4. DISCUSSION
This study found a significant relationship between malnutrition and skin tears, as well as malnutrition and multiple skin tears within a large metropolitan tertiary facility. BMI was not associated with a significantly increased risk of skin tears. Clinical guidelines state that the best way to manage skin tear prevalence is prevention; however, limited research has been conducted focusing on modifiable risk factors such as malnutrition and BMI.4, 40
Malnutrition was the variable most likely to increase the odds of skin tear development of those patients analysed. Identifying patients at risk of malnutrition early in admission and trained staff undertaking a comprehensive nutrition assessment, such as an SGA, is important to reduce patient harm and costs to the health care system.17, 41 Identification of modifiable risk factors for skin tears, such as malnutrition, is useful to highlight the need for the implementation of risk mitigation strategies (eg, manual handling precautions, dressing types), which may further contribute to improving patient care, preventing harm, and reducing health care costs. Nutrition is important for not only the prevention of skin tears but also its management, and nutrition should be optimised to heal any wounds, especially those that have developed into chronic wounds.42 Several studies state dietetic consultation as a beneficial strategy for skin tear prevention and management in order to promote and monitor adequate nutrition and hydration.8, 25, 28, 36, 43, 44 This study further supports the role of nutrition in the prevention and management of skin tears. Findings also highlight a significant reduction in the point prevalence of malnutrition over the 6‐year period; these findings are the subject of a separate manuscript for future publication.
The findings of this study reflect the work within pressure injuries with Banks et al,18 Ness et al,15 Iizaki et al,17 and Baumgarten et al19 who found ORs of 1.8 to 2.6 of developing a pressure injury in moderately malnourished patients up to 5 OR in the severely malnourished patient group. While the study showed malnourished patients to be more likely to develop multiple skin tears, malnutrition was not correlated with skin tear category.
This study found that BMI was not independently associated with skin tear development. It is common thinking that malnourished patients are low of body weight; however, this study clearly displays that a patient can be malnourished at any BMI category (Figure 1). A lower BMI is associated with a reduction in adipose tissue in various locations around the body, including the extremities. However, BMI is not a reliable indicator of adiposity in individuals as it does not take into account differentiations between populations, with factors such as fluid retention and muscle mass.45 Sanada et al26 found that a lower BMI (17 kg/m2compared to 17.6 kg/m2) correlated to skin tear incidence, but this was not the case for this cohort.
Although the goodness of fit was statistically significant when identifying the relationship between skin tears and malnutrition, it is presumed that pressure injuries and skin tears share similar characteristics in terms of skin integrity. However, these claims are yet to be substantiated with comprehensive evidence, and future research should focus on these knowledge gaps.40 Potential variables of interest include: history of skin tears, assistance with activities of daily living, impaired cognition, dry skin, bruised skin, medications and polypharmacy, inadequate nutritional intake, inability to feed oneself, poor appetite, dehydration, comorbidities, reason for admission, primary diagnosis, mobility, and Braden Score.1, 5, 12, 46
Advanced age is a well‐defined risk factor for skin tears and is an important consideration with Australia's aging population where the number of people aged over 65 years will rise to 18% in 2021 and 26% in 2051.39 Aging leads to structural skin changes, including reduced dermal thickness, elasticity, loss of underlying fat, resilience, and increased dryness increasing susceptibility to injury.22, 47, 48, 49 Due to these physiological changes, people aged 70 to 75 years are twice as likely to develop pressure injuries as those aged 55 to 69 years.50
The results of this study reflect a review article by Rayner et al12 that examined the location of skin tears, with upper extremities being the most frequent skin tear location. The only variation with this study was a smaller number of skin tears in the head (0.6% compared to 3‐4% in other studies) (Table 1). There was no significant difference identified between nutritional status and location of skin tears; however, this lack of significance may be subject to type 2 error due to small numbers in specific categories (head, back/trunk, other). The results also displayed no significant relationship between nutritional status and skin tear classification. This may be due to the skin tear classification system not directly denoting severity as it does with pressure injuries but rather being a measure of skin loss.17, 18
This study has multiple strengths, particularly a complete regression analysis dataset approaching 2000 patients across an entire tertiary hospital population demographic. All diagnoses and classifications for malnutrition and skin tears were standardised and validated and were only conducted by trained health professionals at the large metropolitan teaching hospital. Minimal data (8.8%) were missing data, displaying the rigorous data collection techniques on audit dates. However, limitations of this study include the inability to adjust for reason for admission, primary diagnosis, or comorbidities as these may also substantially impact skin tear point prevalence. Ideally, a Charlson comorbidity index would have been used to adjust for these factors; however, these data were unavailable for the study. Further work is being undertaken by the authors to consider the impact of additional variables of interest, such as specific pharmaceutical products and/or polypharmacy in general, on skin tears. The cross‐sectional point prevalence methodology precluded the identification of incident data for both malnutrition and skin tears and also the identification of causality as whether malnutrition was prevalent prior to skin tear was not able to be determined.
5. CONCLUSION
This sizeable study provides evidence that malnutrition and skin tears are independently associated after adjusting for age and BMI. Malnutrition was also independently associated with patients obtaining multiple skin tears. Findings highlight the importance of malnutrition identification and appropriate nutrition care practices as frontline measures to minimise the impact of skin tears on patients and the health care system more broadly.
Munro EL, Hickling DF, Williams DM, Bell JJ. Malnutrition is independently associated with skin tears in hospital inpatient setting—Findings of a 6‐year point prevalence audit. Int Wound J. 2018;15:527–533. 10.1111/iwj.12893
REFERENCES
- 1. Strazzieri‐Pulido KC, Peres GRP, Campanili TCGF, Santos VLCG. Skin tear prevalence and associated factors: a systematic review. J Sch Nurs. 2015;49(4):668‐674. [DOI] [PubMed] [Google Scholar]
- 2. Fleck CA. Preventing and treating skin tears. Adv Skin Wound Care. 2007;20(6):315‐320. [DOI] [PubMed] [Google Scholar]
- 3. Leblanc K, Baranoski S, Holloway S, Langemo D, Regan M. A descriptive cross‐sectional international study to explore current practices in the assessment, prevention and treatment of skin tears. Int Wound J. 2014;11(4):424‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leblanc K, Baranoski S, Christensen D, et al. The art of dressing selection: a concensus statement on skin tears and best practice. Adv Skin Wound Care. 2016;29(1):32‐46. [DOI] [PubMed] [Google Scholar]
- 5. McGough‐Csarny J, Kopac CA. Skin tears in institutionalized elderly: an epidemiological study. Ostomy Wound Manage. 1998;44(3 A suppl):14S‐24S. discussion 5S. [PubMed] [Google Scholar]
- 6. Chima CS, Barco K, Dewitt ML, Maeda M, Teran JC, Mullen KD. Relationship of nutritional status to length of stay, hospital costs, and discharge status of patients hospitalized in the medicine service. J Am Diet Assoc. 1997;97(9):975‐978. [DOI] [PubMed] [Google Scholar]
- 7. Stephen‐Haynes J, Carville K. Skin tears made easy. Wounds Int. 2011;2(4):1‐6. [Google Scholar]
- 8. LeBlanc K, Baranoski S. Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care. 2011;24(9):2‐15. [DOI] [PubMed] [Google Scholar]
- 9. Payne RL, Martin ML. The epidemiology and management of skin tears in older adults. Ostomy Wound Manage. 1990;26:26‐37. [PubMed] [Google Scholar]
- 10. Malone ML, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalized elderly. J Am Geriatr Soc. 1991;39(6):591‐595. [DOI] [PubMed] [Google Scholar]
- 11. Xu X, Lau K, Taira BR, Singer AJ. The current management of skin tears. Am J Emerg Med. 2009;27(6):729‐733. [DOI] [PubMed] [Google Scholar]
- 12. Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care. 2015;24(9):406‐414. [DOI] [PubMed] [Google Scholar]
- 13. Ferguson M, Capra S, Bauer J. Coding for malnutrition enhances reimbursement under casemix‐based funding. Aust J Nutr Diet. 1997;54(3):102. [Google Scholar]
- 14. Banks M, Ash S, Bauer J, Gaskill D. Prevalence of malnutrition in adults in Queensland public hospitals and residential aged care facilities. Nutr Diet. 2007;64(3):172‐178. [Google Scholar]
- 15. Ness SJ, Hickling DF, Bell JJ, Collins PF. The pressures of obesity: the relationship between obesity, malnutrition and pressure injuries in hospital inpatients. Clin Nutr. 2017; pii: S0261‐5614(17)30297‐2. 10.1016/j.clnu.2017.08.014. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16. Edington J, Boorman J, Durrant ER, et al. Prevalence of malnutrition on admission to four hospitals in England. Clin Nutr. 2000;19(3):191‐195. [DOI] [PubMed] [Google Scholar]
- 17. Iizaka S, O'kuwa M, Junko S, Sanada H. The impact of malnutrition and nutrition‐related factors on the development and severity of pressure ulcers in older patients receiving home care. Clin Nutr. 2010;29:47‐53. [DOI] [PubMed] [Google Scholar]
- 18. Banks M, Bauer J, Graves N, Ash S. Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Nutrition. 2010;26(9):896‐901. [DOI] [PubMed] [Google Scholar]
- 19. Baumgarten M, Margolis D, Berlin JA, et al. Risk factors for pressure ulcers among elderly hip fracture patients. Wound Repair Regen. 2003;11(2):96‐103. [DOI] [PubMed] [Google Scholar]
- 20. Watterson C, Fraser A, Banks M, et al. Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care. Nutr Diet. 2009;66:S1‐S34. [Google Scholar]
- 21. Leblanc K, Baranoski S. Skin tears: the forgotten wound. Nurs Manage. 2014;45(12):36‐46. [DOI] [PubMed] [Google Scholar]
- 22. Sjerobabski‐Mansnec I, Situm M. Skin Aging. Acta Clin Croat. 2010;49(4):515‐518. [PubMed] [Google Scholar]
- 23. Rayner R, Carville K, Leslie G, Dhaliwal SS. Measurement of morphological and physiological skin properties in aged care residents: a test‐retest reliability pilot study. Int Wound J. 2016;14:420‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Koyano Y, Nakagami G, Iizaka S, et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long‐term medical facility in Japan. Int Wound J. 2016;13(2):189‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. White MW, Karam S, Cowell B. Skin tears in frail elders: a practical approach to prevention. Geriatr Nurs. 1994;15(2):95‐99. [DOI] [PubMed] [Google Scholar]
- 26. Sanada H, Nakagami G, Koyano Y, Iizaka S, Sugama J. Incidence of skin tears in the extremities among elderly patients at a long‐term medical facility in Japan: a prospective cohort study. Geriatr Gerontol Int. 2015;15(8):1058‐1063. [DOI] [PubMed] [Google Scholar]
- 27. Leblanc K, Baranoski S, Christensen D, et al. International skin tear advisory panel: a tool kit to aid in the prevention, assessment, and treatment of skin tears using a simplified classification system. Clin Manag. 2013;26(10):459‐476. [DOI] [PubMed] [Google Scholar]
- 28. Brillhart B. Preventive skin care for older adults. Geriatr Aging. 2006;9(5):334‐339. [Google Scholar]
- 29. Reddy M. Skin and wound care‐ important considerations in the older adult. Adv Skin Wound Care. 2008;21(9):424‐436. [DOI] [PubMed] [Google Scholar]
- 30. Bell JJ, Bauer JD, Capra S, Pulle RC. Concurrent and predictive evaluation of malnutrition diagnostic measures in hip fracture inpatients: a diagnostic accuracy study. Eur J Clin Nutr. 2014;68(3):358‐362. [DOI] [PubMed] [Google Scholar]
- 31. Alberda C, Graf A, McCargar L. Malnutrition: etiology, consequences, and assessment of a patient at risk. Best Pract Res Clin Gastroenterol. 2006;20(3):419‐439. [DOI] [PubMed] [Google Scholar]
- 32. Kubrak C, Jensen L. Malnutrition in acute care patients: a narrative review. Int J Nurs Stud. 2007;44(6):1036‐1054. [DOI] [PubMed] [Google Scholar]
- 33. Sheean PM, Peterson SJ, Gurka DP, Braunschweig CA. Nutrition assessment: the reproducibility of subjective global assessment in patients requiring mechanical ventilation. Eur J Clin Nutr. 2010;64(11):1358‐1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? J Parenter Enter Nutr. 1987;11(1):8‐13. [DOI] [PubMed] [Google Scholar]
- 35. Baranoski S, Leblanc K, Gloeckner M. Preventing, assessing, and managing skin tears: a clinical review. Am J Nurs. 2016;116(11):24‐30. [DOI] [PubMed] [Google Scholar]
- 36. Leblanc K, Christensen D, Orsted H, Keast D. Best practice recommendations for the prevention and treatment of skin tears. Wound Care Canada. 2008;6(1):14‐31. [Google Scholar]
- 37. WHO . BMI Classifications. World Health Organisation; 2006. [Google Scholar]
- 38. Payne RL, Martin ML. Defining and classifying skin tears: need for a common language. Ostomy Wound Manage. 1993;39(5):16‐20. 2‐4, 6. [PubMed] [Google Scholar]
- 39. Carville K, Lewin G, Newall N, et al. STAR: a consensus for skin tear classification. Prim Inten. 2007;15(1):18‐21. [Google Scholar]
- 40. Leblanc K, Baranoski S. Skin tears: finally recognised. Adv Skin Wound Care. 2017;30(2):62‐63. [DOI] [PubMed] [Google Scholar]
- 41. Gallagher Allred CR, Coble Voss A, Finn SC, McCamish MA. Malnutrition and clinical outcomes: the case for medical nutrition therapy. J Am Diet Assoc. 1996;96(4):361‐369. [DOI] [PubMed] [Google Scholar]
- 42. Molnar JA, Underdown MJ, Clark WA. Nutrition and chronic wounds. Adv Wound Care. 2014;3(11):663‐681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Leblanc K, Baranoski S. Prevention and management of skin tears. Adv Skin Wound Care. 2009;22(7):325‐332. quiz 33‐34. [DOI] [PubMed] [Google Scholar]
- 44. LeBlanc K, Baranoski S. Skin tears: the forgotten wound. Nurs Manage. 2014;45(12):36‐46. quiz 46‐7. [DOI] [PubMed] [Google Scholar]
- 45. Nevill AM, Stewart AD, Olds T, Holder R. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol. 2006;129(1):151‐156. [DOI] [PubMed] [Google Scholar]
- 46. Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: a case‐control study. Int Wound J. 2015;13:1246‐1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Farage MA, Miller KW, Elsner P, Maibach HI. Structural characteristics of the aging skin: a review. Cutan Ocul Toxicol. 2007;26(4):343‐357. [DOI] [PubMed] [Google Scholar]
- 48. Hanson D, Langemo D, Anderson J, Thompson P, Hunter S. Friction and shear considerations in pressure ulcer development. Adv Skin Wound Care. 2010;23(1):21‐24. [DOI] [PubMed] [Google Scholar]
- 49. Koyano Y, Nakagami G, Iizaka S, Sugama J, Sanada H. Skin property can predict the development of skin tears among elderly patients: a prospective cohort study. Int Wound J. 2016;14(4):691‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Farage MA, Miller KW, Berardesca E, Maibach HI. Clinical implications of aging skin: cutaneous disorders in the elderly. Am J Clin Dermatol. 2009;10(2):73‐86. [DOI] [PubMed] [Google Scholar]


