Abstract
The objectives of this study were to provide an assessment of photographic documentation of the wound from the patients' perspective and to evaluate whether this could improve patients' understanding of and involvement in their wound care. Our results revealed that most patients visiting the wound care clinic have difficult‐to‐see wounds (86%). Only 20% of patients monitor their wounds and instead rely on clinic or nurse visits to track the healing progress. There was a significant association between patients' ability to see their wound and their subsequent memory of the wound's appearance. This was especially true for patients who had recently begun visiting the wound care clinic. This relationship was not present in patients who had visited the clinic for 3 or more years. Patients reported that the inability to see their wounds resulted in feeling a loss of autonomy. The majority of patients reported that photographing their wounds would help them to track the wound progress (81%) and would afford them more involvement in their own care (58%). This study provides a current representation of wound photography from the patients' perspective and reveals that it can motivate patients to become more involved in the management of their wounds – particularly for patients with difficult‐to‐see wounds.
Keywords: Patient perception, Photography, Wound
Introduction
Previous research has established that wound photography can be useful for clinicians and teams of caregivers given the ease of visually comparing wound healing over time, their value and accuracy for calculating wound areas 1, 2, and their effectiveness as tools for interdisciplinary communication between members of the wound care team 3. However, no research has currently been performed on the perceived benefits of wound photography from the patients' perspective. Patients are notably key stakeholders in wound management and are uniquely positioned to provide feedback that is important for wound care improvement.
Langemo et al. suggested that for patients with wounds in areas that are difficult to see (such as on the feet or on the sacrum), seeing their wounds can be educational and may help motivate adherence to treatment protocols 4. However, a literature search for available evidence on patients' perspective of wound photography yielded no results. High‐resolution cellular phone and tablet cameras are becoming ubiquitous, and with the availability of this technology 5 the use of clinical photography in wound management is expected to increase 6, 7, 8, 9, 10; it would therefore be beneficial to understand how patients feel about being involved in wound monitoring using photography.
This study sought to understand the importance and perceived benefits of wound photography from the patient's viewpoint. Specifically, we were interested in evaluating if (and how) patients monitored their wounds and whether we can use photography to foster patient participation in their own wound care.
Methods
The questionnaire covered issues relating the accessibility and chronicity of patients' wounds. Briefly, patients were asked if their wound was difficult to see, if they monitored their wound and if they thought taking photographs of their wound would be beneficial. Specifically, patients were asked whether photographs would help them to monitor recovery and perhaps motivate them to become actively involved in their wound care.
The questionnaire was pilot‐tested among medical students and staff, and then distributed to patients who regularly visited the Wound Care Centre at Women's College Hospital (Toronto, Canada). All patients visiting the clinic on the days of study were offered the chance to participate. No exclusion or inclusion criteria were applied. All patients gave written consent prior to participation in the study. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected by the ethics approval obtained from the Research Ethics Board at the Women's College Hospital.
The questions were arranged in a 6‐point Likert scale format from ‘strongly disagree’ to ‘strongly agree’ with ‘I do not know’ being the midpoint. The survey was completed on a voluntary basis and the questionnaire contained no data that could lead to identification.
The data were tabulated and analysed using chi‐square frequency tests in R language 11.
Results
We interviewed a total of 71 patients whose term at the wound care clinic ranged from 1 month to 20 years with a mean of 3·3 years (SD 4·3 years). On average, patients visited the wound care clinic every 1·4 months (SD 1·6 months) and 38% of patients had been visiting the wound care clinic for at least 3 years. The majority of wounds were located on the lower extremities with 62% [95% confidence interval (CI): 50–72%] on the foot and 24% (95% CI: 16–35%) on the leg (Figure 1), which may account for the reported problems that most patients had seeing their wounds (61%; 95% CI: 49–71%). However, surprisingly, 64% (95% CI: 59–74%) of patients also reported that they remember how their wounds appeared at their last clinical visit.
Figure 1.
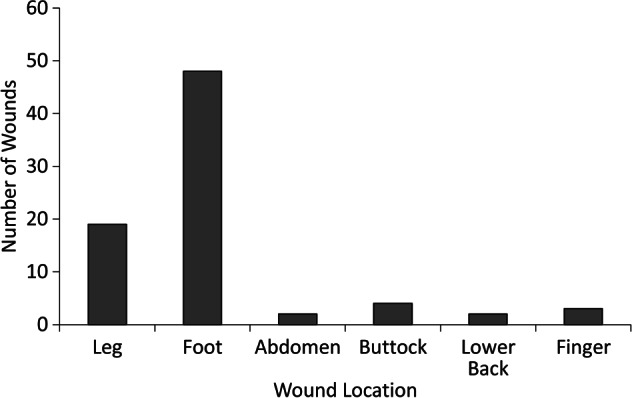
Distribution of locations of patients' wounds.
Only 20% (95% CI: 14–29%) of patients monitor their wounds' progress on their own, and the remaining 80% of patients rely on either nurse visits (40%) or clinical visits (40%) to track their wounds.
The majority of patients (48%; 95% CI: 35–58%) reported that seeing their wounds decrease in size is the most important indicator of wound healing. Interestingly, patients attributed the highest importance for monitoring their wounds to a visual indicator.
Given these results, we wished to examine this question more rigorously by testing whether patients' ability to see their wound was related to subsequent memory.
We split the data by patients' self‐reported ability to see their wound, and tested their reported memory of the wound. The analyses were conducted in R using chi‐square tests. Frequencies are reported in Table 1.
Table 1.
Frequency tables based on patients' reported ability to see their wound
| Patient reported seeing wound | Patient reported not seeing wound | |
|---|---|---|
| Memory for wound | ||
| Remember | 20 | 21 |
| Do not remember | 6 | 24 |
| Photographs useful for tracking healing | ||
| Agree | 21 | 36 |
| Disagree | 5 | 8 |
| Photographs promote more active participation in wound care by | ||
| patients? | ||
| Agree/strongly agree | 13 | 26 |
| Disagree/strongly disagree | 3 | 7 |
| Neutral/do not know | 7 | 12 |
Memory of wounds if patients reported being able to see them
A chi‐square analysis was run on the 2 (memory of wound) × 2 (visual access to wound) tabulated data (see Figure 2 for proportions). There was a significant association between patients being easily able to see their wound and whether they reported subsequent memory of how the wound appeared (χ 2 = 6·18, P < 0·01). On the basis of the odds ratio, the odds of remembering a wound were 3·73 times higher if they had reported previously seeing it. There was no reported difference in memory for participants who did not have visual access to their wounds.
Figure 2.
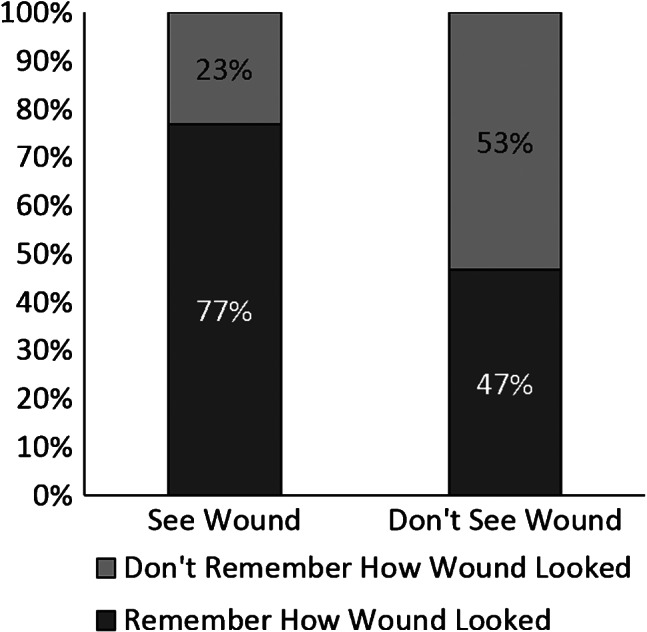
Reported memory for wounds based on visual access.
We were interested to see whether chronicity might interact with the visibility of wounds and memory, that is, whether patients who had been visiting the clinic for longer than 3 years might react differently from those under that margin. We plotted wound memory and ease of visibility as a function of time (Figure 3). Patients' memories of their wounds appear to be highest within the first few years of wound care. To test the significance of this trend, we refined our sample to those patients who spent less than 3 years in the clinic (versus those that spent more), and performed the chi‐square analysis again on these subsets. The result was considered statistically significant (χ 2 = 11·9, P < 0·001). On the basis of the odds ratio, this implies that the odds of remembering a wound were ∼13·6 times higher if patients had reported previously seeing it. There was no significant relationship between wound visibility and memory for the wound in patients who had been visiting the clinic for more than 3 years. Thus, it appears that the results of the initial analysis may be driven by patients with more recently developed wounds (i.e. less than 3 years) that are visible, and which patients tend to remember more. Long‐term wound care may reflect apathy or disinterest as a result of slow progress.
Figure 3.
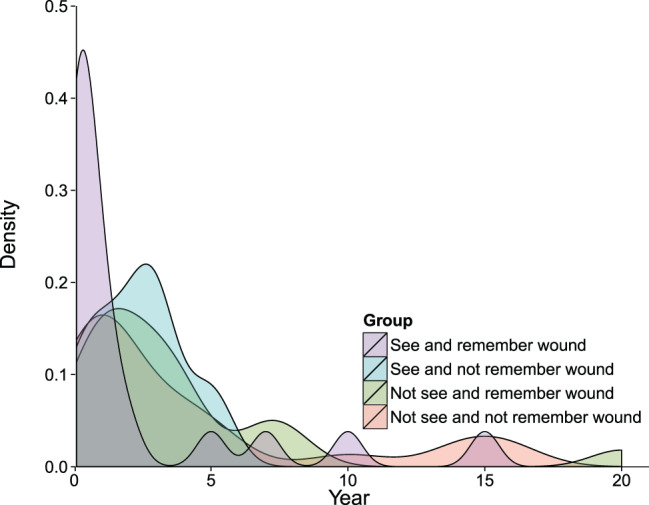
Density plot of memory for wound by visibility across time.
Whether photographs would help track healing
Given the importance for patients to visually assess their own wounds, we split the data by the ease with which patients reported being able to see their wounds and tested whether they thought photographs would help track healing and promote more active participation in wound care.
Interestingly, patients were equally likely to endorse using photographs to track healing regardless of whether their wounds were easy to see or not (χ 2 = 0·012, P = 0·91; Figure 4). This did not differ as a function of time spent in the clinic (all P's > 0·08).
Figure 4.
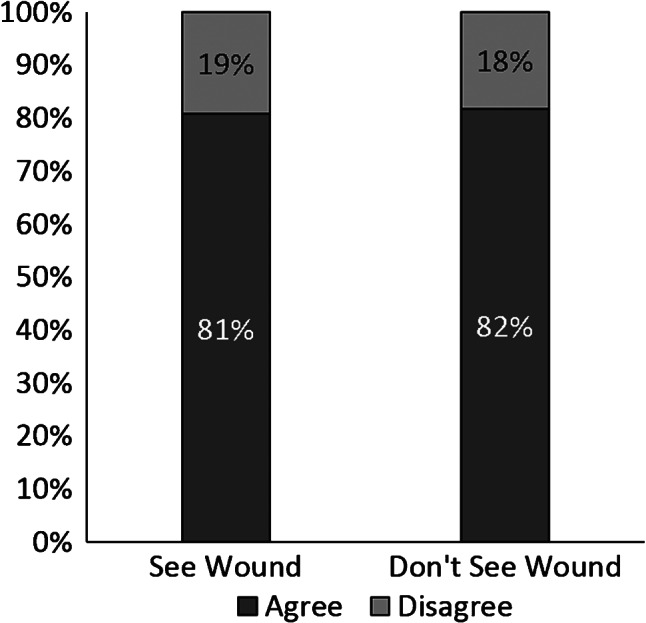
Patients' endorsement of photographs to help track healing.
Whether photographs would promote active participation in care
We next tested whether patients' visual access to their wounds would make a difference to their endorsement of the idea that photographs might promote active participation. More than half of our patients agreed that access to photographs would promote greater participation in self‐care (Figure 5). These rates did not differ by whether participants could easily see their wound or not [χ 2 (2) = 1·2, P = 0·54], suggesting that both groups thought that photographs would be a useful tool for tracking their wounds. These rates also did not differ by chronicity (i.e. patients who had been to the clinic for 3 or less years were equally likely to endorse using photographs to promote active patient care as those who had been coming to the clinic for longer periods).
Figure 5.
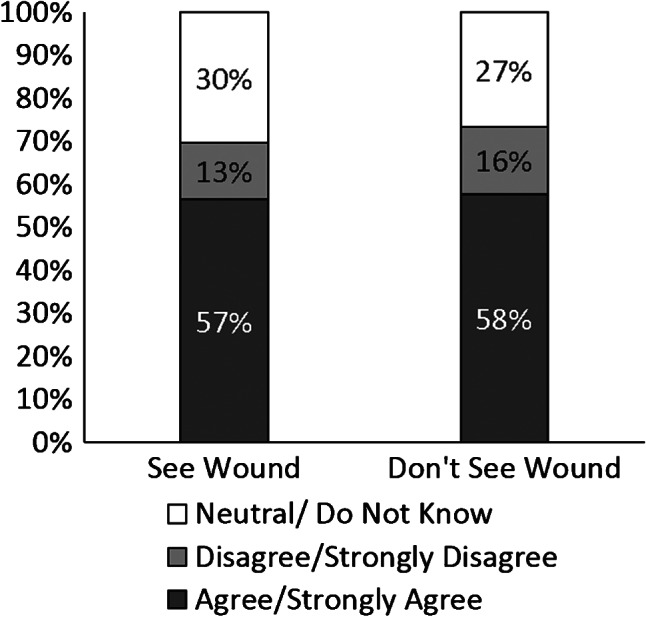
Participants' endorsement of the idea that photographs would promote active participation in care.
Patient perspectives of wound photography
In the open comments section, patients reported feeling ‘fear and a loss of independence and control’ because they could not see easily their wounds due to visual impairment, lack of flexibility or because their wounds were located on difficult‐to‐see areas such as the foot or behind the leg. Patients further reported that being able to see their wounds better would afford them ‘peace of mind’ and the ability to associate the severity of their pain with the appearance of the wound. They also reported that photographs provide ‘objective descriptions’ of their wounds allowing them to observe how their wound is healing as opposed to relying solely on the physician's assessments. One patient noted that looking at her actual wound was ‘too disturbing’ and that she preferred to look at a photograph to assess visually the condition of her wound. Finally, several patients also noted that it would help them coordinate their own care between different health care specialists if a wound photograph was included in every report.
Not all patients believed that taking photographs would be beneficial. Approximately 18–19% (95% CI: 11–30%) of patients reported that they did not accept that taking a photograph is useful for tracking the healing process of their wound (Figure 4) and 13–16% (95% CI: 5–20%) of them disagreed that taking photographs of their wounds would help them to be more actively involved in their own care (Figure 5). These patients reported that the location of the wound and their decreased range of motion and/or visual acuity prevented them from becoming more involved in their own care regardless of whether photographs were taken. Some patients also reported that they already used mirrors to visualise difficult‐to‐see wounds and factors such as depth of the wound cannot be captured in a photograph.
Discussion
This study provides insight into the chronicity and accessibility of wounds, and specifically evaluates patients' perceptions of wound photography. Up to 38% of patients who participated in this study had chronic wounds (greater than 3 years) and visit the wound care clinic frequently. The majority of patients base their assessment of wound healing on visual indicators. A finding of concern in this study was that many patients have difficulty seeing their wounds and therefore, not surprisingly, few patients monitor their wounds themselves. A concerted effort is needed to provide patients who are not able to see their wounds with tools to help them become more involved in their own wound care. Of particular interest, patients who are able to see their wounds are approximately four times more likely to remember how their wounds appeared previously and therefore monitor the progress of wound healing. However, patients' ability to recall how their wounds appeared in a previous clinical visit declined drastically with wound chronicity. The finding that the odds of remembering a wound were 14 times higher if patients had reported previously seeing it easily, and they had been visiting the wound care clinic for less than 3 years is intriguing, especially given that there was no significant relationship between wound visibility and memory of the wound in patients who had been visiting the clinic for more than 3 years. These results suggest additional patient education, potentially through photographic documentation of the wounds, may be particularly beneficial during the early period of clinical visits. Furthermore, these results also raise the important issue of lack of motivation and apathy prevalent in long‐term patients.
The majority of patients report that taking photographs of their wounds would help them to track their wound progression and allow them to be more involved in their own wound care (81–82% and 57–58%, respectively), regardless of whether they have difficult‐to‐see wounds. These results demonstrate that wound photography can be a powerful tool in facilitating patient education and management of their wounds.
It is interesting to note that although 82% of patients reported that wound photography would be helpful for tracking wound progress, significantly fewer patients believed that photographs would help them to be more involved in their own care (57%). As noted previously, patients reported a variety of factors such as the location of the wound, limited visual acuity and reduced range of motion that minimised their ability to manage their wounds at home. If the question had been reworded to ask if wound photography would help patients and their families to be more actively involved in their wound care, patients may have responded more positively.
A small proportion of patients (19%) did not believe that taking photographs of their wounds would be useful for tracking wound healing because they either already used mirrors to visualise difficult‐to‐see wounds, or because photographs cannot adequately show them factors such as depth of the wound. It is important to clarify to patients that photographs of wounds are a useful adjunct to the written documentation but they would not replace a standard wound evaluation, which includes observations of depth, warmth and odour. Furthermore, patients' use of mirrors reveals a clear interest among them to be involved in their own care, which should be fostered by the health care team. For example, many patients suggested that photographs of their wounds could improve coordination and continuity of their care among different health care providers. Wound photography could also be easily incorporated into the electronic medical record system and may enhance communication between all members of the wound care team.
This study has a number of limitations. First, questions about the perceived utility of wound photography may have been leading. However, the open comments section afforded patients the opportunity to provide an unlimited range of qualitative answers and insight into components that are important for their satisfaction. Second, a larger study sample (greater than n = 71) would be useful to confirm these results and to provide more information about long‐term wound patients who formed a minority in this study. We hope that this study will set a precedent for further appraisal of patients' perspectives on wound care in other clinics.
Finally, this study provides a broad characterisation of patient satisfaction and perception of wound care, and the relationship between wound chronicity, accessibility and the utility of wound photography. Although our findings help identify target populations for whom we can improve care, for example, patients who have difficult‐to‐see chronic wounds, it is important to recognise that many other factors are pertinent to patient‐centred wound care and that there is significant value in evaluating patient perceptions when considering a new intervention, such as wound photography.
Ideally, follow‐up and evaluation of the impact of wound photography on patient/family education, adherence to plan of care, motivation to be more involved in the patient's wound care and ultimately the resulting healing progress are necessary to confirm the intended outcomes.
This work is attributed to the Wound Care Centre at Women's College Hospital and the University of Toronto.
References
- 1. Rajbhandari SM, Harris ND, Sutton M, Lockett C, Eaton S, Gadour M, Tesfaye S, Ward JD. Digital imaging: an accurate and easy method of measuring foot ulcers. Diabet Med 1999;16:339–42. [DOI] [PubMed] [Google Scholar]
- 2. Samad A, Hayes S, French L, Dodds S. Digital imaging versus conventional contact tracing for the objective measurement of venous leg ulcers. J Wound Care 2002;11:137–40. [DOI] [PubMed] [Google Scholar]
- 3. Fischetti LF, Paguio EC, Alt‐White AC. Digitized images of wounds: a nursing practice innovation. Nurs Clin North Am 2000;35:541–50. [PubMed] [Google Scholar]
- 4. Langemo D, Hanson D, Anderson J, Thompson P, Hunter S. Digital wound photography: points to practice. Adv Skin Wound Care 2006;19:386–7. [DOI] [PubMed] [Google Scholar]
- 5. Alder ME, Deahl ST, Matteson SR. Clinical usefulness of two‐dimensional reformatted and three‐ dimensionally rendered computerized tomographic images: literature review and a survey of surgeons' opinions. J Oral Maxillofac Surg 1995;53:375–86. [DOI] [PubMed] [Google Scholar]
- 6. Ahn C, Salcido RS. Advances in wound photography and assessment methods. Adv Skin Wound Care 2008;21:85–93 (quiz 4–5). [DOI] [PubMed] [Google Scholar]
- 7. Kanthraj GR, Braun RP. The integration of the internet, mobile phones, digital photography, and computer‐aided design software to achieve telemedical wound measurement and care [9] (multiple letters). Arch Dermatol 2005;141:1470–2. [DOI] [PubMed] [Google Scholar]
- 8. Sprigle S, Nemeth M, Gajjala A. Iterative design and testing of a hand‐held, non‐contact wound measurement device. J Tissue Viability 2012;21:17–26. [DOI] [PubMed] [Google Scholar]
- 9. Tsai HH, Pong YP, Liang CC, Lin PY, Hsieh CH. Teleconsultation by using the mobile camera phone for remote management of the extremity wound: a pilot study. Ann Plast Surg 2004;53:584–7. [DOI] [PubMed] [Google Scholar]
- 10. Van LB, Sicotte KM, Lassiter RR, Jablonski KA, Crean DA, Jeng JC, Jordan MH. Digital photography: enhancing communication between burn therapists and nurses. J Burn Care Rehabil 2004;25:54–60. [DOI] [PubMed] [Google Scholar]
- 11. Team RC . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2013. [Google Scholar]


