Abstract
In this study, we analyzed sarcopenia prevalence and the cut-off points for skeletal muscle mass index (SMI), gait speed, and handgrip strength in young (18-39 years), middle-aged (40-59 years), and elderly (>60 years) individuals (n=1685) from Zhejiang Province in China. The prevalence of sarcopenia among individuals above 65 years was 2.21%, 4.87%, 5.31%, 14.16%, and 16.37% according to five diagnostic criteria (AWGS2019, AWGS2014, EWGSOP1, EWGSOP2, and local standard). The mean SMI (Kg/m2) was 7.961±0.7966, 7.801±0.7276, and 7.544±0.7493, respectively, in young, middle-aged, and elderly males. The mean SMI in young, middle-aged, and elderly females was 6.1570±0.5658, 6.604±0.5658, and 6.248±0.7483, respectively. SMI correlated negatively with age (r=-0.2344, P<0.001), but was not associated with age in females (r=0.0573, P=0.1463). The cut-off point of SMI for sarcopenia was ≤6.3678 kg/m2 in males and ≤5.0254 kg/m2 in females. These findings shows that the prevalence of sarcopenia increased gradually with age and varied significantly based on the diagnostic criteria used for this analysis. The mean SMI of young women was lower than in middle-aged women, making them an unsuitable reference population for determining cut-off values for sarcopenia diagnosis.
Keywords: sarcopenia, skeletal muscle index, prevalence, cut-off point, body composition
INTRODUCTION
Sarcopenia is an age-related syndrome that is characterized by progressive loss of muscle mass, strength and function that reduces quality of life and is accompanied by physical disability [1]. It was officially recognized in 2016 as a specific disease and assigned the diagnosis and staging code, ICD-10-CM (M62.84) [2, 3] The prevalence of sarcopenia is 5-13% among individuals aged 60-70 years [4, 5] and 11-50% among individuals aged above 80 years [6, 7].
Muscle mass varies among people of different racial origin [8], and is influenced by genes [9], hormones [10], and lifestyle [11]. Sarcopenia is defined as by reduction in skeletal muscle mass that is two standard deviations below the average muscle mass of young adults as the reference population [1, 7, 12–14]. As a result, diagnosis and prevalence results of sarcopenia vary significantly between populations because the cut-off values are different. Despite similar socioeconomic backgrounds, there is great variation in body composition as well as muscle mass, strength and performance between individuals of different races [15]. Hence, the cut-off values for the diagnosis of sarcopenia based on muscle mass, strength, and function need to be determined based on ethnicity [16]. Currently, the cut-off points for the diagnosis of sarcopenia are arbitrary due to differences in measurement techniques and reference populations. The European Working Group on Sarcopenia in older people (EWGSOP2) [17] and the Asian Working Group on Sarcopenia (AWGS) in 2014 [12] and 2019 [18] proposed key criteria for the diagnosis of sarcopenia in order to compare results of studies involving individuals from different ethnic backgrounds.
EWGSOP2 used muscle strength as the main parameter for diagnosing sarcopenia, but, evaluation of muscle loss varies considerably based on the instruments and methods that are used [15] Currently, the cut-off points for the diagnostic parameters of sarcopenia are arbitrary because of differences in measurement techniques and reference populations. In China, the parameters proposed by AWGS in 2014 have been used for sarcopenia studies [19, 20]. The prevalence of sarcopenia in older adults is 17% in China compared to 6% in Hong Kong and Taiwan [21].
The cut-off points for determining loss of muscle mass varies significantly in studies conducted in different Chinese populations [5, 22, 23]. Moreover, most of the data regarding sarcopenia is obtained from the elderly individuals and groups, and very few studies have monitored the prevalence of sarcopenia in younger Chinese populations. In particular, the data for muscle mass is not available for young adults. Sarcopenia is common among older adults but can also occur in younger and middle aged individuals. Hence, development of validated cut-off points based on normative data and their predictive value is of high priority [17]. This requires analysis of the relevant diagnostic parameters of sarcopenia in different age groups.
In this study, we evaluated the cut-off point for the skeletal muscle index to diagnose sarcopenia in 1685 Chinese individuals belonging to different age groups from the Zhejiang Province. We also compared the differences in sarcopenia prevalence among males and females belonging to different age groups based on five different diagnostic criteria.
RESULTS
The prevalence of sarcopenia based on the five diagnostic criteria ranged from 2.61%-9.72% for individuals aged above 60 years, 4.87%-16.37% for individuals aged above 65 years, and 18.52%-55.56% for individuals aged above 80 years old. Overall, sarcopenia prevalence increased significantly with age (P<0.001, Table 1). Moreover, the prevalence of sarcopenia among females in different age groups evaluated according to the EWGSOP2 parameters was statistically similar (P=0.345, Table 1).
Table 1. Prevalence of sarcopenia in males and females belonging to different age groups according to the 5 diagnostic criteria.
| Gender | Diagnostic criteria | Age group (% sarcopenia positive) | Chi-square | P value | ||||
| 18-39y | 40-59y | ≥60y | ≥65y | ≥80y | ||||
| Male | AWGS2019 | 0.32 (1/311) | 1.85 (10/541) | 6.67 (16/240) | 12.9 16/124) | 53.85 (7/13) | 71.134 | <0.001 |
| AWGS2014 | 0.32 (1/311) | 0.37 (2/541) | 5.83 (14/240) | 10.48 (13/124) | 38.46 (5/13) | 74.491 | <0.001 | |
| EWGSOP 1 | 0.32 (1/311) | 0.37 (2/541) | 2.92 (7/240) | 5.65 (7/124) | 23.08 (3/13) | 74.491 | <0.001 | |
| EWGSOP2 | 0.32 (1/311) | 0 (0/541) | 1.67 (4/240) | 3.23 (4/124) | 15.38 (2/13) | 25.436 | <0.001 | |
| Local standard | 0.32 (1/311) | 0 (0/541) | 2.5 (6/240) | 4.84 (6/124) | 15.38 (2/13) | 32.869 | <0.001 | |
| Female | AWGS2019 | 0.43 (1/230) | 1.1 (2/181) | 13.74 (25/182) | 20.59 (21/102) | 57.14 (8/14) | 77.934 | <0.001 |
| AWGS2014 | 0.43 (1/230) | 1.1(2/181) | 3.85 (7/182) | 18.63 (9/102) | 57.14 (8/14) | 91.299 | <0.001 | |
| EWGSOP 1 | 0 (0/230) | 0 (0/181) | 2.75 (5/182) | 4.9 (5/102) | 21.43 (3/14) | 91.299 | <0.001 | |
| EWGSOP2 | 0 (0/230) | 0 (0/181) | 0.55 (1/182) | 0.98 (1/102) | 0 (0/14) | 4.81 | 0.345 | |
| Local standard | 0 (0/230) | 0 (0/181) | 2.75 (5/182) | 4.9 (5/102) | 21.43 (3/14) | 26.888 | <0.001 | |
| Total | AWGS2019 | 0.37(2/541) | 1.66 (12/722) | 9.72 (41/422) | 16.37 (37/226) | 55.56 (15/27) | 150.268 | <0.001 |
| AWGS2014 | 0.37(2/541) | 0.55 (4/722) | 4.98 (21/422) | 14.16 (32/226) | 48.15 13/27) | 171.028 | <0.001 | |
| EWGSOP 1 | 0.18 (1/541) | 0.28 (2/722) | 2.84 (12/422) | 5.31 (12/226) | 22.22 (6/27) | 171.028 | <0.001 | |
| EWGSOP2 | 0.18 (1/541) | 0(0/722) | 1.18 (5/422) | 2.21 (5/226) | 7.14 (2/27) | 24.568 | <0.001 | |
| Local standard | 0.18 (1/541) | 0(0/722) | 2.61 (11/422) | 4.87 (11/226) | 18.52 (5/27) | 60.644 | <0.001 | |
As shown in Table 1, the prevalence of sarcopenia as calculated by the five different diagnostic criteria varied widely. In both males and females, the highest percentage of sarcopenia prevalence was according to AWGS 2019 and the lowest percentage was according to EWGSOP2. The percentages of sarcopenia prevalence according to AWGS 2014, EWGSOP1, and local standard were in between the values obtained for AWGS 2019 and EWGSOP2. This demonstrated that the clinical evaluation of sarcopenia prevalence varied significantly based on the diagnostic criteria used for analysis.
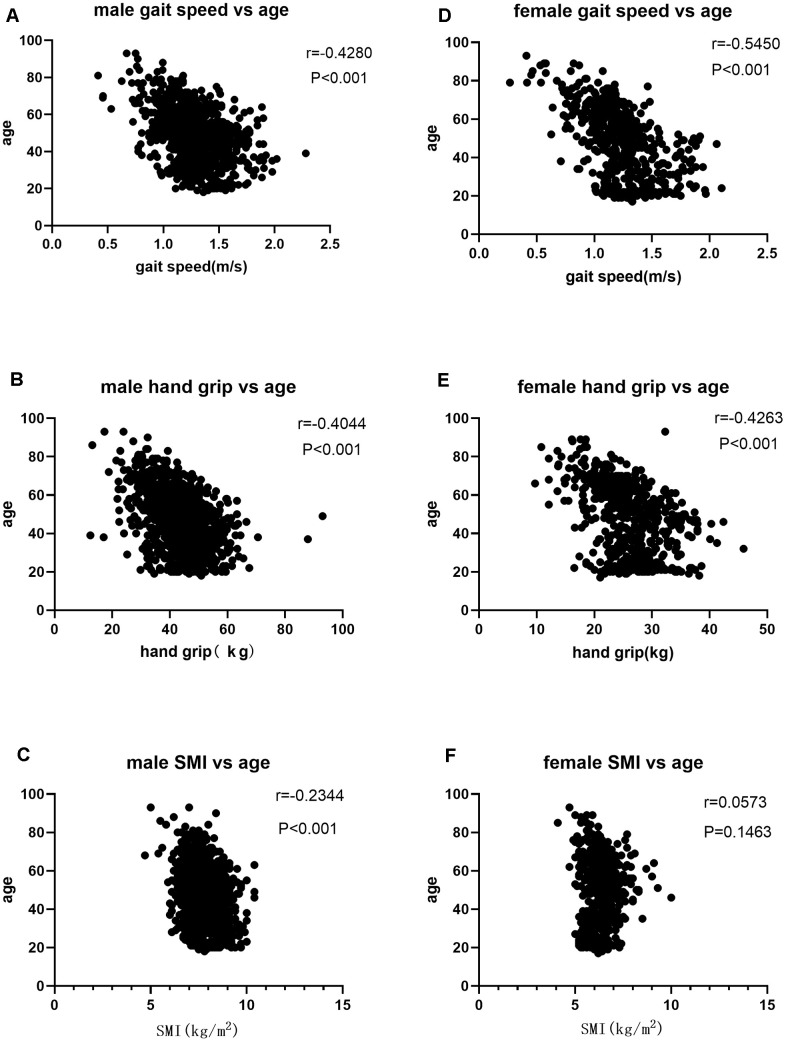
We then performed Pearson correlation analysis according to gender stratification to determine the relationship between age and sarcopenia parameters such as SMI, gait speed, and hand grip. In males, we observed a negative correlation between age and SMI (r=-0.2344), hand grip (r=-0.4044), and gait speed (r=-0.4280) (P<0.001; Table 2, Figure 1A–1C). In females, we did not observe any association between SMI and age (r=0.0573, P=0.1463, Table 2, Figure 1D–1F), but observed a negative correlation between age and hand grip (r=-0.4263) and gait speed (r=-0.5450) (P<0.001; Table 2, Figure 1D, 1E).
Table 2. Pearson correlation analysis between diagnostic indicators of sarcopenia and age in males and females.
| Gender | Parameters | r | P |
| Male | gait speed | -0.4280 | <0.001 |
| Hand grip | -0.4044 | <0.001 | |
| SMI | -0.2344 | <0.001 | |
| Female | gait speed | -0.5450 | <0.001 |
| Hand grip | -0.4263 | <0.001 | |
| SMI | 0.05973 | 0.146 |
Figure 1.
(A) Correlation analysis of gait speed and age in males; (B) Correlation analysis of hand grip and age n males; (C) Correlation analysis of SMI and age in males; (D) Correlation analysis of gait speed and age in females; (E) Correlation analysis of hand grip and age in females; (F) Correlation analysis of SMI and age in females.
As shown in Figure 2, the mean SMI values for men and women aged 18-39 years were 7.961 ± 0.7966 kg/m2 and 6.157 ± 0.5658 kg/m2, respectively. Therefore, the cut-off points for the abnormal SMI (two standard deviations below the mean SMI) in males and females aged 18-39 years were ≤ 6.3678 kg/m2 and ≤ 5.0254 kg/m2, respectively. These cut-off points were significantly lower than the recommended AWGS values for SMI, namely, ≤ 7.0 kg/m2 for males and ≤ 5.7 kg/m2 for females.
Figure 2.
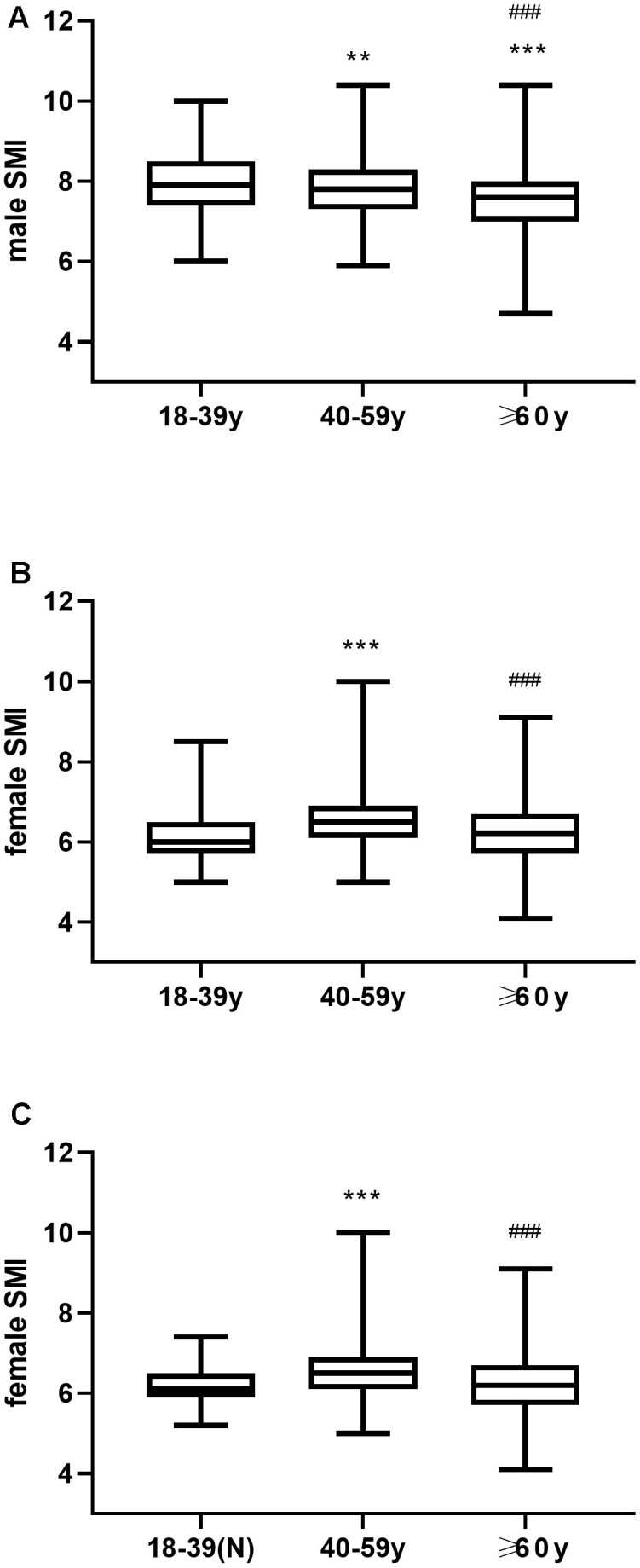
(A) Mean SMI in young, middle-aged and elderly men. (B) Mean SMI in young, middle-aged and elderly women. (C) Mean SMI in young women with normal BMI (18.5-23.9) as well as middle-aged and elderly women. ** P ≤0.01 vs 18-39y, *** P <0.001 vs 18-39y, ### P <0.001 vs 40-59y.
In males, the SMI values gradually decreased with age, and the pair-wise comparisons between young, middle-aged, and elderly age groups were statistically significant (P<0.001, Figure 2A). Moreover, young women and young women with normal BMI showed significantly lower SMIs than the middle-aged women (P < 0.001, Figure 2B, 2C), and lower but statistically similar SMI values than the elderly women (P=0.34 Figure 2, P>0.05, Figure 2B). Hence, young women were not suitable as a reference population for determining the cut-off point to diagnose sarcopenia.
As shown in Table 3, the mean SMI values for women aged 60-69 years were 6.386 ± 0.7492 kg/m2. The females aged 60-69 years showed significantly higher SMI values than the females aged 18-29 years (P=0.0031, Table 3), and SMI values were statistically similar, compared with the females aged 30-39, 40-49, 50-59, 18-39, 18-59 years (P>0.9999, P=0.9286, P>0.9999 P= 0.0689, P>0.9999, Table 3). The females aged>60 years showed significantly similar SMI values than the females aged 18-29, 18-39 years (P=0.4326, P> 0.9999, Table 3). The females aged 18-29 years showed significantly similar SMI values than the females aged 18-39 years (P=0.1911, Table 3).
Table 3. Comparison of SMI values among women in different age groups.
| Age | mean1 | mean2 | Summary | P value |
| 18-29y vs. 60-69y | 6.074 | 6.386 | ** | 0.0031 |
| 30-39y vs. 60-69y | 6.325 | 6.386 | ns | >0.9999 |
| 40-49y vs. 60-69y | 6.604 | 6.386 | ns | 0.9286 |
| 50-59y vs. 60-69y | 6.604 | 6.386 | ns | >0.9999 |
| 18-39y vs. 60-69y | 6.157 | 6.386 | ns | 0.0689 |
| 18-59y vs. 60-69y | 6.354 | 6.386 | ns | >0.9999 |
| 18-29y vs. ≥60y | 6.074 | 6.248 | ns | 0.4326 |
| 18-39y vs. ≥60y | 6.157 | 6.248 | ns | >0.9999 |
| 18-29y vs. 30-39y | 6.074 | 6.325 | ns | 0.1911 |
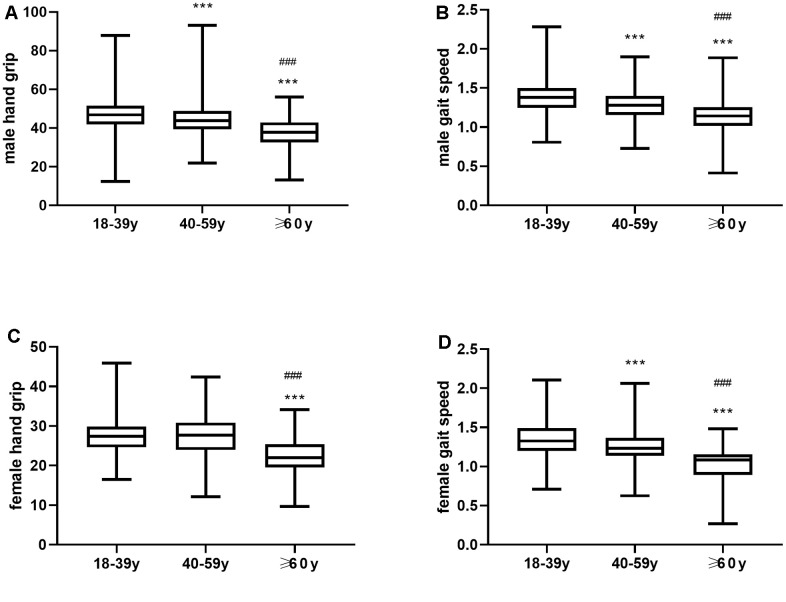
The handgrip strength of men gradually decreased with age, and the pair wise comparisons between young, middle-age and elderly age groups were statistically significant (P<0.001, Figure 3A). Moreover, the gait speed significantly decreased with age among both men and women (P<0.001, Figure 3B). In females, handgrip strength gradually decreased with age, but the differences were not statistically significant between young and middle-aged women (P>0.05, Figure 3C). The handgrip strength of both young and middle-aged women was significantly higher compared to the elderly women (P<0.001, Figure 3D).
Figure 3.
(A) Mean hand grip values and (B) Mean gait speed in young, middle-aged and elderly men. (C) Mean hand grip and (D) gait speed in young, middle-aged and elderly women. ** P ≤0.01 vs 18-39y, *** P <0.001 vs 18-39y, ### P <0.001 vs 40-59y.
DISCUSSION
Currently, there is no consensus regarding the diagnostic criteria for sarcopenia. Hence, sarcopenia diagnosis remains a matter of debate with the existence of multiple diagnostic criteria proposed by different medical expert groups. We analyzed 1685 individuals in three different age groups according to 5 diagnostic criteria for sarcopenia. The prevalence was 2.61%-9.72% among those aged over 60, 4.87%-16.37% among those aged over 65, and 18.52%-55.56% among those aged over 80. This demonstrates that the prevalence of sarcopenia increases significantly with age. Our data is consistent with previously reported research [4, 5, 7] and suggests an imbalance between muscle synthesis and degeneration [24, 25]. However, the wide-range of the cut-off points for different diagnostic parameters affects clinical determination of sarcopenia prevalence, especially among women. The cut-off points for the diagnostic parameters are determined based on the normative population data whenever available or from the predictive population data when normative data is not available. We observed that the muscle mass index of the young subjects in our study was lower than that of other Asian populations. These differences suggest that skeletal muscle mass depends on variables such as race, body shape, lifestyle, diet, and cultural background [26–28]. These differences may also be due to insufficient sample size in our study.
The variation in the muscle mass and strength in older individuals is related to the rate of muscle degeneration and the peak muscle mass and strength gained during the early years of life [29]. Muscle mass peaks around the age of 35 years [30]. After the age of 50 years, muscle mass and strength in the legs decrease every year by 1-2% and 1.5-5%, respectively [31]. In general, muscle mass reduces by about 30% and the cross-sectional muscle area shrinks by about 20% between 20 and 80 years of age [32].
Factors such as decreased nutrient intake, low physical activity, and chronic diseases increase the rate of sarcopenia progression [33]. We focused on the muscle mass of young individuals as a reference group to determine the cut-off points. In this study, we recruited healthy young women with a normal BMI and their skeletal muscle index was compared with that of the middle-aged and elderly women [34]. The middle-aged women in our study showed higher muscle mass than the younger women in our study, which was contradictory to previous findings that muscle mass reduces gradually with age. This may indicate that loss of muscle loss may occur during early periods of life in young women. It is also plausible that lifestyle and reduced physical activity may account for lower muscle mass in younger women compared to the middle aged women in our study. Larsson reported that the loss of the larger and faster contracting type II muscle fibers begins with adulthood [35]. The rate of muscle loss is significantly increased in individuals with immobility [36], including those who are immobilized at a young age. [37]. Evidence suggests that sarcopenia begins as early as the 4th decade of life [29, 30, 38]. Therefore, our study demonstrates that it is not suitable to use young subjects as references to determine the SMI (skeletal muscle mass index) cut-off points for sarcopenia.
In addition to the reducing synthesis of muscle protein, increased muscle protein breakdown affects muscle loss in the elderly over 70 [14]. So we chose women aged 60-69 as comparison, it can be seen from Table 3 that the SMI value of women aged 60-69 is higher than that of women aged 18-29 and others (18-39, 30-39, 40-49, 50-59), so 18-59 years old are not significant different statistically. In this study, the women aged 60-69 are more suitable than younger women as the reference population for the muscle mass of elderly women with sarcopenia.
This study has several limitations. Firstly, because of the limited number of samples, we fail to calculate sarcopenia prevalence based on more specfic stratification on gender-age. Secondly, this study was conducted in the coastal cities of the Zhejiang Province in China. Hence, the conclusions of this study may not apply to elderly populations in other regions of China and the world. Finally, there may be significant differences in nutrition and physical fitness of individuals belonging to different age groups, which may have influenced the results of our study. Moreover, generation differences may cause discrepancies among young and elderly individuals that have been selected by random sampling of the same population. Therefore, the cut-off point represented by two standard deviations below the average muscle mass of young adults may not be accurate.
In the future, the cut-off points for the diagnosis of sarcopenia need to be verified in the Chinese population, especially those regarding physical fitness and SMI values. Therefore, we recommend large-scale, multi-center studies in the rural, urban, and inland populations. Another plausible approach to resolve the discrepancies in the SMI values for diagnosing or evaluating sarcopenia in experimental studies is to determine a suitable reference range using the SMI values of healthy elderly individuals (For example, the cut-off points for the abnormal SMI of women is one standard deviations below the mean SMI values in females aged 60-69 years). Furthermore, BMI may not fully reflect the comparable physical status of elderly individuals when compared with middle-aged and younger individuals because of decreased height, reduced muscle mass, and increased fat content. Therefore, we recommend analyzing body composition annually for the elderly and compare changes in their muscle mass over time. Such an analysis can alert patients that are susceptible to sarcopenia when the rate of muscle loss exceeds the threshold range and preventive measures can be taken. We also suggest collecting body composition analysis data of the young and middle-aged individuals in addition to the elderly in order to develop large-scale data to support diagnosis of sarcopenia. In summary, our study shows that the prevalence of sarcopenia increases gradually with age. We also demonstrate that sarcopenia prevalence varies significantly between the five diagnostic criteria used in this study. Moreover, the mean SMI values of young women was lower than the middle-aged women’in this study and was not suitable as a reference population in determining cut-off values for the diagnostic parameters in evaluating sarcopenia.
MATERIALS AND METHODS
Inclusion and exclusion criteria of study subjects
This observational study included 1685 volunteers aged 18 and above from two communities in the coastal cities of Zhejiang Province, China between September 2018 and June 2019. This included 422 volunteers over 60 from the elderly health monitoring cohort, which has enrolled 20,000 people from 11 cities in the Zhejiang Province and has been followed-up since 2014. 1263 healthy volunteers between 18-59 years were recruited from the same communities. We obtained written consent from all the study subjects. This study was approved by the Ethics Committee of Zhejiang Provincial Center for Disease Control and Prevention. We excluded individuals with cognitive impairment, mental illness, communication inability and cardiac pacemakers.
Measurement of skeletal muscle mass
Skeletal muscle mass was measured using bioelectrical impedance analysis (BIA) with the InBody S10 body composition analyzer (InBody Co., Ltd, Seoul, South Korea). During testing, the study subjects adopted an erect position on an empty stomach.
Measurement of handgrip strength (HS)
Muscle strength was measured by estimating the handgrip strength of the main hand twice with a hand-held dynamometer instrument. The higher value was used for analysis.
Measurement of physical performance
Physical performance was assessed by estimating the gait speed (GS). The participants walked along a straight path for more than 8 meters at their usual speed and the gait speed was calculated for the middle 6-meter course.
Diagnosis of sarcopenia
Sarcopenia was diagnosed based on the estimation of five different criteria, namely, local Standard, EWGSOP1 [1], EWGSOP2 [16], AWGS 2014 [11] and AWGS 2019 [17] as shown in Table 4.
Table 4. Criteria for the diagnosis of sarcopenia.
| Diagnosis is based on documentation of criterion 1 plus (criterion 2 or criterion 3) | |||||
| local standard* | EWGSOP 1 | EWGSOP 2** | AWGS(2014) | AWGS(2019) | |
| 1.Muscle mass(BIA) | male <6.4 kg/m2 female <5.0 kg/m2 | male <6.4 kg/m2 female <5.0 kg/m2 | male <6.4 kg/m2 female <5.0 kg/m2 | male <7.0 kg/m2 female <5.7 kg/m2 | male <7.0 kg/m2, female <5.7 kg/m2 |
| 2.Muscle strength | male <26 kg, female <18 kg | Male <30kg, female <20kg | male <27 kg, female <16 kg | male <26 kg, female <18 kg | male <28 kg, female <18 kg |
| 3. Performance | GS≤0.8m/s | GS ≤0.8m/s | —— | GS <0.8m/s | GS <1.0m/s |
local Standard*: In reference to EWGSOP1, the SMI of the local Standard is 2 standard deviations below the mean of young adults aged 18-39 in the study groups (male <6.4 kg/m2 female <5.0 kg/m2) and the gait speed at ≤0.8m/s. The handgrip strength was modified compared to AWGS 2014 and was below 26 Kg for males and below 18 Kg for females. EWGSOP2**: The SMI of the local Standard was 2 standard deviations below the mean of young adults aged 18-39 in the study group (male<6.4 kg/m2 female<5.0 kg/m2). The handgrip strength was below 27 Kg for males and <16 Kg for females.
Data collection
We estimated the muscle mass, strength and function in 1685 volunteers by measuring body composition, handgrip strength and gait speed, respectively. The study subjects were divided into 3 age groups, namely, 541 individuals aged between 18-39 years (Average age: 28.49 ± 6.402), 722 individuals aged between 40-59 years (Average age: 49.99 ± 5.147), and 422 individuals aged 60 years and above (Average age: 67.84 ± 6.861).
Statistical analyses
Fisher’s exact test was used to compare differences in sarcopenia prevalence between different age groups. Pearson correlation analysis was performed to determine the relationship between various indicators of sarcopenia and age. Single Factor ANOVA was used to compare the differences in skeletal mass index (SMI) between the age groups, and Tukey’s multiple comparisons test was applied for pairwise comparison. Statistical analysis was performed using SPSS software version 20.0 (SPSS Inc., Chicago, Illinois, USA).
Acknowledgments
We thank all the participants for their support in this study. We also thank Jiayan Jiang, Hua Jiang, Fenna Zhang, Weijun Le, and Kefeng Li for their help in data collection and Inbody Company (InBody Co., Ltd, Korea) for its free assistance in technical and equipment support for the body composition analyses.
Footnotes
AUTHOR CONTRIBUTIONS: Jie Huang and Fan He jointly proposed the concept of this research and designed this experiment. Zhendong Tong, Shoushun Chen, Suya Zhong made a positive contribution to the data collectiom. Jie Huang, Xue Gu, have jointly analyzed and interpreted the data. Jie Huang and Suya Zhong have drafted and revised the manuscript.
CONFLICTS OF INTEREST: The authors declare that they have no conflicts of interest.
FUNDING: This work was supported by the Zhejiang Provincial Medical and Health Science and Technology Program (2020RC005).
REFERENCES
- 1.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M, and European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–23. 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anker SD, Morley JE, von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. 2016; 7:512–14. 10.1002/jcsm.12147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vellas B, Fielding RA, Bens C, Bernabei R, Cawthon PM, Cederholm T, Cruz-Jentoft AJ, Del Signore S, Donahue S, Morley J, Pahor M, Reginster JY, Rodriguez Mañas L, et al. Implications of ICD-10 for sarcopenia clinical practice and clinical trials: report by the international conference on frailty and sarcopenia research task force. J Frailty Aging. 2018; 7:2–9. 10.14283/jfa.2017.30 [DOI] [PubMed] [Google Scholar]
- 4.Patel HP, Syddall HE, Jameson K, Robinson S, Denison H, Roberts HC, Edwards M, Dennison E, Cooper C, Aihie Sayer A. Prevalence of sarcopenia in community-dwelling older people in the UK using the European working group on sarcopenia in older people (EWGSOP) definition: findings from the hertfordshire cohort study (HCS). Age Ageing. 2013; 42:378–84. 10.1093/ageing/afs197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen M, Bai H, Wang C, Wang Y, Xue DH, Xie H, Yi Q, Li Z, Li R, Gao ZH, Sun JQ. Establishment of muscle mass diagnostic standard of sarcopenia using a bioelectrical impedance analysis and epidemiological investigation of the elderly in Shanghai. Chinese Journal of Geriatrics. 2015; 34:483–6. [Google Scholar]
- 6.Morley JE. Sarcopenia: diagnosis and treatment. J Nutr Health Aging. 2008; 12:452–56. 10.1007/BF02982705 [DOI] [PubMed] [Google Scholar]
- 7.Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998; 147:755–63. 10.1093/oxfordjournals.aje.a009520 [DOI] [PubMed] [Google Scholar]
- 8.Silva AM, Shen W, Heo M, Gallagher D, Wang Z, Sardinha LB, Heymsfield SB. Ethnicity-related skeletal muscle differences across the lifespan. Am J Hum Biol. 2010; 22:76–82. 10.1002/ajhb.20956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNally EM. Powerful genes—myostatin regulation of human muscle mass. N Engl J Med. 2004; 350:2642–44. 10.1056/NEJMp048124 [DOI] [PubMed] [Google Scholar]
- 10.Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, Montori VM, and Task Force, and Endocrine Society. Testosterone therapy in men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2010; 95:2536–59. 10.1210/jc.2009-2354 [DOI] [PubMed] [Google Scholar]
- 11.Lee K, Shin Y, Huh J, Sung YS, Lee IS, Yoon KH, Kim KW. Recent issues on body composition imaging for sarcopenia evaluation. Korean J Radiol. 2019; 20:205–17. 10.3348/kjr.2018.0479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014; 15:95–101. 10.1016/j.jamda.2013.11.025 [DOI] [PubMed] [Google Scholar]
- 13.Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM, Kiel DP, Kritchevsky SB, Shardell MD, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014; 69:547–58. 10.1093/gerona/glu010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, De Meynard C, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011; 12:249–56. 10.1016/j.jamda.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiles Shaffer N, Simonsick EM, Thorpe RJ, Studenski SA. The roles of body composition and specific strength in the relationship between race and physical performance in older adults. J Gerontol A Biol Sci Med Sci. 2020; 75:784–91. 10.1093/gerona/glz103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jensen B, Moritoyo T, Kaufer-Horwitz M, Peine S, Norman K, Maisch MJ, Matsumoto A, Masui Y, Velázquez-González A, Domínguez-García J, Fonz-Enríquez E, Salgado-Moctezuma SG, Bosy-Westphal A. Ethnic differences in fat and muscle mass and their implication for interpretation of bioelectrical impedance vector analysis. Appl Physiol Nutr Metab. 2019; 44:619–26. 10.1139/apnm-2018-0276 [DOI] [PubMed] [Google Scholar]
- 17.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, et al. , and Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31. 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, Kojima T, Kuzuya M, Lee JS, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21:300–07.e2. 10.1016/j.jamda.2019.12.012 [DOI] [PubMed] [Google Scholar]
- 19.Zhang L, Guo Q, Feng BL, Wang CY, Han PP, Hu J, Sun XD, Zeng WF, Zheng ZX, Li HS, Zhou LB, Luo Q, Jiang LF, Ye HH. A cross-sectional study of the association between arterial stiffness and sarcopenia in Chinese community-dwelling elderly using the Asian working group for sarcopenia criteria. J Nutr Health Aging. 2019; 23:195–201. 10.1007/s12603-018-1147-9 [DOI] [PubMed] [Google Scholar]
- 20.Hai S, Cao L, Wang H, Zhou J, Liu P, Yang Y, Hao Q, Dong B. Association between sarcopenia and nutritional status and physical activity among community-dwelling Chinese adults aged 60 years and older. Geriatr Gerontol Int. 2017; 17:1959–66. 10.1111/ggi.13001 [DOI] [PubMed] [Google Scholar]
- 21.Wu LJ. Meta-analysis on the prevalence of sarcopenia in the elderly in Chinese communities. Modern Preventive Medicine. 2019; 46:4109–12. [Google Scholar]
- 22.Lau EM, Lynn HS, Woo JW, Kwok TC, Melton LJ 3rd. Prevalence of and risk factors for sarcopenia in elderly Chinese men and women. J Gerontol A Biol Sci Med Sci. 2005; 60:213–16. 10.1093/gerona/60.2.213 [DOI] [PubMed] [Google Scholar]
- 23.Zeng P, Wu S, Han Y, Liu J, Zhang Y, Zhang E, Zhang Y, Gong H, Pang J, Tang Z, Liu H, Zheng X, Zhang T. Differences in body composition and physical functions associated with sarcopenia in Chinese elderly: reference values and prevalence. Arch Gerontol Geriatr. 2015; 60:118–23. 10.1016/j.archger.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 24.Cesari M, Penninx BW, Pahor M, Lauretani F, Corsi AM, Rhys Williams G, Guralnik JM, Ferrucci L. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2004; 59:242–48. 10.1093/gerona/59.3.m242 [DOI] [PubMed] [Google Scholar]
- 25.Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BW, Lenchik L, Palla SL, Ambrosius WT, Tracy RP, Pahor M. Sarcopenia, obesity, and inflammation—results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study. Am J Clin Nutr. 2005; 82:428–34. 10.1093/ajcn.82.2.428 [DOI] [PubMed] [Google Scholar]
- 26.Karasik D, Cohen-Zinder M. The genetic pleiotropy of musculoskeletal aging. Front Physiol. 2012; 3:303. 10.3389/fphys.2012.00303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu R, Wong M, Leung J, Lee J, Auyeung TW, Woo J. Incidence, reversibility, risk factors and the protective effect of high body mass index against sarcopenia in community-dwelling older Chinese adults. Geriatr Gerontol Int. 2014. (Suppl 1); 14:15–28. 10.1111/ggi.12220 [DOI] [PubMed] [Google Scholar]
- 28.Tramontano A, Veronese N, Sergi G, Manzato E, Rodriguez-Hurtado D, Maggi S, Trevisan C, De Zaiacomo F, Giantin V. Prevalence of sarcopenia and associated factors in the healthy older adults of the Peruvian andes. Arch Gerontol Geriatr. 2017; 68:49–54. 10.1016/j.archger.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 29.Sayer AA, Syddall H, Martin H, Patel H, Baylis D, Cooper C. The developmental origins of sarcopenia. J Nutr Health Aging. 2008; 12:427–32. 10.1007/BF02982703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, Der G, Gale CR, Inskip HM, Jagger C, Kirkwood TB, Lawlor DA, Robinson SM, et al. Grip strength across the life course: normative data from twelve British studies. PLoS One. 2014; 9:e113637. 10.1371/journal.pone.0113637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2014; 3:346–50. [PMC free article] [PubMed] [Google Scholar]
- 32.Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R. Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol (1985). 2000; 88:1321–26. 10.1152/jappl.2000.88.4.1321 [DOI] [PubMed] [Google Scholar]
- 33.Peterson SJ, Mozer M. Differentiating sarcopenia and cachexia among patients with cancer. Nutr Clin Pract. 2017; 32:30–39. 10.1177/0884533616680354 [DOI] [PubMed] [Google Scholar]
- 34.Chen CM. Guidelines for the prevention and control of overweight and obesity in Chinese adults. People's Medical Publishing House. 2006; 46. [Google Scholar]
- 35.Larsson L. Histochemical characteristics of human skeletal muscle during aging. Acta Physiol Scand. 1983; 117:469–71. 10.1111/j.1748-1716.1983.tb00024.x [DOI] [PubMed] [Google Scholar]
- 36.Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007; 297:1772–74. 10.1001/jama.297.16.1772-b [DOI] [PubMed] [Google Scholar]
- 37.Bowden Davies KA, Pickles S, Sprung VS, Kemp GJ, Alam U, Moore DR, Tahrani AA, Cuthbertson DJ. Reduced physical activity in young and older adults: metabolic and musculoskeletal implications. Ther Adv Endocrinol Metab. 2019; 10:2042018819888824. 10.1177/2042018819888824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sayer AA, Syddall HE, Gilbody HJ, Dennison EM, Cooper C. Does sarcopenia originate in early life? findings from the Hertfordshire cohort study. J Gerontol A Biol Sci Med Sci. 2004; 59:M930–34. 10.1093/gerona/59.9.m930 [DOI] [PubMed] [Google Scholar]