Abstract
Evidence suggests priorities differ between patients in HIV care and their providers regarding topics most important to address in care. At five U.S. sites, we asked patients and providers to prioritize 25 potential topic areas to address during routine visits, and invited patients to discuss selection rationale. Patients (n=206) and providers (n=17) showed high discordance in rank order priorities (Γ2 (24, 223)=71.12; p<0.0001). Patients ranked social domains such as HIV stigma highly; a higher proportion of providers prioritized substance use domains. HIV stigma was a higher priority for patients in care fewer than 6 years (Fisher’s exact p=0.0062), nonwhite patients (Fisher’s exact p=0.0114), and younger patients (Fisher’s exact p=0.0281). Patients’ priorities differed between men and women (Γ2 (24, 188)=52.89; p<0.0001), white race vs. other races (Γ2 (24, 206)=48.32; p=0.0023), and Latinos vs. non-Latinos (Γ2 (24, 206)=48.65; p=0.0021). Interviews (n=79) revealed perceived impact of social context on health and health behaviors.
Resumen
Las pruebas sugieren que los pacientes en tratamiento anti-VIH y los proveedores de aquél tienen prioridades distintas sobre qué aspectos más importantes abordar en el tratamiento. En cinco centros estadounidenses, pedimos a pacientes y proveedores que priorizaran 25 posibles aspectos a abordar durante las consultas de rutina, e invitamos a los pacientes a explicar los motivos de sus elecciones. Entre pacientes (n=206) y proveedores (n=17) hubo una disparidad alta a la hora de ordenar sus prioridades (Γ2 (24, 223)=71,12; p<0,0001). Los pacientes dieron gran importancia a los aspectos sociales, tales como el estigma asociado al VIH; una mayor proporción de proveedores dio mayor importancia a lo relativo al uso de sustancias. El estigma asociado al VIH fue una prioridad más alta para los pacientes en tratamiento durante menos de 6 años (prueba exacta de Fisher p=0,006), pacientes de raza no blanca (prueba exacta de Fisher p=0,0114) y pacientes más jóvenes (prueba exacta de Fisher p=0.0281). Las prioridades de los pacientes difirieron entre hombres y mujeres (Γ2 (24, 188)=52,89; p<0,0001), raza blanca frente a otras razas (Γ2 (24, 206)=48,32; p=0,0023), y origen latino frente a no latino ((Γ2 (24, 206)=48.65; p=0.0021). Las entrevistas (n=79) realizadas revelaron una percepción del efecto del contexto social sobre la salud y los comportamientos relacionados con la salud.
Introduction
The movement toward patient-centered care, a cornerstone of the Chronic Care Model, (1–4) works toward meaningful inclusion of patient perspectives in their care and a framework of active partnership with patients in making treatment decisions. Patient-centered care is associated with decreased health care utilization,(5) lower costs,(5) and improved patient-provider communication.(6) High-quality patient-provider relationships, grounded in a positive communication dynamic in which both patients and providers are able to address their respective priorities, are central to the success of patient-centered care.(7, 8)
Evidence from our own work suggests that patients in HIV care may have different priorities than their health care providers regarding what topics are most important to address during the context of routine clinic visits.(9) For example, in a rank order exercise conducted with HIV care providers and their patients, we found that providers prioritized behavioral domains such as substance use more highly, while patients placed higher value on addressing context-based domains, such as the impact of HIV-related stigma on their lives and health.(9) Concerningly, we found strong discordance between priorities in HIV care between providers and patients recently diagnosed with HIV (≤5 years, p<0.001) as well as substantial differences by sex and race. (9)
The typically time-constrained nature of clinic visits may make it difficult to effectively identify and address multiple patient concerns, and highlights the need to prioritize what to address.(10) Patient priorities may not get communicated during clinic visits. This communication gap may be mitigated by pre-visit collection of patient-reported outcomes (PROs), which are reports generated directly from patients describing function or feelings in relation to one or more health conditions and their treatments. (11) In HIV care, electronic pre-visit PRO collection significantly improved provider ability to identify depression, poor antiretroviral adherence, and substance abuse,(12) making it possible to effectively tailor the visit to make the best use of time addressing patient needs. Meaningful PRO integration into care requires selection of PRO domains that both reflect patient priorities and are most clinically relevant to providers.(13, 14)
We sought to build on our preliminary evaluation of health domain priorities among HIV care providers and patients by understanding which PRO domains patients and providers value most highly. We were particularly interested in gaining insight into the priorities of patients from socially and/or economically marginalized populations living with HIV whose perspectives are often underrepresented.
Methods
Patient involvement
We included boards of patients from 3 sites in this study in accordance with IAP2 Spectrum of Public Participation guidelines.(15) We routinely consulted and sought approval from a board of patients living with HIV (PLWH) from the University of Washington’s Madison Clinic to develop and pilot test rank order exercises, to review and further develop interview guides, and to develop analysis and interpret results. Patient boards from 2 additional clinics (Fenway Community Health and University of Alabama 1917 Clinic) contributed to the analytic phase by providing insight on possible overarching rationales for rank order choices, and ultimately approved proposed interpretations and implications of study results.
Study participants
We recruited PLWH from five geographically diverse clinics within the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS), a U.S. consortium of clinical practice research sites providing care for a demographically heterogeneous cohort of ~30,000 people living with HIV. Collection sites were: the 1917 Clinic (University of Alabama-Birmingham), Owen Clinic (University of California-San Diego), Ward 86 at Zuckerberg San Francisco General Hospital (University of California-San Francisco), Fenway Community Health in Boston, MA, and the Madison Clinic (University of Washington in Seattle, WA). We prioritized recruitment of the following under-represented and/or marginalized patient populations in HIV care: transgender women; cis-gender women; people aged 55 or over, or under age 30; Latinos/Latinas, including those whose primary language is Spanish; African-Americans; patients poorly engaged in HIV care (defined as having missed 1 or more visits in two consecutive 6-month periods over the past two years); patients who self-reported living in rural areas; and patients living with HIV for fewer than 6 years. We strove for broad geographic representation within all demographic groups. Research coordinators approached patients scheduled for their routine clinic visit in a private waiting room to invite them to participate. We recruited HIV care providers in-person from 8 sites within the CNICS network attending a national meeting (2/2015). We gained Institutional Review Board approval to administer informed consent to UW patients through the University of Washington; other sites gained approval through their respective institutions.
Data collection
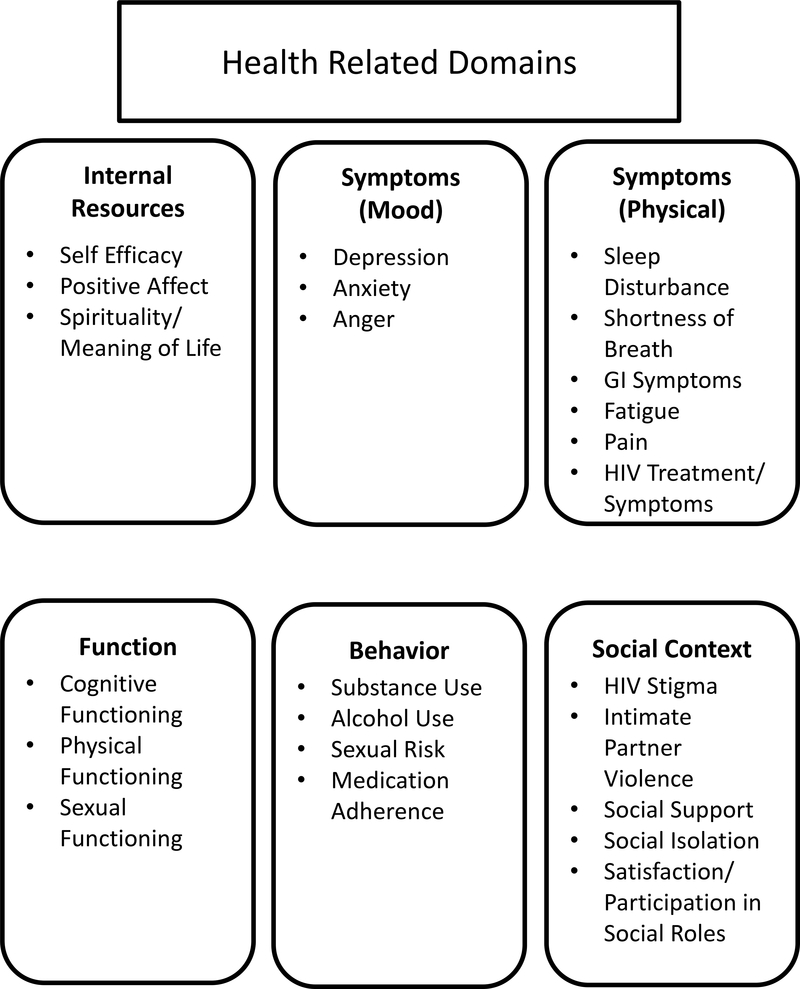
We used an explanatory sequential mixed-methods study design in which we sought explanation for quantitative data through qualitative data collection. (16) We invited patients, and, separately, providers, to rank their top 8 and bottom 3 priorities for domains to address in the context of a typical routine HIV clinical care visit, based on a set of 25 domains (see Figure 1)(17) between May 2015 and December 2016. Participants were allotted 10 minutes to complete the exercise. The 25 domains included dimensions of symptoms/functioning such as HIV/treatment-related symptoms, depression, pain, fatigue, sleep disturbance, gastrointestinal symptoms, shortness of breath, anger, anxiety, and cognitive, physical, and sexual functioning; behavior including alcohol abuse, substance abuse, tobacco use, medication adherence, sexual risk behavior; social context including social support, social isolation, social roles, HIV stigma, intimate partner violence; and personal/internal resources including positive affect, self-efficacy, spirituality/meaning of life. Providers performed the rank order task by reviewing the list of 25 domain names and writing their top 8 and bottom 3 into their selected rank order on paper. Patients performed a similar rank-ordering task, in which they were presented with 25 notecards, each showing a health domain name. We asked patients to spread the cards out onto a large table, and spend as much time as needed to select their top 8 and bottom 3 domains.
Fig 1.
Health-related domains
We invited patients to explain their rationales for their rank order choices immediately after completion, including how they would want providers to address high-ranked domains, in the form of a pre-written semi-structured 1:1 interview. Patients completing the rank order exercise without a subsequent 1:1 interview received $20; those completing the rank order exercise and subsequent interview received $40. Providers were not compensated. We did not perform similar interviews with providers, as our prior findings of high prioritization concordance between providers(9) rendered it less relevant to discern their individual rank order rationales.
We digitally recorded and sent interviews for transcription to an independent transcription agency (Verbal Ink).
Data analysis
We conducted quantitative and qualitative data analyses concurrently and separately.
Rankings
We examined overall ranking among patients and providers, as well as rankings between subgroups of patients and between subgroups of patients and providers. For these analyses, providers served as the reference category, and they were not sub-divided based on any other characteristics. The patient subgroups considered for analyses were based on gender (cis-gender male, cis-gender female, or transgender female [defined as birth sex male/current gender identity female]), rural/suburban/urban, self-reported race/ethnicity (African-American, White, Latino), detectable viral load, at least 6 years since diagnosis, level of engagement in HIV care, and current drug use (cocaine, methamphetamines, or illicit opiates). Overall rankings were compared using a method from Holander and Sethuraman, which results in a test statistic with a chi-squared distribution.(18) The proportions ranking each domain in the top 8 were compared using Fisher’s exact test, which is an exact p-value and as such has no test statistic. In addition, due to the marked differences between patients and providers observed in earlier work in prioritization of social and behavioral domains (9), we were interested in which patient factors most strongly accounted for any differences in patient and provider rankings in HIV stigma, social support, alcohol abuse, substance abuse, and sexual risk. For this, we used Poisson regression with robust standard errors to obtain the incidence rate ratio (IRR). Due to sample size constraints, separate models were fit for each grouping variable, and we did not attempt to perform additional stratified analyses (e.g. both race and age in a single model), except for within-race sex differences.
Interviews
We created excerpts from transcribed interview content using Dedoose qualitative analysis software (19) and analyzed data using variants of the Content Analysis (CA) approach. (20) Using a directed CA approach (21) two coders independently coded content corresponding to any of 25 domain areas. A third coder evaluated all codes to reconcile differences when they arose. Next, two coders used a conventional CA approach, independently open-coding content within each of the domain areas to identify meta-rationales. Once reaching consensus on final meta-rationale codes, we re-coded excerpts according to these additional codes.
Results
Rank order exercise: patients vs. providers
Patients (n=206, mean age 46; 62% cisgender male, 30% cisgender female, 9% male-to-female transgender; 37% White, 33% African-American, 28% Latino, see Table 1) and providers (n=17) showed high discordance in rank order priorities (Γ2 (24, 223)=71.12; p<0.0001). Table 2 shows rank orderings for providers, patients overall, and patients by age, gender, and race; Table S1 shows additional patient sub-groups. Notably, all substance use domains were present in the provider top 8 but absent from the patient top 8, while the patients’ top 8 included social-related domains, such as HIV stigma and social support.
Table 1.
Patient demographic and clinical characteristics
| Ranking Participants N=206 |
Interview Participants N=79 |
|
|---|---|---|
| Age | ||
| < 30 | 23 (11%) | 13 (16%) |
| 30–54 | 138 (67%) | 49 (62%) |
| ≥55 | 45 (22%) | 17 (22%) |
| Gender | ||
| Cisgender male | 127 (62%) | 40 (51%) |
| Cisgender Female | 61 (30%) | 27 (34%) |
| MTF | 18 (9%) | 12 (15%) |
| Race/ethnicity | ||
| African-American | 67 (33%) | 34 (43%) |
| White | 76 (37%) | 19 (24%) |
| Asian | 2 (1%) | 1 (1%) |
| Hawaiian/Pacific Islander | 2 (1%) | 2 (3%) |
| Native American | 2 (1%) | 2 (3%) |
| Latino | 57 (28%) | 23 (29%) |
| Language* | ||
| English | 176 (85%) | 69 (87%) |
| Spanish | 30 (15%) | 10 (13%) |
| Sexual Orientation | ||
| Lesbian/Gay | 82 (52%) | 28 (46%) |
| Bisexual | 16 (10%) | 6 (10%) |
| Heterosexual | 59 (38%) | 27 (44%) |
| Urbanicity | ||
| Rural | 21 (10%) | 10 (13%) |
| Suburban | 66 (32%) | 21 (27%) |
| Urban | 119 (58%) | 48 (61%) |
| Engagement in HIV care | ||
| Well engaged | 126 (75%) | 46 (77%) |
| Less engaged | 43 (25%) | 14 (23%) |
| Years living with HIV | ||
| 0–5 | 62 (30%) | 26 (33%) |
| ≥6 | 144 (70%) | 53 (67%) |
| Viral Load (copies/mL) | ||
| <400 | 131 (71%) | 50 (68%) |
| ≥400 | 53 (29%) | 23 (32%) |
MTF: male-to-female transgender patient
Language in which domain importance exercise/interview conduct
Table 2.
Top 8 and bottom 3 rank order selections of providers, patients, and patients by age, gender, and race
| Rank | Providers | All Patients | Age <30 | Age 30–54 | Age ≥55 | |
| 1 | Substance Abuse | Medication Adherence | Medication Adherence | Medication Adherence | HIV Treatment/ Symptoms | |
| 2 | Depression | HIV Treatment/ Symptoms | HIV Treatment/ Symptoms | HIV Treatment/ Symptoms | Medication Adherence | |
| 3 | Medication Adherence | Depression | Depression | Depression | Pain | |
| 4 | Alcohol Abuse | Sexual Risk Behavior | HIV Stigma | Sexual Risk Behavior | Depression | |
| 5 | Tobacco Use | HIV Stigma | Sexual Risk Behavior | HIV Stigma | Cognitive Function | |
| 6 | Sexual Risk Behavior | Pain | Social Support | Pain | Sexual Risk Behavior | |
| 7 | HIV Treatment/ Symptoms | Physical Function | Positive Affect | Physical Function | HIV Stigma | |
| 8 | Cognitive Function | Social Support | Physical Function | Substance Abuse | Social Support | |
| … | … | … | … | … | ||
| 23 | Shortness of Breath | Anger | Tobacco Use | Shortness of Breath | Domestic Violence or IPV | |
| 24 | Positive Affect | Shortness of Breath | Sexual Function | Tobacco Use | Anger | |
| 25 | Spirituality or Meaning of Life | Tobacco Use | Shortness of Breath | Sexual Function | Tobacco Use | |
| Rank | Men | Women | Male to Female Transgender | African American | White | Latino |
| 1 | Medication Adherence | HIV Treatment/ Symptoms | HIV Treatment/ Symptoms | HIV Treatment/ Symptoms | Medication Adherence | Medication Adherence |
| 2 | HIV Treatment/ Symptoms | Medication Adherence | Medication Adherence | Medication Adherence | HIV Treatment/ Symptoms | HIV Treatment/ Symptoms |
| 3 | Depression | Pain | Cognitive Function | Sexual Risk Behavior | Depression | HIV Stigma |
| 4 | Sexual Risk Behavior | Sexual Risk Behavior | Physical Function | HIV Stigma | Physical Function | Depression |
| 5 | HIV Stigma | Depression | Sexual Risk Behavior | Depression | Pain | Sexual Risk Behavior |
| 6 | Physical Function | Social Support | Depression | Pain | Sexual Risk Behavior | Social Support |
| 7 | Substance Abuse | Cognitive Function | HIV Stigma | Social Support | Cognitive Function | Substance Abuse |
| 8 | Pain | HIV Stigma | Anxiety | Cognitive Function, Physical Function (tie) | Fatigue | Pain |
| … | … | … | … | … | … | |
| 23 | Tobacco Use | Sexual Function | Social Isolation | Sleep Disturbance | Sexual Function | Domestic Violence or IPV |
| 24 | Domestic Violence or IPV | Alcohol Abuse | Sexual Function | Alcohol Abuse | Participation in Social Roles | Shortness of Breath |
| 25 | Shortness of Breath** | Tobacco Use | Anger | Tobacco Use | Spirituality or Meaning of Life | Anger |
Tied with item above.
Table 3 shows the proportion of patients rating each domain in the top 8, in comparison with providers. Higher proportions of patients prioritized positive affect (p=0.0039), fatigue (p=0.0081), spirituality/meaning of life (p=0.0148), HIV stigma (p=0.0208), and sleep disturbance (p=0.0271) in their top 8, while higher proportions of providers prioritized substance use (p<0.0001), alcohol use (<0.0001), tobacco use (p<0.0001), depression (p<0.0001), and sexual risk behavior (p=0.0112) (all p-values from Fisher’s exact test).
Table 3.
Percent of providers or patients rating a domain in top 8*.
| Providers | Patients | p-value | |
|---|---|---|---|
| Alcohol abuse | 82 | 19 | < 0.0001 |
| Anger | 0 | 16 | 0.1412 |
| Anxiety | 29 | 24 | 0.5736 |
| Cognitive function | 47 | 33 | 0.2887 |
| Depression | 100 | 55 | < 0.0001 |
| Domestic violence/IPV | 29 | 13 | 0.0767 |
| Fatigue | 0 | 27 | 0.0081 |
| Gastrointestinal symptoms | 6 | 24 | 0.1289 |
| HIV and treatment symptoms | 53 | 73 | 0.0924 |
| HIV stigma | 18 | 48 | 0.0208 |
| Medication adherence | 94 | 76 | 0.1294 |
| Pain | 41 | 40 | 1.0000 |
| Physical function | 18 | 40 | 0.1164 |
| Positive affect | 0 | 31 | 0.0039 |
| Self-efficacy | 12 | 27 | 0.2299 |
| Sexual function | 6 | 17 | 0.3184 |
| Sexual risk behavior | 82 | 50 | 0.0112 |
| Shortness of breath | 6 | 9 | 1.0000 |
| Sleep disturbance | 0 | 22 | 0.0271 |
| Social isolation | 0 | 17 | 0.0818 |
| Social roles | 0 | 18 | 0.0829 |
| Social support | 18 | 42 | 0.0699 |
| Spirituality/meaning of life | 0 | 26 | 0.0148 |
| Substance abuse | 94 | 36 | < 0.0001 |
| Tobacco use | 71 | 15 | < 0.0001 |
Fisher’s Exact test
IPV: intimate partner violence
Next, we examined which patient factors strongly accounted for patient-provider differences in rankings of HIV stigma, social support, alcohol abuse, substance abuse, and sexual risk. Compared with providers, younger patient age and length of time since HIV diagnosis were associated with ranking HIV stigma in the top 8 in separate models; those under 30 were nearly 4 times as likely as providers to rank HIV stigma in the top 8 (z=2.53, p=0.0115; IRR 3.94, 95% confidence interval [95% CI] 1.36, 11.42). Similar results were seen in patients diagnosed for less than six years (z=2.38, p=0.0173; IRR 3.56, 95% CI 1.25, 10.15). Compared to providers, higher proportions of Latino patients (z=2.38, p=0.0171; IRR 3.58, 95% CI 1.25, 10.21) and African-American patients (z=1.96, p=0.0499; IRR 2.87, 95% CI 1.00, 8.26) prioritized HIV stigma in their top 8 domains. Higher proportions of patients prioritized social support in their top 8, but this difference did not reach statistical significance, either overall or for any subgroup. In comparison with providers, lower proportions of patients ranked alcohol use, substance use, and sexual risk in their top 8, regardless of subgroup.
Rank order exercise: differences between patient groups
Top 8 and bottom 3 selections are listed in Tables 2 and S1. We found significant overall differences in rank ordering between cis-gender men and cis-gender women (Γ2 (24, 188)=52.89; p<0.0001), white race vs. other races (Γ2 (24, 206)=48.32; p=0.0023); Latinos vs. non-Latinos (Γ2 (24, 206)=48.65; p=0.0021), and African-American females vs. African-American males (Γ2 (24, 62)=38.10; p=0.0339). We found no single domain to be clearly driving the difference between cis-gender men and cis-gender women. Notably, despite the lower proportion of patients who prioritized behavioral domains such as substance use in their top 8 compared with providers, patients who reported currently using drugs (cocaine/crack, heroin, methamphetamines) were more likely than other patients to include the domain of substance use among the top 8 domains to discuss with providers (Table S2, Fisher’s exact p=0.0117).
Table 4 shows proportions of patients rating each domain in the top 8 by age, gender, race/ethnicity, and years since diagnosis, and Table S2 shows these proportions for additional patient subgroups (language spoken, sexual orientation, level of engagement in care, urbanicity, cocaine/amphetamine/opiate use, at risk alcohol use, and by level of medication adherence). Across age groups, higher proportions of younger patients selected HIV stigma in the top 8 domains (Fisher’s exact p=0.0281). Across race and ethnic groups, higher proportions of Latinos prioritized alcohol abuse (Fisher’s exact p=0.0301), higher proportions of Latinos and African-Americans prioritized HIV stigma (Fisher’s exact p=0.0114) and spirituality/meaning of life (Fisher’s exact p=0.0472); higher proportions of African-Americans prioritized social support (Fisher’s exact p=0.0440); and lower proportions of Latinos prioritized medication adherence (Fisher’s exact p=0.0242) and anger (Fisher’s exact p=0.037). Higher proportions of patients in HIV care for less than 6 years prioritized HIV stigma (Fisher’s exact p=0.0062) than those in care 6 or more years; higher proportions of those in HIV care 6 or more years prioritized HIV symptoms and treatment (Fisher’s exact p=0.0386), or substance use (Fisher’s exact p=0.0110) in their top 8 (Table 4). Patients who chose to participate in English prioritized anger more highly (Fisher’s exact p=0.0058) than Spanish-speaking patients, and patients who participated in Spanish prioritized alcohol abuse and tobacco use more highly (Fisher’s exact p=0.0009 andp=0.0236) (Table S2). Higher proportions of gay and bisexual patients prioritized alcohol use (Fisher’s exact p=0.0167) to discuss with providers than non-gay or bisexual patients; pain was prioritized more highly by bisexual and heterosexual patients (Fisher’s exact p=.0220). A lower proportion of urban patients prioritized sexual risk behavior in their top 8 compared to their suburban and rural counterparts (Fisher’s exact p=0.0467).
Table 4.
Percent of patients rating a domain in top 8, by subgroup*
| Age | Gender | Race/ethnicity | Years since diagnosis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 30 | 30–54 | ≥55 | p-value | Male | Female | MTF | p-value | Af. Am. | White | Latino | p-value | <6 | 6+ | p-value | |
| Alcohol abuse | 22 | 20 | 16 | 0.80 | 24 | 10 | 22 | 0.07 | 15 | 13 | 35 | 0.03 | 21 | 19 | 0.71 |
| Anger | 22 | 15 | 13 | 0.61 | 17 | 18 | 0 | 0.15 | 19 | 16 | 7 | 0.04 | 13 | 17 | 0.54 |
| Anxiety | 39 | 23 | 20 | 0.21 | 28 | 15 | 28 | 0.10 | 22 | 24 | 28 | 0.82 | 31 | 22 | 0.21 |
| Cognitive function | 17 | 33 | 42 | 0.12 | 25 | 41 | 61 | 0.004 | 30 | 37 | 32 | 0.77 | 26 | 36 | 0.20 |
| Depression | 74 | 54 | 49 | 0.13 | 57 | 52 | 50 | 0.78 | 52 | 59 | 54 | 0.72 | 53 | 56 | 0.76 |
| Domestic violence/IPV | 9 | 15 | 9 | 0.54 | 9 | 20 | 17 | 0.12 | 15 | 13 | 12 | 0.97 | 8 | 15 | 0.18 |
| Fatigue | 17 | 26 | 36 | 0.27 | 29 | 26 | 17 | 0.58 | 21 | 37 | 23 | 0.177 | 26 | 28 | 0.87 |
| Gastrointestinal symptoms | 17 | 22 | 31 | 0.40 | 28 | 16 | 22 | 0.23 | 13 | 30 | 28 | 0.10 | 19 | 26 | 0.38 |
| HIV and treatment symptoms | 70 | 72 | 78 | 0.72 | 69 | 79 | 83 | 0.27 | 78 | 79 | 63 | 0.04 | 63 | 78 | 0.04 |
| HIV stigma | 70 | 49 | 36 | 0.03 | 51 | 44 | 39 | 0.50 | 51 | 36 | 63 | 0.01 | 63 | 42 | 0.006 |
| Medication adherence | 78 | 75 | 76 | 1.00 | 75 | 75 | 83 | 0.82 | 76 | 86 | 63 | 0.02 | 79 | 74 | 0.60 |
| Pain | 22 | 41 | 49 | 0.09 | 37 | 51 | 28 | 0.11 | 43 | 46 | 32 | 0.34 | 37 | 42 | 0.64 |
| Physical function | 39 | 40 | 40 | 1.00 | 41 | 33 | 56 | 0.21 | 34 | 49 | 35 | 0.09 | 45 | 38 | 0.35 |
| Positive affect | 48 | 26 | 38 | 0.06 | 29 | 31 | 44 | 0.44 | 34 | 30 | 26 | 0.27 | 35 | 29 | 0.41 |
| Self-efficacy | 22 | 27 | 31 | 0.74 | 29 | 21 | 33 | 0.41 | 30 | 24 | 26 | 0.56 | 37 | 23 | 0.04 |
| Sexual function | 4 | 19 | 20 | 0.20 | 21 | 11 | 11 | 0.23 | 13 | 14 | 23 | 0.13 | 13 | 19 | 0.32 |
| Sexual risk behavior | 57 | 53 | 38 | 0.18 | 51 | 46 | 56 | 0.71 | 54 | 46 | 53 | 0.26 | 47 | 51 | 0.65 |
| Shortness of breath | 0 | 10 | 11 | 0.28 | 08 | 13 | 6 | 0.56 | 10 | 11 | 7 | 0.88 | 11 | 8 | 0.60 |
| Sleep disturbance | 22 | 21 | 24 | 0.90 | 22 | 25 | 11 | 0.51 | 19 | 24 | 21 | 0.59 | 26 | 20 | 0.37 |
| Social isolation | 17 | 17 | 18 | 1.00 | 16 | 26 | 0 | 0.02 | 19 | 14 | 19 | 0.65 | 16 | 18 | 0.84 |
| Social roles | 9 | 20 | 16 | 0.43 | 17 | 20 | 22 | 0.67 | 18 | 14 | 23 | 0.54 | 21 | 17 | 0.55 |
| Social support | 57 | 40 | 40 | 0.33 | 40 | 48 | 33 | 0.51 | 51 | 36 | 35 | 0.04 | 40 | 42 | 0.88 |
| Spirituality/meaning of life | 26 | 25 | 29 | 0.91 | 24 | 31 | 28 | 0.54 | 34 | 16 | 28 | 0.05 | 27 | 26 | 0.86 |
| Substance abuse | 30 | 40 | 27 | 0.25 | 39 | 34 | 22 | 0.41 | 33 | 36 | 39 | 0.96 | 23 | 42 | 0.01 |
| Tobacco use | 13 | 16 | 13 | 0.96 | 15 | 13 | 22 | 0.63 | 13 | 12 | 23 | 0.52 | 19 | 13 | 0.29 |
Fisher’s Exact test
IPV: intimate partner violence
Patient interviews
Interviews (n=79) supported the rank order results in that patients heavily prioritized social domains over behavioral domains. Patients often explained their rank order choices in terms of cause and effect, and revealed concern that negative social context adversely influenced other health domains, including depression and self-medicating behavior.
Most paramount were the effects of anticipated or actual HIV stigma, which often overwhelmed patients:
The stigma will bring you back to depression, and people still don’t understand, and it’s like [you] have to force it on them if you want people to understand…it just makes you feel like there’s nobody there for you, and it takes a lot to get over the stigma, and to trust people to tell, because you can’t handle everything on your own. Cisgender female, 49, Birmingham
…a lot of times people are broken by their stigma. Or they feel really worthless and nobody loves them because they have HIV. Which isn’t true, but it might be for some people …that just lead[s] to everything bad. Cisgender female, 36, Seattle
You feel like “they’re gonna start talking about me” and just the overall that you have it, you just feel like you don’t want to do anything because some people think I have it and I’m probably just gonna die. I might as well just not do anything about it…[you] start feeling depressed and not wanting to go out … start feeling isolated. I think that’s a big thing. Cisgender female, 31, San Diego
Many patients described anticipated or experienced HIV-related stigma as leading to social isolation, leading to depressed mood, which in turn led to decreased motivation to maintain health behaviors, such as remaining adherent to antiretroviral medication:
I know a lot of people that socially isolate themselves…they don’t want somebody to find out [about HIV positive status], or the ones that do know treat them differently. And so, they isolate themselves, and that comes along with depression and not wanting to take your meds. Cisgender female, 47, Seattle
If you don’t get over the [HIV] stigma…none of this matters. The isolation is gonna come in, right? You’re not gonna even care about the symptoms or the treatments. You’re not gonna take any of your medication, you’re gonna start that risky behavior. Cisgender male, 54, Birmingham
…you feel that…being [HIV] positive is affecting the way that you have relations with other people – you know, meaningful relationships… you feel it’s that other people won’t be able to deal with your HIV status. So, it can cause you anxiety, and along with that anxiety…depression. Cisgender male, 48, Boston
Patients also described the risk of engaging in self-medicating behavior due to HIV stigma and social isolation, such as substance abuse or sexual risk behavior, in order to try to feel better:
These [domains of social support, depression, sexual risk behavior] all come [after] stigma, for sure. Sexual risk behavior; I know of people who get the HIV and then they’re just kind of all out and they don’t care about anything because they feel like they just have everything; it can’t get any worse. Cisgender male, 24, Seattle
The depression is like I don’t care, I have sex with both of them – men, women or whatever. I don’t care. ‘I got [HIV] and I don’t want to live’…..that type of depression. Cisgender male, 44, San Francisco
[HIV stigma] is all you think of…it causes depression and then you want to use [drugs]…you’re gonna socially isolate yourself, because you don’t want to deal with [stigmatizing] people like that. Cisgender female, 47, Seattle
One patient described domains reinforcing each other within the cause and effect pattern, for example, anticipated HIV stigma leading to depression and social isolation:
When I first was diagnosed, I was depressed. I didn’t know who I could talk to. I didn’t know how to talk about it…it’s been a struggle, because you have to let some friends go, and you knew you couldn’t tell this person, because they were going to act like this, and you’ve got all these thoughts going on in your head, and people treating you different when you thought that you could trust them, and people saying negative and ugly things.... Cisgender female, 49, Birmingham
The presence of a chronic physical symptom, i.e., pain, was described by some patients as having a similar “domino” effect on functioning, and in turn mood and behavior:
Most of my other HIV (positive) friends do have a lot of pain and their pain leads to depression, substance abuse, [poorer] physical function. Cisgender female, 36, Seattle
If I’m fatigued I know I’m gonna have more problem with cognitive [functioning]. If I’m not sleeping well I’m gonna have more trouble with fatigue and the cognitive. If I’m depressed I’m gonna have more. Cisgender female, 50, Seattle
Patients who had been living with HIV for several years described an evolution of domain priorities over time, with HIV stigma and depression being initially very important upon learning of their diagnosis:
‘Now, the reason why I have them in this order is because when I first found out about me being diagnosed, these first three [depression, HIV stigma, spirituality/meaning of life] it hit me hard. I was depressed. I didn’t want to be around…I didn’t know how to handle it at first… these three really stood out because of the simple fact that I really felt like I was by myself. Cisgender female, 25, Seattle
Patient feedback: how might providers address domains important to patients?
High prioritization of social context-related domains was clear in most interviews. We asked patients how they believed providers could best address such domains (i.e. HIV stigma, social support, social isolation). Many patients acknowledged that there may be no ‘easy fix’ to these context-based problems. However, patients reported deep appreciation of providers at least acknowledging the difficult circumstances. Patients appreciated providers sincerely asking “how it’s going” in the social realm of their lives. Other suggestions included: acknowledgement of the impact of stigma on their quality of life; treating depression; mental health referrals to assist in coping with stigma; timely access to mental health care; more patient education to help debunk others’ myths about HIV transmissibility; referral/access to social support outlets; and making patients aware of opportunities to connect with other patients.
Discussion
PLWH and their providers may have different priorities regarding what broad areas should be addressed in the context of a routine clinic visit. While we found relative concordance between patients and providers on the importance of addressing certain domains [e.g., medication adherence, depression, and HIV-related symptoms], we found that patients prioritized social context-based domains [e.g., HIV stigma, social support] more highly than providers, and providers prioritized addressing behavioral domains, such as substance use, more highly than patients. Many patients felt it important that their health care address the at-times overwhelming context-based problems in their lives, such as anticipated or experienced HIV stigma and its resulting psychosocial impact (22), to meaningfully address adverse health behaviors. Addressing HIV stigma in care was particularly important to those of younger age, people in HIV care >6 years, and/or people with African-American race or Latino/Latina ethnicity.
Our study highlights an opportunity to acknowledge broad, socially-based root problems such as HIV stigma or lack of social support in order to impact health behaviors and symptoms. For population groups that have been less well-retained in HIV care, such as African-American and younger patients,(23, 24) addressing this priority could promote retention. The question is: how to address such issues in the context of a time-constrained clinic visit with a patient population that often presents with multiple conditions or problems? When specifically asked how providers could address these concerns, patients indicated that they want their provider to show interest and to demonstrate familiarity with the social realms of their lives. Most patients did not expect such problems to be solved during the visit; showing interest, demonstrating familiarity, and availing of mental health and social support-related referrals were sufficient. Some patients expressed interest in developing communication skills surrounding HIV disclosure; for this, referral to health educators could improve patients’ ability to navigate negative reactions. Most patients wanted to be “known” by their providers, and, in some cases, to be offered resources for bolstering social support and/or helping address stigma. Provider acknowledgment of these issues may strengthen the patient-provider relationship and thereby improve the likelihood of successfully addressing behavioral domains.
Discordance in patient-provider priorities is not unique to HIV care, and has been noted in other populations, including geriatric care and psychiatry. (25, 26) The growing number of aging patients living with multiple chronic conditions is likely to also have many concerns to address during a clinic visit. In the U.S. healthcare system, the number of concerns per primary care visit has increased, as has volume of work; resulting in less time to address each concern. (10, 27) In HIV care, patients on antiretroviral regimens now live much longer, in many cases developing multiple chronic conditions over time. Given the combination of patient-provider priority discordance in HIV care, and the increase in number of concerns to prioritize, patient-provider communication, as well as quality of care, may suffer. Effective patient-centered care requires elicitation of patients’ needs. Brief technology-based solutions, such as the use of a computer-based discussion prioritization tool,(28) have helped to identify and prioritize patient stressors among patients with multiple chronic conditions, without lengthening visits.(6) Similarly, in HIV care, collection of PROs has improved provider identification of antiretroviral adherence, depression, and substance abuse,(12) and improved providers’ ability to prioritize patient needs.(29) Identifying the health-related priorities of patients in HIV care offers providers a roadmap for collaborative treatment planning, and gives us possible starting points, such as addressing HIV stigma; acknowledging and addressing broader social-realm problems in the context of clinic visits may improve patient-provider relationships and improve the ability to successfully treat conditions such as depression, more effectively address the desire to self-medicate, and improve patients’ motivation to engage in behavior that sustains or improves their health.
Strengths
We included PLWH in study design, piloting and refining of study materials, and in interpreting results. In addition, we recruited a demographically and geographically diverse study population.
Limitations
A key study limitation is that the number of statistical tests performed may render false positive associations in the proportion ranking a domain in the top 8. Despite our efforts to recruit with geographic diversity in mind for each sub-group, we note that priorities of any sub-group may not be representative of other PLWH within that group. Despite recruitment efforts, our sample of Latina patients was small, which reflects CNICS cohort characteristics. We did not interview providers; doing so may have revealed nuanced context for prioritization, such as referring more ‘social’ domains to an on-site social worker, or prioritizing differently for particular marginalized sub-populations of PLWH.
Conclusion
Priorities in HIV clinical care vary substantially between patients and providers. While providers are more likely to prioritize risk behaviors such as substance use, patients desire acknowledgment from providers regarding their difficult social contexts.
Supplementary Material
Acknowledgements
We thank our patients and the Fenway Community Health and UAB Community Advisory Boards for their insights, and we thank the Madison Clinic Patient Advisory Board for guidance in domain selection and development of the measure. This work was funded by the Patient Centered Outcomes Research Institute (PCORI) SC14-1403-14081. Additional support came from the National Institute of Allergy and Infectious Diseases (NIAID) [CNICS R24 AI067039, UW CFAR NIAID Grant P30 AI027757; and UAB CFAR grant P30 AI027767].
References
- 1.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 2.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9. [DOI] [PubMed] [Google Scholar]
- 3.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20(6):64–78. [DOI] [PubMed] [Google Scholar]
- 4.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 5.Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229–39. [DOI] [PubMed] [Google Scholar]
- 6.Wittink MN, Walsh P, Yilmaz S, Mendoza M, Street RL Jr., Chapman BP, et al. Patient priorities and the doorknob phenomenon in primary care: Can technology improve disclosure of patient stressors? Patient Educ Couns. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. 2014;14:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70(4):351–79. [DOI] [PubMed] [Google Scholar]
- 9.Fredericksen RJ, Edwards TC, Merlin JS, Gibbons LE, Rao D, Batey DS, et al. Patient and provider priorities for self-reported domains of HIV clinical care. AIDS Care. 2015;27(10):1255–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health US and Human Services FDA. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crane HM, Crane PK, Tufano JT, Ralston JD, Wilson IB, Brown TD, et al. HIV Provider Documentation and Actions Following Patient Reports of At-risk Behaviors and Conditions When Identified by a Web-Based Point-of-Care Assessment. AIDS and behavior. 2017;21(11):3111–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fredericksen RJ, Crane P, Tufano J, Ralston J, Schmidt S, Brown T, et al. Integrating a web-based patient assessment into primary care for HIV-infected adults. Journal of AIDS and HIV Research. 2012;4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen RE, Rothrock NE, DeWitt EM, Spiegel B, Tucker CA, Crane HM, et al. The role of technical advances in the adoption and integration of patient-reported outcomes in clinical care. Med Care. 2015;53(2):153–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.IAP2 Spectrum of Public Participation: International Association of Public Participation; 2018. [Available from: https://cdn.ymaws.com/www.iap2.org/resource/resmgr/pillars/Spectrum_8.5×11_Print.pdf.
- 16.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Third Edition. ed. Los Angeles: SAGE; 2018. xxvii, 492 pages p. [Google Scholar]
- 17.PROMIS. Dynamic tools to measure health outcomes from the patient perspective: PROMIS (Patient Reported Outcomes Measurement Information System); 2011. [Available from: www.nihpromis.org.
- 18.Hollander M SJ. Testing for agreement between two groups of judges. Biometrika. 1978;65(2):403–11. [Google Scholar]
- 19.Dedoose version 5.0.11 [Internet]. Sociocultural Research Consultants LLC. 2014. Available from: www.dedoose.com. [Google Scholar]
- 20.Campos CJ, Turato ER. Content analysis in studies using the clinical-qualitative method: application and perspectives. Rev Lat Am Enfermagem. 2009;17(2):259–64. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. [DOI] [PubMed] [Google Scholar]
- 22.Florom-Smith AL, De Santis JP. Exploring the concept of HIV-related stigma. Nurs Forum. 2012;47(3):153–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horberg MA, Hurley LB, Silverberg MJ, Klein DB, Quesenberry CP, Mugavero MJ. Missed office visits and risk of mortality among HIV-infected subjects in a large healthcare system in the United States. AIDS patient care and STDs. 2013;27(8):442–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh S, Bradley H, Hu X, Skarbinski J, Hall HI, Lansky A, et al. Men living with diagnosed HIV who have sex with men: progress along the continuum of HIV care--United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63(38):829–33. [PMC free article] [PubMed] [Google Scholar]
- 25.Voigt I, Wrede J, Diederichs-Egidi H, Dierks ML, Junius-Walker U. Priority setting in general practice: health priorities of older patients differ from treatment priorities of their physicians. Croat Med J. 2010;51(6):483–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomson S, Doody G. Parallel paths? Patient and doctor priorities in psychiatric outpatient consultations. J Ment Health. 2010;19(5):461–9. [DOI] [PubMed] [Google Scholar]
- 27.Abbo ED, Zhang Q, Zelder M, Huang ES. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008;23(12):2058–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wittink MN, Yilmaz S, Walsh P, Chapman B, Duberstein P. Customized Care: An intervention to Improve Communication and health outcomes in multimorbidity. Contemp Clin Trials Commun. 2016;4:214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fredericksen RJ, Tufano J, Ralston J, McReynolds J, Stewart M, Lober WB, et al. Provider perceptions of the value of same-day, electronic patient-reported measures for use in clinical HIV care. AIDS Care. 2016:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.